Playlist
Show Playlist
Hide Playlist
Candidiasis on Darker Skin: Epidemiology and Etiology
-
Slides Candidiasis on Darker Skin Epidemiology and Etiology.pdf
-
Download Lecture Overview
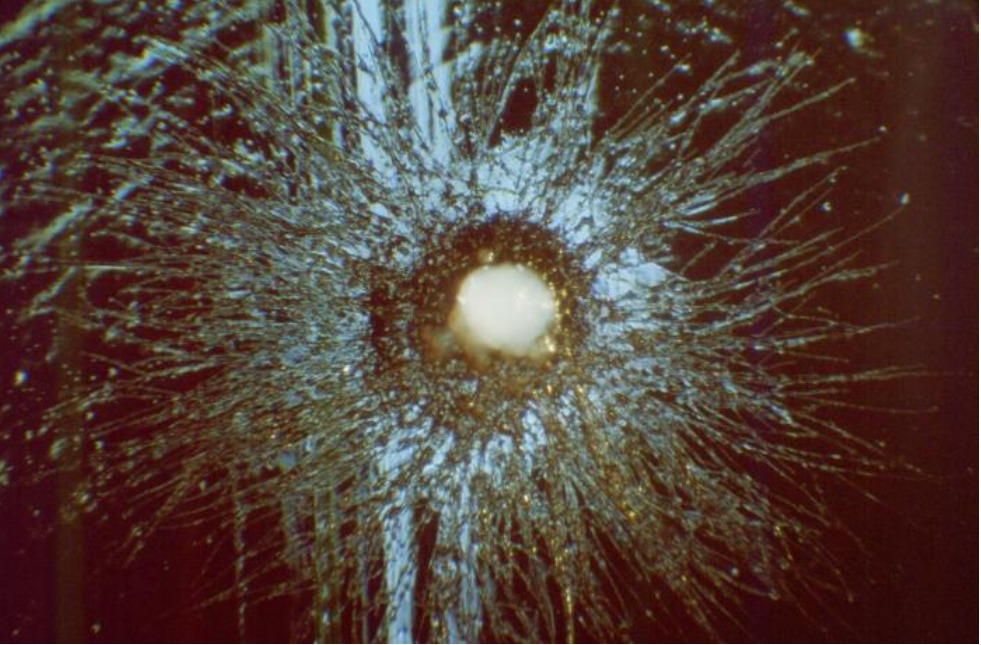
00:01 Welcome to our lecture on candidiasis. 00:05 Candidiasis is an infection caused by the yeast Candida albicans. 00:11 Or it could be due to other Candida species. 00:14 It is also known as candidosis or moniliasis. 00:19 It's a common cause of intertrigo in older adults and diabetic patients. 00:24 The prevalence of Candida infection is on the rise, mainly due to inappropriate antibiotic use and high sugar diets. 00:34 The predisposing factors of candidiasis include warm climate, use of broad spectrum antibiotics for a long time, usage of contraceptive pills with high estrogen content, as well as endocrine conditions, for example, diabetes and Cushing's disease. 00:54 Malignancies, chemotherapy and immunocompromised patients are also predisposed to candidiasis. 01:03 And the last one is underlying skin disease, for example atopic dermatitis. 01:12 Candidiasis is caused commonly by Candida albicans, which is a yeast. Non albicans species can also cause candidiasis. 01:27 We are going to cover the most common clinical presentations of Candida. 01:31 Firstly we'll talk about Candida intertrigo. 01:34 Chronic paronychia. Candida onychomycosis, generalized cutaneous candidiasis, oral candidiasis, vulvovaginal candidiasis and Candida balanitis. 01:48 So let's talk about Candidal intertrigo. 01:51 A patient will present with erythematous and macerated plaques with peripheral scaling. 01:57 It's important to note that in Candida intertrigo, you may see satellite lesions, or these can present with pustules or papules around the main lesion. 02:10 So this is an important clue that one is ones dealing with Candida intertrigo. 02:16 The usual sites are the armpits and groin, skin folds, and the web spaces between fingers or toes. 02:24 The differential diagnosis is dermatitis, which can be irritant or allergic. 02:32 The second topic is chronic paronychia or nail fold infection. 02:38 Here, one gets proximal nail fold swelling, which presents with dusky erythema and dystrophic nails, particularly in skin of color. 02:48 The differential for this is acute bacterial paronychia, which could be due to staff or strep infection. 02:58 Onychomycosis is nail plate infection. 03:01 Here you get dystrophic and discolored nail with proximal nail fold swelling. 03:07 The differential is tinea unguium or squamous cell carcinoma. 03:15 Now looking at generalized cutaneous candidiasis , this usually presents in children who usually are very ill. 03:23 One gets diffuse eruption over the trunk, thorax and extremities, and the rash begins as individual vesicles that spread into larger confluent areas. 03:34 How about oral candidiasis? Pseudomembranous candidiasis is the most common type and it presents with white plaques on gums, tongue and inside the mouth. 03:48 It can be peeled off, leaving raw areas. 03:53 This is a nice way of differentiating between oral candida and conditions like oral leukoplakia. Still on oral candidiasis. 04:07 Another type of oral candidiasis is due to ill-fitting dentures, which predispose to angular colitis. 04:18 The other type is erythematous candidiasis. 04:22 There's also hyperplastic Candidiasis and lastly, chronic atrophic candidiasis. 04:32 That sums up all the clinical manifestations of oral candidiasis. 04:41 What about vulvovaginal candidiasis? It affects 75% of women at least once in a lifetime, and they present with white curd like, almost looking like sour milk or yogurt vaginal discharge, is usually a burning sensation in the vagina and vulva, and itchy rash on the vulva and surrounding skin may also be a presenting symptom. 05:07 Looking at Candida balanitis, this presents in men with blotchy erythema with small red satellite papules or dry, dull red areas. 05:21 The complications of Candida in immunocompromised patients or patients with advanced HIV or ICU patients are listed on the slide. 05:34 The diagnosis is based on physical examination as well as skin swab or scraping for fungal microscopy and culture. 05:44 And one will see pseudohyphae on a potassium hydroxide wet slide. 05:52 The skin biopsy is usually not necessary. 05:55 However, in cases of difficulty it can be undertaken. 06:03 Management of Candida for limited disease includes the use of topical antifungal agents as listed on the slide. 06:13 Now we're going to focus on the treatment of extensive or refractory disease. 06:18 We use the following systemic antifungals: fluconazole and itraconazole. 06:25 The dosages and duration of treatment will depend on the clinical manifestations and comorbidities of the patient.
About the Lecture
The lecture Candidiasis on Darker Skin: Epidemiology and Etiology by Ncoza Dlova is from the course Fungal Skin Infections in Patients with Darker Skin.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |