Playlist
Show Playlist
Hide Playlist
Cardiac Case: 77-year-old Man with Shortness of Breath and Palpitations
-
Cardiac Case 77-year-old Man with Shortness of Breath and Palpitations.pdf
-
Reference List Cardiology.pdf
-
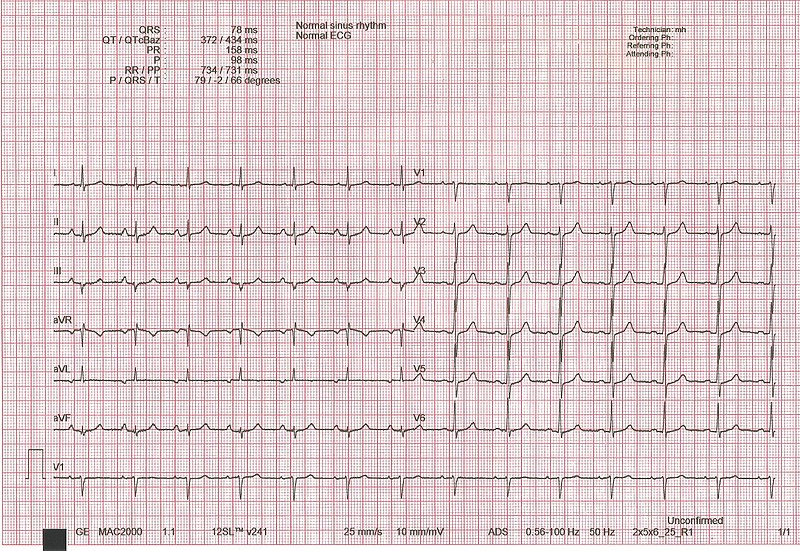
Download Lecture Overview
00:00 A 77-year-old man comes to the emergency room complaining of shortness of breath and feeling his heart bouncing all over the place. 00:09 In the emergency room he’s seen and it’s noted that his heart rate is a 144 per minute, quite abnormal. 00:17 His blood pressure is slightly elevated at 150/78 and the pulse is very irregular. 00:23 So instead of the pulse being pum pum pum pum, the pulse is this -- you can here it’s very fast and very irregular. 00:36 So what’s critical in this history? First of all he has dyspnea, secondly he has a tachycardia that’s very abnormal in its rhythm because it’s very irregular and he also of course has a little bit of hypertension and of course the critical point is the irregular pulse so we obtained an electrocardiogram. 00:56 Please look at the electrocardiogram and tell me what is going on here. 01:07 Well, I hope you noticed that this is a markedly irregular heart rate with no clear P waves otherwise the QRSs are normal so it’s not a myocardial infarct and this is atrial fibrillation. 01:23 And you can see here with the normal ECG underneath P wave followed by QRS and look at atrial fibrillation above, totally irregular so instead of pum pum pum pum, you're seeing -- completely random occurrences of the QRSs and the ventricular contractions. 01:49 The EKG is otherwise normal but the QRSs do not show a myocardial infarct and of course when your heart rate goes at 140 to a 150 the filling pressures in the heart go up transmitted back to the lung and make you short of breath. 02:04 So the first treatment is to give him a beta blocker, metoprolol which will slow the heart rate, slow the ventricular rate. 02:12 He's admitted to the coronary care unit and overnight his heart rhythm stabilizes, he could go back to sinus rhythm or he may have slowed atrial fib and he’s discharged with prescriptions with metoprolol to prevent it if he went back to sinus rhythm or to keep the rate slow and then anti-coagulants because of the high risks for a blood clot forming in the left atrium that can get out and cause a stroke. 02:39 If he were still in atrial fib but slow we would then want to see him in a few weeks after he’d been anticoagulated for a few weeks to makes sure any clots in the left atrium were dissolved and he would then undergo electrical cardioversion, it turned out in this case, as often happens, giving him some metoprolol usually given intravenously during the night converts him back to sinus rhythm and of course he needs an outpatient appointment with a cardiologist for follow up, he needs to continue on his anticoagulation cause once having atrial fib he’s at high risk to do it again even when he tells you, "Oh, I never feel it again." Maybe it occurs during sleep, he can still get a blood clot in the left atrium and still get a stroke. 03:23 He needs to continue he’s anticoagulation and we almost always continue he’s beta blocker metoprolol. 03:30 What’s very important here is that if metoprolol didn’t control his atrial fib we have other drugs which can be administered to help keep the patient in sinus rhythm, regular rhythm, and if that fails the cardiac electrophysiologist or the cardiac electricians can actually consider an ablation procedure which markedly increases the likelihood that he would remain in sinus rhythm.
About the Lecture
The lecture Cardiac Case: 77-year-old Man with Shortness of Breath and Palpitations by Joseph Alpert, MD is from the course Cardiovascular Cases.
Included Quiz Questions
Which of the following best describes the ECG findings in atrial fibrillation?
- No discernable P waves with irregularly irregular QRS complexes
- Irregular QRS complexes with regular P waves
- Increasing PR intervals with a drop of every 4th QRS complex
- Regular QRS complexes independent from regular P waves
- Varying R-R intervals with high amplitude P waves
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Alpert provides such a clear & concise overview about high-yield diagnosis & management strategies! Thank you for creating this very helpful lecture series!