Playlist
Show Playlist
Hide Playlist
Calcium Homeostasis in Children
-
Slides HypocalcemiaandHypercalcemia Pediatrics.pdf
-
Download Lecture Overview
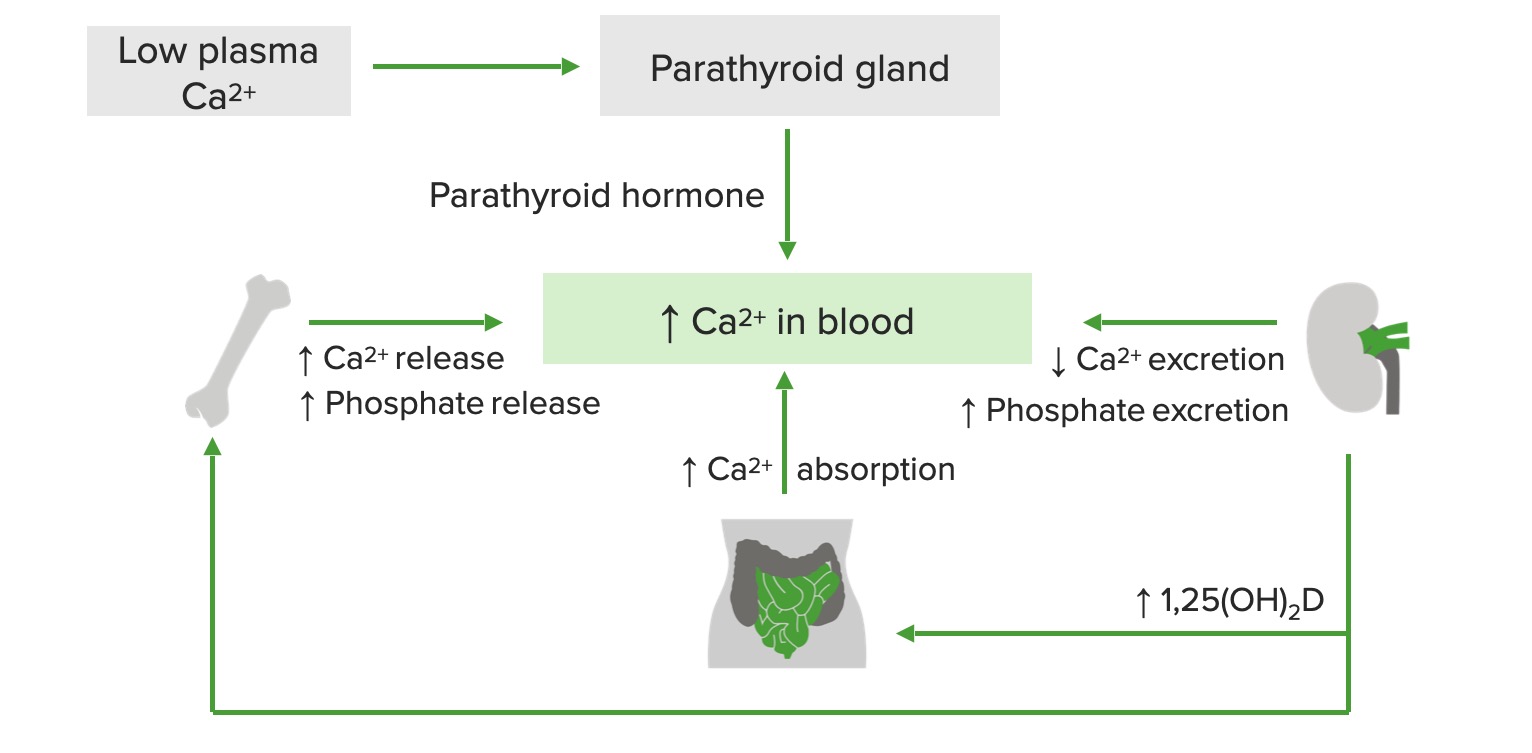
00:02 In this lecture we will review calcium homeostasis disorders such as hypocalcemia and hypercalcemia. 00:10 So in order to think about this let's try and remember the basic fundamental control mechanism of our calcium levels in our blood. 00:20 Parathyroid hormone is controlling this and the parathyroid hormone receptor. 00:25 We have vitamin D controlling this and we have a calcium-sensing receptor and these are all things that are helping us to control our levels. 00:34 On this slide you can see a general overview of how we control calcium levels. 00:39 Let's go through this bit by bit. 00:41 Remember vitamin D in general is absorb from the skin through light exposure or in the diets. 00:49 In patients with darker skin there is less effective absorption of light and conversion of vitamin D in our blood. 00:58 Generally, this vitamin D level is then travels to the liver where this metabolize into 25-hydroxy vitamin D. 01:07 It then goes from the liver to the kidney and the kidney turns this in to 1,25-Dihydroxy vitamin D which is the active metabolite of vitamin D. 01:18 The kidney can dispose of 1,25-hydroxy vitamin D. 01:24 So it's a bit difficult to overdose on that particular formulation. 01:28 The 1,25-hydroxy vitamin D then goes to the bone where it promotes the resorption of calcium and phosphate from the bone and into the blood. 01:39 Likewise, the 1,25-hydroxy vitamin D, proceeds to the intestine where it promotes absorption of calcium and phosphate from ingested contents. 01:52 Also, remember that PTH has an effect of increasing 1,25-hydroxy vitamin D conversion in the kidney and promotes resorption via the osteoclast. 02:07 And remember there is a negative feedback loop where 1,25-hydroxy vitamin D is actually inhibiting the activity of parathyroid hormone. 02:18 Basically all of these activities promote the production of calcium and phosphorus in the blood and those two metabolites go on to be important in both bone mineralization, a variety of metabolic functions and neuromuscular functions, especially the calcium. 