Playlist
Show Playlist
Hide Playlist
Cardiothoracic Surgery: Esophageal Cancer
-
Slides EsophagealCancer Surgery.pdf
-
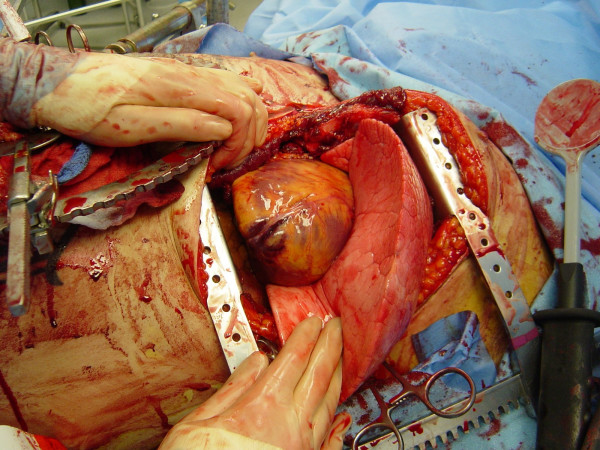
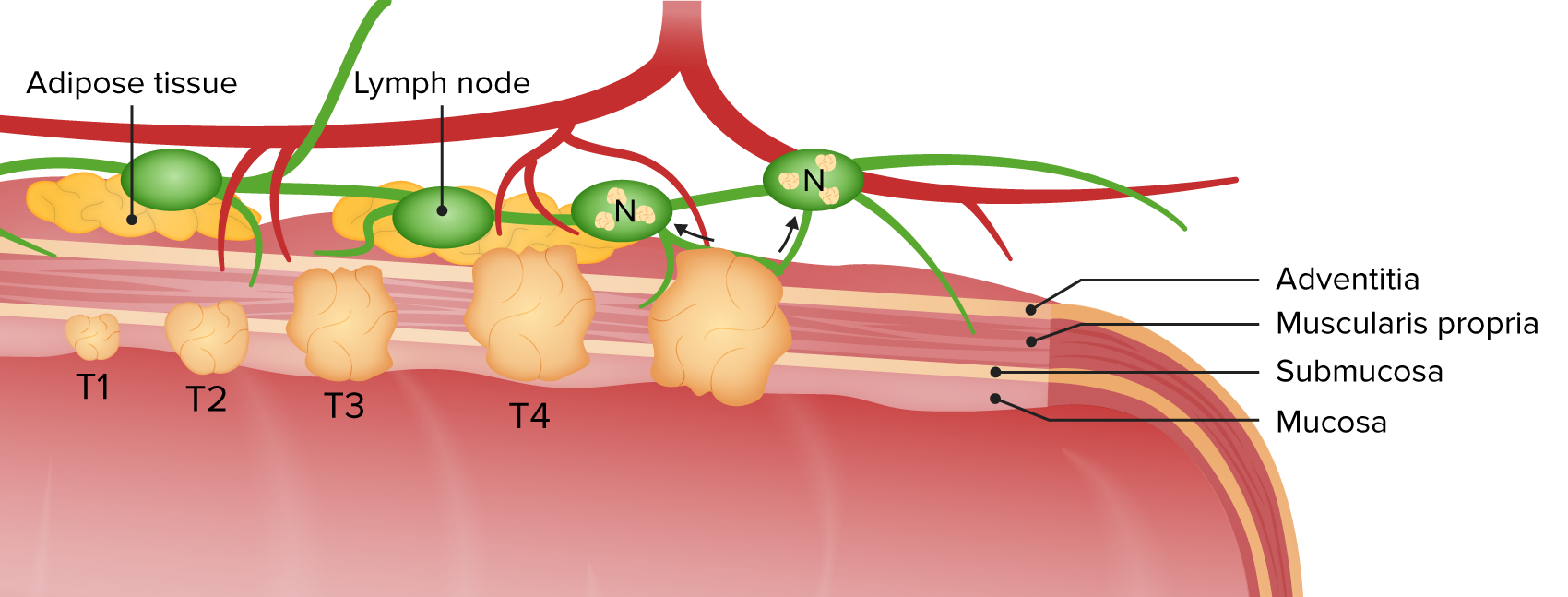
Download Lecture Overview
00:01 Thank you for joining me on this discussion of esophageal cancer in the section of cardiothoracic surgery. 00:08 Unfortunately, esophageal cancer patients don't typically do very well. 00:13 Let's start discussing the esophageal cancer types. 00:17 Squamous cell cancer of the esophagus is associated with smoking and drinking. 00:23 But don't forget that chronic reflex also can lead to esophageal cancer. 00:27 Do you remember our discussion about gastroesophageal reflux disease and Barrett's esophagus? In chronic reflux disease, patients tend to get adenocarcinomas. 00:39 What are some physical findings of esophageal cancer. 00:42 In late disease, patients can have dysphasia. 00:45 And this dysphasia may be progressive. 00:47 The reason is, as the tumor grows, the lumen of the esophagus is narrowed. 00:52 Additionally, similarly with all other patients presenting with dysphasia, inability to tolerate PO may lead to weight loss, and this can be significant. 01:02 Additionally, as you may remember, any patient with cancer also secrete tumor necrosis factor, which can cause anorexia. 01:13 Unfortunately, no routine laboratory studies is indicative of esophageal cancer. 01:19 Typically, an EGD is necessary. 01:22 An EGD is performed by a GI doctor. 01:24 And in this image, on the left, you notice there is a mass. 01:28 Distally, you see the GE junction, also known as the lower esophageal sphincter. 01:32 On the right of the screen, you note a normal esophagus. 01:36 Here, you see a retroflex view of the EGD. 01:39 This image actually shows a proximal stomach or lower esophageal sphincter cancer. 01:46 In these situations, although it may involve the esophagus, it is treated like a proximal stomach tumor. 01:52 Tumor staging is very important for esophageal cancer. 01:53 And like all oncologic processes, it's done according to the AJCC TNM system. 02:01 T for tumor, N for node status or lymph node involvement. 02:06 And M for metastasis or distant spread. 02:11 For esophageal cancer, especially because of its invasive nature, the T is very important. 02:17 Let’s discuss little bit what the tumor staging involves. 02:20 T1 disease are masses that invades the submucosa. 02:25 T2 invades the muscularis. 02:29 T3 invades the adventitia. 02:32 And lastly, T4 invades adjacent structures. 02:35 These are more advanced disease. 02:38 In this schematic, you notice that there is a dot in the middle of the esophagus. 02:43 That's actually the endoscopic ultrasound probe. 02:46 Endoscopic ultrasound probe has given us incredible images to allow us to accurately determine the actual depth of invasion. 02:56 Now, radiographic imagings, this is a barium swallow examination. 03:01 And although highlighted in the green circle is a lesion that appears to be apple core in nature, which is in fact the esophageal cancer. 03:11 This finding is rare, though, on normal routine scans unless it's late in the course of the disease and the mass is large enough to show the actual defect. 03:20 Vast majority of the time, the patients undergo EGD and potentially axial images by CAT scan. 03:27 In this image, you notice a combined anatomic CT scan as well as a PET scan. 03:34 Remember, cancers are PET-avid. 03:37 Now, remember I talked about endoscopic ultrasound. 03:40 It's incredibly important to use endoscopic ultrasound to evaluate for the depth of penetration as well as endobronchial involvement. 03:49 Remember, the esophagus sits very, very close to the trachea and main airways. 03:54 Invasion of these structures is a poor prognostic sign. 03:57 Here, you see an endotracheal ultrasound, showing invasion, highlighted by the green. 04:03 Now, before moving to surgery, if you’ve determined that the patient has advanced cancer, neoadjuvant chemo radiation therapy is actually standard protocol as first-line therapy for higher stage cancers. 04:16 Neoadjuvant means you have curative intent surgically, but the patient receives chemoradiation before surgery actually occurs. 04:27 And when the patient has had neoadjuvant therapy or if clinically appropriate, the patient undergoes an esophagectomy. 04:35 An esophagectomy is a large, morbid case. 04:39 And before surgery, you will want to make sure that your patient can tolerate the procedure from a cardiac standpoint. 04:46 Esophagectomy involves removing the section around the tumor and reconstructing the GI system. 04:52 This can involve using the stomach or the colon as a conduit. 04:57 The conduit is usually brought into the chest and a connection is made. 05:01 Unfortunately, given the number of layers of lining in the esophagus, these anastomoses or connections are prone to anastomotic leaks. 05:11 Anastomotic leaks in these patients are fraught with complications and can lead to septic shock. 05:19 Now, it's time to visit some important clinical pearls and high-yield information. 05:23 Remember, extensive metastatic workup should be completed prior to resection of the esophagus, particularly if the patient may be a candidate for neoadjuvant therapy. 05:34 Additionally, if the patient has metastatic disease, you should not offer the patient a morbid procedure such as esophagectomy. 05:42 At that point, the patient is likely a candidate either for clinical trials or palliative surgery. 05:48 And remember, the gastroesophageal junction cancers are treated like stomach cancers. 05:54 Thank you very much for joining me on this discussion of esophageal cancers.
About the Lecture
The lecture Cardiothoracic Surgery: Esophageal Cancer by Kevin Pei, MD is from the course Special Surgery. It contains the following chapters:
- Cardiothoracic Surgery: Esophageal Cance
- Diagnosis of Esophageal Cancer
- Management of Esophageal Cancer
Included Quiz Questions
Which of the following describes a T2 stage esophageal cancer?
- Tumor invades muscularis propria
- Tumor invades adventitia
- Tumor invades submucosa
- Tumor invades adjacent structures
- Tumor invades pleura, pericardium, or diaphragm
Which of the following describes a T3 stage esophageal cancer?
- Tumor invades adventitia
- Tumor invades pleura
- Tumor invades pericardium
- Tumor invades submucosa
- Tumor invades diaphragm
Which diagnostic modality is used commonly to identify the depth of an esophageal cancer?
- Endoscopic ultrasound
- Esophagram
- Esophagus-gastric-duodenoscopy
- CT scan
- Barium swallow
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |