Playlist
Show Playlist
Hide Playlist
Cardiogenic and Obstructive Shock
-
Slides Pulmonary Critical Care Respiratory Pathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
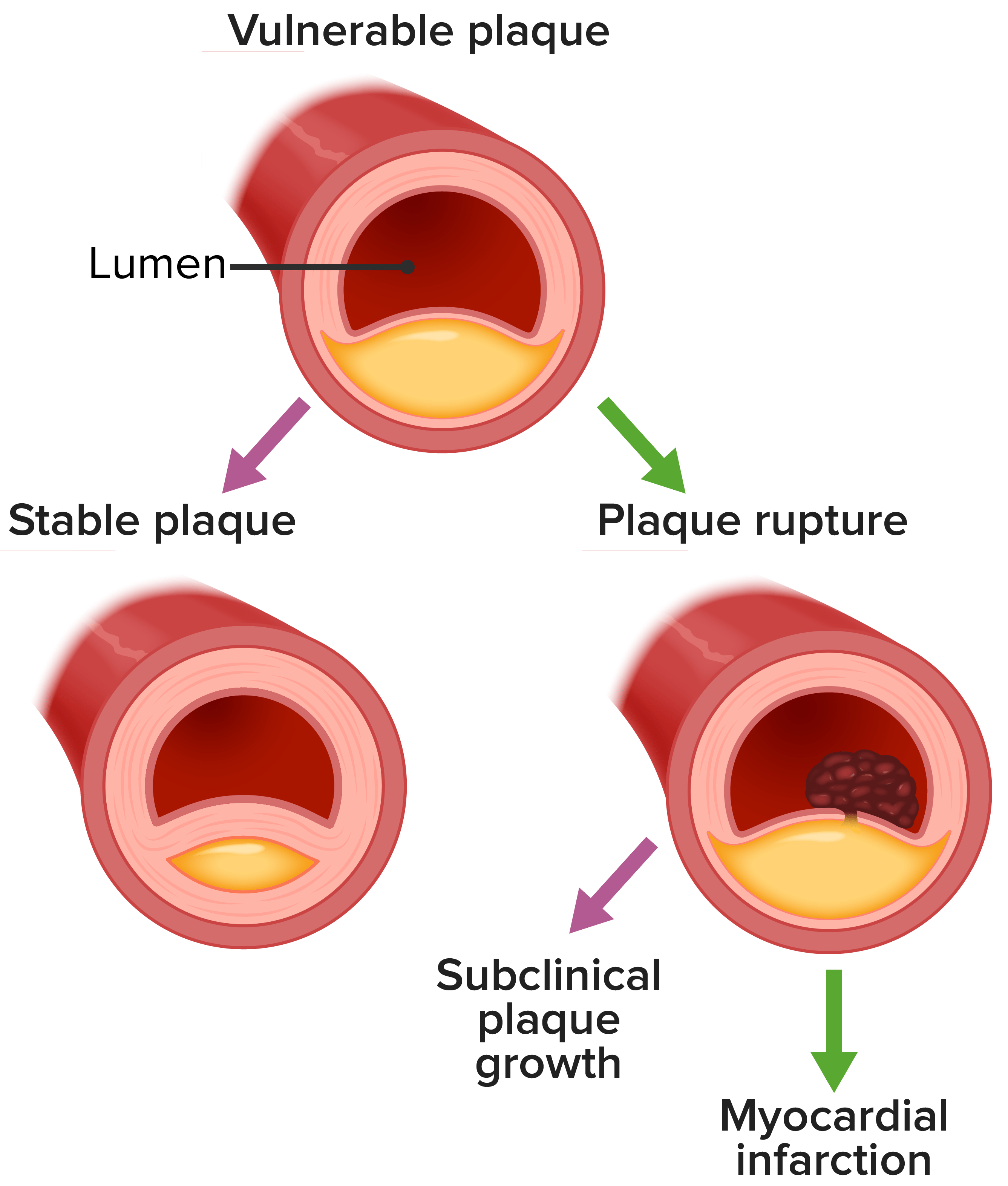
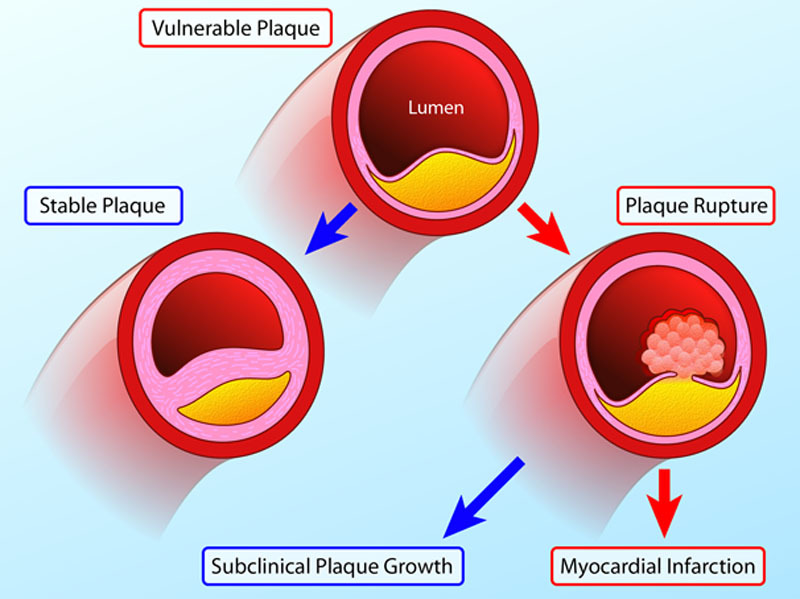
00:01 Let's take a look at the other two major shocks here. 00:02 Once again, what is now causing decreased oxygenation every tissue? We either have cardiogenic, or you have obstructive. 00:09 Let's go to each one. 00:10 And the reason that these are put in the same row is because many of the features are going to be comparable. 00:18 And there are certain features that are absolutely distinct. 00:21 So, let's first go through cardiogenic. 00:24 Obviously, the causes are going to be different, right? If it's cardiogenic, what happened? Oh, my goodness, you or the patient has suffered a myocardial infarction. 00:33 If there's a myocardial infarction, one of the post MI complications include your CHF and acute congestive heart failure. 00:41 You would have then a decreased in cardiac output You have a decrease in cardiac output, what then happens to yout tissue? That's improperly being oxygenated. 00:49 Okay, what other issues do we have here? Acute MI, valvular dysfunction, arrhythmias. 00:55 See if your heart stops, then where do you begin here? It's on hemorrhaging, a decreased cardiac output. 01:01 And where does some of this fluid go? Oh, yeah. It backs up into maybe the pulmonary. 01:08 Alright, pulmonary edema. 01:10 If it's cardiogenic, it will be transiting maybe if it's bad enough, may result in alveolar hemorrhage in company, but decreased cardiac output. 01:18 Here, once again, what happens to your stretch? Decreased. 01:21 What do you want from your medulla? You want sympathetic. 01:26 Okay, so this is example number two, where it's a shock, we have increased in your sympathetic and so therefore, I want you to now move into your diagnosis here. 01:37 And you would expect to find cold and clammy. 01:39 But that's not specific, because it's sympathetic. So let's go into diagnosis for each of the shocks, your cardiogenic obstructive, before we move on. 01:49 Let's just make sure that we're clear about obstructive, and why the heart might not be properly or the cardiovascular and the pulmonary system are not properly functioning as they should. 02:02 And obstructive cardiac tamponade. 02:04 What happened here? Oh, maybe the patient had a myocardial infarction, oh, maybe there was a scar formation, but was weakened, so resulting in ventricular aneurysm, and maybe there was ventricle wall rupture. 02:17 And so therefore, how quickly is this pericardial cavity being filled up? Way too quick. 02:22 What do we have here? Cardiac tamponade. 02:25 What is this? Obstructive type. 02:27 And then we have pulmonary embolism. 02:29 Pomi. embolism would also be considered an obstructive type. 02:33 Let's talk about the diagnosis. 02:34 So apart from the cold and clammy because of why? Sympathetic. 02:39 Let's talk about congestive heart failure In CHF, well, what's that heart sound that you're going to create when you have a very large left ventricle? And so now at this point, as soon as you have diastole, early on, this mitral valve opens and blood rushes into left ventricle creating... 02:56 S3. 02:58 Whereas S3, in relation to S1,S2 Good after S2. 03:04 So, S2 would be the closure of the aortic and, right after closure, you're opening up your mitral valve and you're going to create massive flow of blood from left atrium and to left ventricle creating your S3 gallop. 03:18 Hopefully that's clear. 03:20 Next, well, say that your heart is not functioning properly, you're going to backup, where? Lungs. 03:27 One side or two sides? Both sides, with what? Good pulmonary edema. 03:34 Number one, if it's the right side that affected then you're going to have what's this right here when your intrajugular vein can be seen to be pulsating? You should never normally be able to see the internal jugular vein. 03:47 But if you find it to be pulsating as your positive JVP, jugular venous pulse. 03:53 Are we clear? Heart issues? cardiogenic. 03:57 Okay, what about obstructive and company? And here because it's obstructive well, if your pericardial cavity is being filled up, you cannot properly hear your heart sounds, so therefore, it'll be muffled. 04:10 Okay, now, my problem is this. 04:12 Now, don't memorize this. Work with me. 04:14 The heart isn't working properly. 04:17 And if it's congestive heart failure, which is the best example to give you at this point, and then you know, the heart is filled with blood, volume overload. 04:26 And so therefore, there's more blood and your heart isn't there and CHF. 04:30 And so therefore, this has been referred to as being preload. 04:34 You expect your pulmonary capillary wedge pressure or your central venous pressure to be increased. 04:38 And that's what you're seeing here. 04:42 Next, well here, if your heart's not working either obstructive or cardiogenic, you can expect your cardiac output did the decreased severely. 04:50 And what kind of symptoms are you finding here? Or type of signs cold and clammy, right? Sympathetic nervous system. 04:58 What does that then doing to your systemic vascular resistance and arterioles. 05:02 Good, basic construction increase in TPR. 05:06 Now, what treatment obviously be different? If it's congestive heart failure and you're trying to reestablish a pumping motion, then obviously you want to use a positive inotropic agent, maybe something like dobutamine beta-1 agonist. 05:19 And if you want to try to take care of that edema, you're thinking about, good, furosemide, a diuretic. 05:27 In obstructive shock caused by cardiac tamponade, the diagnosis is usually made by ultrasound and supported by hearing muffled heart sounds, because the pericardial fluid is blocking the passage of sound from the heart to the chest wall. 05:40 When tension pneumothorax is causing the obstruction, the trachea will be deviated away from the side with the pneumothorax. 05:47 A large pulmonary embolism will have a respiratory consequence of hypoxia, and a hemodynamic consequence of hypotension. 05:55 The patient will have dyspnea and pleuritic chest pain. 05:58 All of these three causes will result in an increase in the CVP which is clinically seen as an elevated jugular pressure and the preload to the heart will be decreased because the venous return path back to the heart is obstructed. 06:11 Naturally then the cardiac output will be decreased and the systemic vascular resistance will be increased by sympathetic hyperactivity. 06:19 The treatment for all causes of obstructive shock is immediate relief of the obstruction.
About the Lecture
The lecture Cardiogenic and Obstructive Shock by Carlo Raj, MD is from the course Pulmonary Critical Care.
Included Quiz Questions
What is the cranial nerve responsible for transmitting the stimulus which increases sympathetic outflow in response to decreased baroreceptor firing?
- Glossopharyngeal nerve
- Recurrent laryngeal nerve
- Trigeminal nerve
- Hypoglossal nerve
- Vestibulocochlear nerve
Which of the following physiologic changes would you expect to see in a patient with hypovolemic shock?
- Increased sympathetic outflow
- Increased baroreceptor firing
- Decreased afterload
- Increased preload
- Increased cardiac output
Which of the following scenarios would result in hypovolemic shock in the setting of increased total body water?
- Patient with severe pancreatitis and massive ascites
- Patient with massive blood loss from a gunshot wound
- Patient with congestive heart failure
- A patient who is severely dehydrated
- Patient with uterine hemorrhaging after childbirth
Which of the following IV fluids is typically used in the management of hypovolemic shock?
- 0.9% normal saline
- 0.45% normal saline
- Fresh frozen plasma
- Albumin
- D5W
Which of the following measurements is indicative of a failure of the left ventricular output and is used as a rough measurement of preload?
- Pulmonary capillary wedge pressure
- Central venous pressure
- Mixed venous O₂
- Diastolic blood pressure
- Total peripheral resistance
Which of the following signs would you expect in a patient with cardiogenic shock?
- S3 gallop
- Warm skin
- Muffled heart sounds
- Unilateral crackles
- Anhydrosis
A patient with suspected shock has decreased preload, decreased cardiac output, increased total, and peripheral vascular resistance. What is the most likely etiology?
- Severe volume depletion
- Sepsis
- Congestive heart failure
- Acute Myocardial infarction
- Arrhythmia
Which of the following medications is most suitable in the management of a patient with cardiogenic shock induced pulmonary edema?
- Furosemide
- Angiotensin II antagonist
- Angiotensin receptor blocker
- Beta blocker
- Dopamine
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
his teaching style is abrasive. Lecturio couldn't find a better lecturer?
Thank you very much for this very clear shock lecture !