02:38 There are a few things that can inhibit calcium in the blood outside of the system, one is high phosphate levels. 02:46 High phosphate levels reduce serum calcium through simple binding of the two elements together and deposition in tissues. 02:54 Likewise, a low magnesium will inhibit the production of calcium because magnesium is a cofactor for the function of the parathyroid hormone. 03:04 So ionized calcium can be measured, probably we should stop getting calcium levels because that will go up and down depending on binding to albumin. 03:16 But ionized calcium can be measured and this is the true amount of calcium in the blood. 03:21 Total calcium needs to be corrected if there is low albumin, because some albumin is binding some of that calcium and thus the calcium levels maybe off. 03:32 In fact we're going to adjust that using a formula. 03:35 For every gram that your albumin is low you should actually correct your calcium up by 0.8.
About the Lecture
The lecture Calcium Homeostasis in Children by Brian Alverson, MD is from the course Pediatric Endocrinology.
Included Quiz Questions
Which of the following electrolyte imbalances induces low serum calcium levels?
- Hypomagnesemia
- Hypophosphatemia
- Hyperkalemia
- Hyponatremia
- Hypochloremia
Regarding calcium homeostasis, which of the following statements is FALSE?
- High levels of PTH decrease osteoclast activity.
- Parathyroid hormone and vitamin D mainly control the calcium levels in the body.
- Milk and fish are good sources of vitamin D.
- 1, 25(OH)₂D inhibits the activity of PTH by negative feedback.
- Calcium must be very tightly maintained to keep action potentials working across nerve cells.
Where does the conversion of 25(OH)D to 1, 25(OH)₂D occur?
- Kidney
- Lung
- Skin
- Gut
- Liver
A child with suspected liver disease shows the following lab values: albumin: 1.4 g/dL (normal range: 3.4 - 5.4 g/dL), total calcium: 7.5 mg/dL. What is the value of the corrected calcium?
- 9.1 mg/dl
- 8 mg/dl
- 7.5 mg/dl
- 8.7 mg/dl
- 8.3 mg/dl
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |