Playlist
Show Playlist
Hide Playlist
Bronchiectasis: Pathogenesis
-
Slides ObstructiveLungDisease Bronchiectasis RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
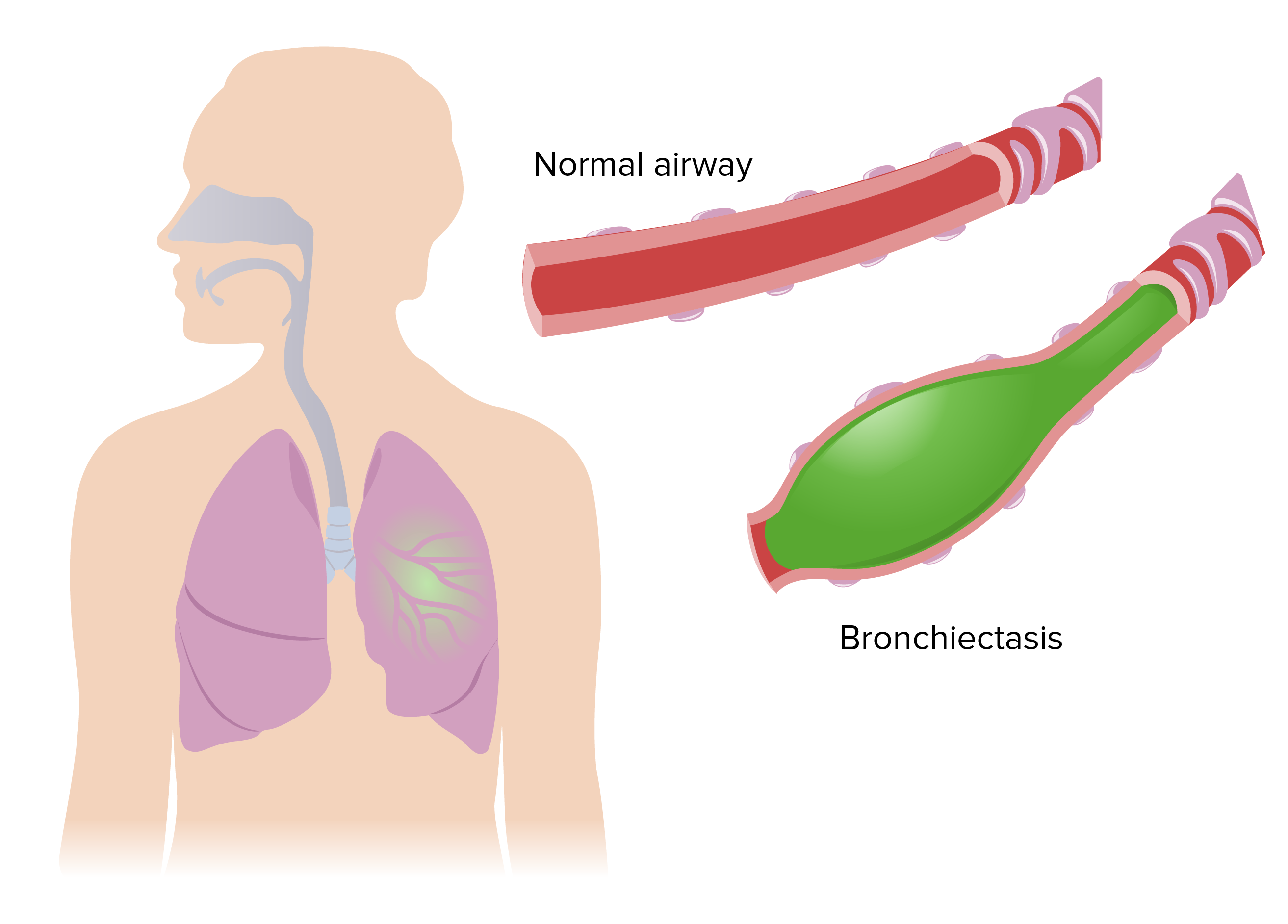
Download Lecture Overview
00:01 Finally come to our last little specific disease of obstructive. 00:06 However, I do need you to keep the topics that are upcoming, as more or less a continuum of things that we've looked at. 00:15 With obstructive, three major ones that you have to keep in mind, and we discussed this as an overview. 00:21 So, we're concluding our discussion of obstructive, is your Asthma, Chronic Bronchitis, and your Emphysema. 00:28 What we'll take a look at here, we'll begin by looking at is Bronchiectasis. 00:32 First, dissect the name bronchi and ectasis, and this will then give you your definition or your presentation of a dilated bronchi. 00:44 A persistent inflammation of the airways can cause an abnormal dilatation of the bronchi, by definition, that is what you have your bronchiectasis, but interesting enough, could this be then be associated with other issues, and other COPD differentials that we've seen where the airways are becoming inflamed? Of course, such as chronic bronchitis with mucus production. 01:09 Now, this is, the prime operative word here is, secondary to the impaired clearance of the airways which cause a vicious cycle of infection, inflammation, obstruction. 01:23 Infection, inflammation, obstruction. 01:26 What does this mean? So, say that infection has now kicked in. 01:30 If infection has kicked in, you can then only imagine that the type of breath that this individual's going to have will be rather foul-smelling or even the sputum more importantly that you end up gathering is going to be foul smelling, isn't it? Bronchiectasis. Inflammation and obstruction. 01:50 Well, say that there's enough obstruction as such that's taking place, are you then going to result in bronchiolitis obliterans? Sure, with the development of fibrosis. 02:00 Keep all that in mind as we move forward here through the discussion of bronchiectasis. 02:06 On your left, is your normal bronchus. 02:08 What we have here is the wall of the bronchi, the mucus glands, the cilia, the air passage and the mucus itself. 02:17 You find the mucus to be quite, quite minimal and you find that the airway passage is quite open, so that you allow for air to move in and out. 02:25 Whereas with the pathology of bronchiectasis, you end finding quite a bit of increase in mucus. 02:31 Now, would you please take a look at the lumen that you see there, which is light pink and quite warped. 02:37 And so, therefore, the lumen here of the airway is extremely small, you can only imagine that you're having difficulty with properly getting out your air. 02:47 Welcome to a type of obstruction. Welcome to bronchiectasis. 02:51 Tell me about the cilia, the cilia gets smothered, and so therefore your mucociliary clearance then is not functioning properly. 03:01 Now, be very careful, before I move on, I wish to be very clear with you about chronic bronchitis in which you might find here bronchiectasis. 03:08 In chronic bronchitis, it's definition that you're paying attention to. 03:12 Chronic Bronchitis is define as at least three months of symptoms each year for the past two consecutive years. 03:19 The months themselves do not need to be consecutive. 03:22 And the fact that we talked about the different histologic changes, that are taking place in the upper airways, such as squamous metaplasia and mucus production. 03:29 And the fact that we'll look at Reid index, whereas here, we have issues with mucus, but you don't have the same type of definition and coughing, but you might have, well, we'll take a look at the laboratory investigations. 03:42 This is advanced severe bronchiectasis, with segmental dilation and scarred airway walls. 03:48 Bronchiectasis usually affects the lower lobes bilaterallly, as shown here. 03:54 Alright, now here, if you take a look at the CT of bronchiectasis, we'll find that the, for sure the bronchi are dilated. 04:03 You see a picture like this and you don't find the definition of chronic bronchitis, you'd choose bronchiectasis. And hopefully they've given you a little bit more, in terms of a secondary type of issue, such as infection then resulting in dilation. 04:19 With bronchiectasis, let's now take a look at the all-important clinical manifestations, what I like for you to keep in mind are the differentials of chronic bronchitis and also asthma. 04:29 Patients typically present with episodes of, well, dyspnea, nonspecific, fever, once again you could find that in a few issues. 04:38 Now, chronic productive cough and a frequent respiratory infections. 04:43 Those are two that you're definitely paying attention to. 04:46 A lot more of these respiratory infections, whereas chronic bronchitis, more associated with smoking irritation. 04:52 With chronic bronchitis, chronic bronchitis is define as at least three months of symptoms each year for the past two consecutive years. 05:00 The months themselves do not need to be consecutive. 05:02 But careful because this patient here in terms of symptoms and the way that he or she might be expressing his or her symptoms might seem like it's chronic bronchitis, infection which you're paying attention to. 05:15 If there's enough damage, with the coughing then there might be hemoptysis, and there's blood that's actually coming from your respiratory tree, might then seem a little foamy, right? That's because you have involvement, and, well, composed of a little bit of sputum perhaps, right? Whereas if it was hemoptysis and it was clear blood, without foam then that would be like emesis originating from your GI system. 05:42 Now, giving your patient, sputum cup might then help them to quantify how much sputum that they're producing a day. 05:49 And that's useful for you and then as far as sputum is concerned, you're worried about infection.
About the Lecture
The lecture Bronchiectasis: Pathogenesis by Carlo Raj, MD is from the course Obstructive Lung Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is the most appropriate statement regarding bronchiectasis?
- This is secondary to the impaired clearance of the airways that causes a vicious cycle of infection, inflammation, and obstruction.
- It is a strong predisposing factor to carcinoma.
- This is secondary to the impaired clearance of the interstitium that causes a vicious cycle of infection, inflammation, and obstruction.
- This is secondary to the impaired clearance of the airways that causes a vicious cycle of metastatic inflammation.
- This is secondary to the impaired clearance of the pulmonary vasculature that causes a vicious cycle of infection, inflammation, and obstruction.
Which of the following is not true regarding the pathological changes that occur in bronchiectasis?
- Lung hepatization
- Cilia loss
- Increased mucus production
- Bronchial wall destruction
- Increased lumen size
Which of the following is an unlikely presentation in bronchiectasis?
- Hypothermia
- Shortness of breath
- Chronic productive cough
- Fever
- Frequent respiratory infections
Customer reviews
2,6 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
2 |
| 1 Star |
|
4 |
9 customer reviews without text
9 user review without text