Playlist
Show Playlist
Hide Playlist
Bronchiectasis: Overview and Causes
-
Slides 05 MajorAirwaysObstructionBronchiectasis RespiratoryAdvanced.pdf
-
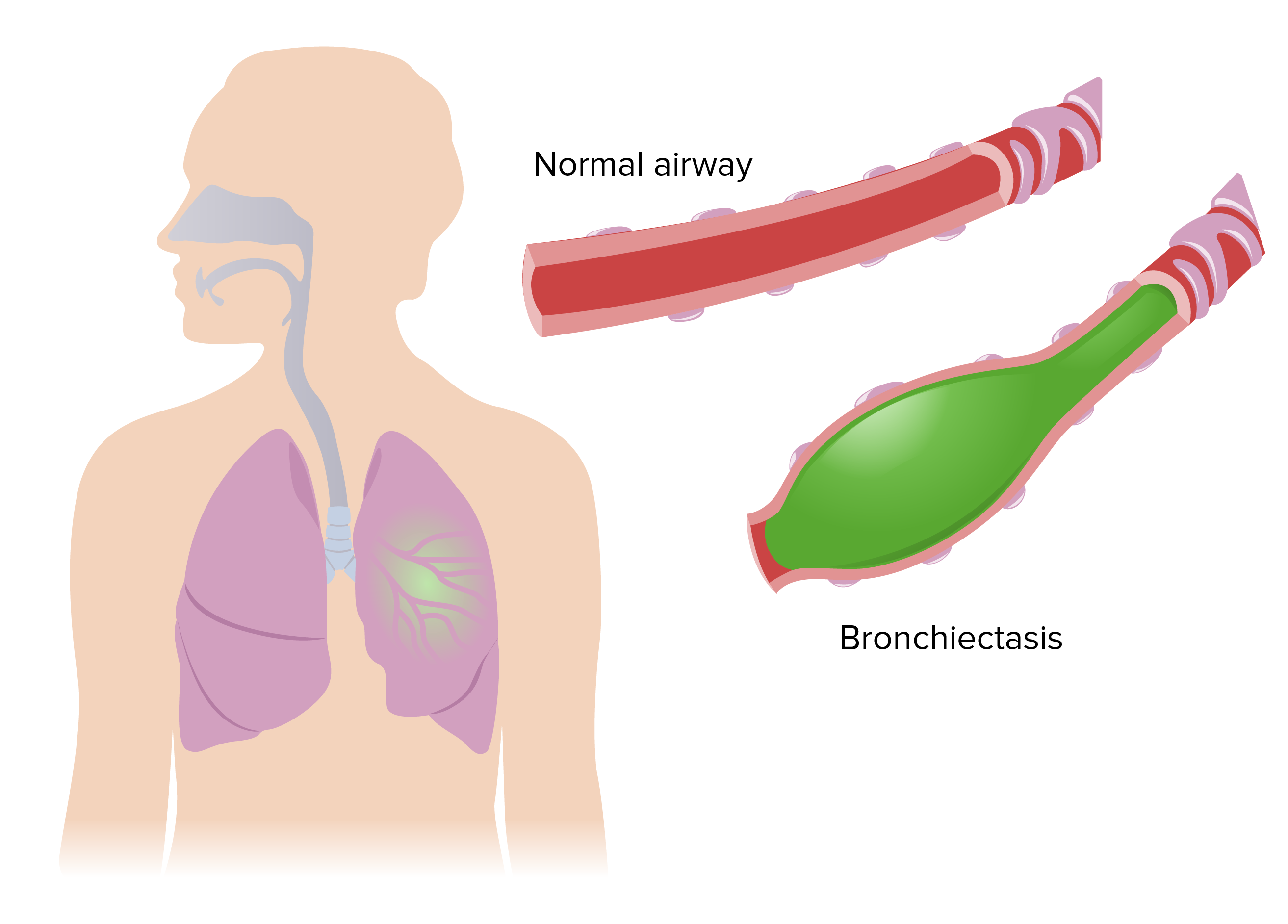
Download Lecture Overview
00:01 So moving on, I'm now going to talk about bronchiectasis. 00:04 Now this is a surprisingly common problem. Bronchiectasis is often considered as the disease of the 19th century or countries where don’t have ready access to medical care or antibiotics for their respiratory problems. But actually, the data suggests there are about a 100,000 in the UK at the moment who have bronchiectasis. What is bronchiectasis? Well it's abnormal chronic dilatation of bronchi and that could be localized or it could be diffused. It's an anatomical diagnosis and therefore is made by doing a CT scan. So it's the visual appearance of the scan that tells you whether the patient has bronchiectasis or not. What's the pathology? The pathology is a combination of neutrophilic airways inflammation, fibrosis of the small airways of obliterative bronchiolitis. So that sounds confusing. The large airways are dilated, that's the definition of bronchiectasis, but the airways distal to that, the bronchioles, the smaller airways, what happens to them in bronchiectasis, is actually that they become tighter, you get small airways obstruction. And that's one of the common forms of irreversible airways obstruction. And the underlying pathology is that the chronic bacterial infection of the dilated airway. The dilated airway is unable to clear the bacteria and therefore is a chronic infection of that site and that drives the symptoms and how the patient presents. It tends to be a chronic disease, but it is often associated with very frequent exacerbations. So bronchiectasis affects any age, although the peak age of diagnosis is around 50 and women are more likely to have the disease than men, although it's only a slight sex preference. And the reason why it presents with any age is that there are multiple different causes of bronchiectasis, it's the end result of a whole range of different problems. Actually, 40% or more of patients where you are not sure why the patient has developed bronchiectasis and this tends to be the middle-aged women who are presenting with the symptoms later in life. One of the biggest causes is post-infective. 02:10 An infection often as a child such as measles, whooping cough, tuberculosis or a previous pneumonia causes the bronchiole wall damage and allows bronchiectasis to become a clinical problem later in life. And there are many other inflammatory causes such as allergic bronchopulmonary aspergillosis, rheumatoid arthritis, COPD, as mentioned in one of the previous lectures is actually complicated by bronchiectasis with severe disease. 02:35 An important catch here are those patients who have immune defects and that's normally in a deficiency of the antibodies, IgG. But, there are a range of other immune defects that are sometimes associated with bronchiectasis. One of the common immune defects that you need to consider are mucocilary problems. What I mean by that are diseases that impair the mucocilary clearance. Now the cilia are the protein hair like projections from the respiratory epithelium that are required for moving mucus up the bronchi and clearing out any stuff that impacts in the bronchial tree and tipping it down into the back of the larynx. Now that is one main method by which we keep our lungs clear of infection, but if there are any problems of that mucocilary clearance, then you might develop bronchiectasis, and the classic example of that is cystic fibrosis, and the other classic example is ciliary dyskinesia. And there are a whole range of very rare causes or relatively rare causes of bronchiectasis. If you have localized obstruction, and that will cause distal bronchiectasis, and so on and so on. So, the basic pathogenesis of bronchiectasis is you either have an immune defect, the classic examples being cystic fibrosis or IgG deficiency or local bronchial obstruction that allows the bacteria to colonize and infect the bronchi or we have airway inflammation which damages the bronchi and again allows the bacteria in and infect the bronchi and causes of airway inflammation that do that is after infection, allergic bronchopulmonary aspergillosis, rheumatoid arthritis, COPD. Once you have colonization and infection of the bronchi, that in itself would drive an inflammatory response and that inflammatory response will cause further damage to the bronchi. So it's likely you're going to set up a positive feedback circuit, a vicious cycle of infection, inflammation, further damage allows the bacteria to stay within the bronchi even more because of the impairment of host defenses and so on and so on, and the bacteria themselves can also drive damage through the products that they produce. Just to discuss mucociliary clearance. As I mentioned, the cilia on the surface of the bronchial epithelium are important for clearing bacteria that impact in the lung and there are two main defects, which lead to bronchiectasis in these circumstances. 05:05 One is an inherited deficiency of cilia proteins, and this shows a diagram of the cilia and cross-section, and the little blue round circles there are protein tubules, which extend up the cilia. And the common defects that you get in ciliary dyskinesia is where the connections between those protein tubules are the proteins that do that connection are affected and that means that the cilia are unable to beat and are therefore immotile and therefore unable to move the mucus up the bronchial tree and clear the bacteria from the infecting lung. 05:42 And these patients present with bronchiectasis, they also get upper airways disease in 50% they'll also have dextrocardia with a heart being on the right hand side of the chest rather than the left and that's called Kartagener's syndrome, and is an inherited disease of the cilia. The other problem of mucociliary tree which important is cystic fibrosis, and that's not the cilia, it's the mucus itself that is being affected where the mucus viscosity is being increased and therefore the cilia clearance mechanism is not working. And I'll discuss that later in this talk.
About the Lecture
The lecture Bronchiectasis: Overview and Causes by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following is LEAST likely to be an etiology of bronchiectasis?
- Asthma
- Chronic obstructive pulmonary disease
- Rheumatoid arthritis
- Cystic fibrosis
- Allergic bronchopulmonary aspergillosis
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
1 |
Excellent teacher , he is a very good teacher , explains all with perfect detail , i liked the image of a cross section of the bronchi and the mucociliary elevator
3 customer reviews without text
3 user review without text