Playlist
Show Playlist
Hide Playlist
Bronchiectasis: Diagnosis and Treatment
-
Slides 05 MajorAirwaysObstructionBronchiectasis RespiratoryAdvanced.pdf
-
Download Lecture Overview
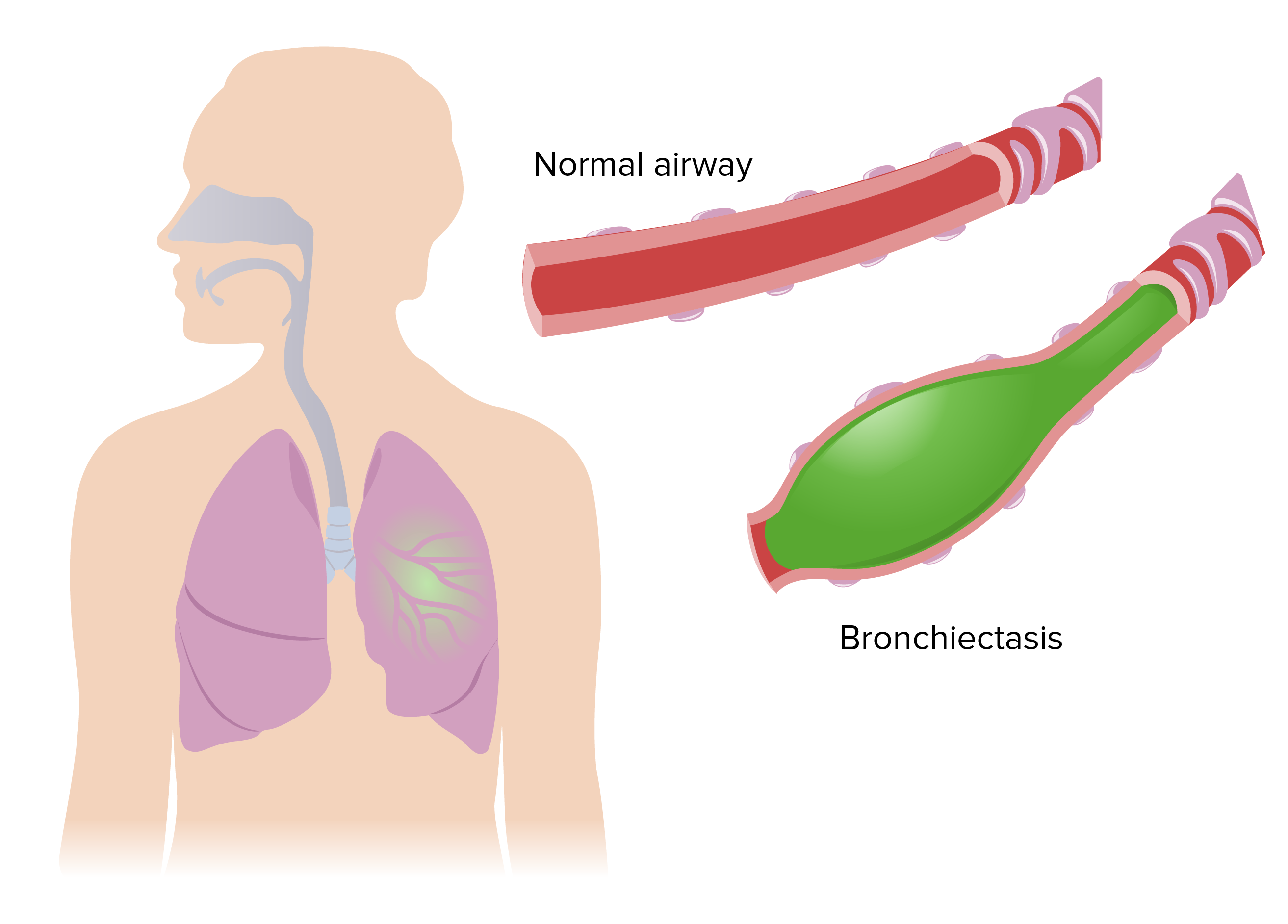
00:00 How do you made the diagnosis? Well, a chest x-ray is a very insensitive test for bronchiectasis. 00:05 Only half of patients with bronchiectasis will have an abnormal chest x-ray. 00:09 This example here of a chest x-ray shows really quite severe bronchiectasis. 00:14 However, that's unusual. 00:15 Most patients of bronchiectasis will not have an abnormal x-ray, or anywhere as nearer as abnormal x-ray as this one. 00:24 And so the diagnosis requires a CT scan, which I'll discuss in a second. 00:28 The second thing you need to do after confirm the diagnosis, you need to assess the severity. 00:32 And that's done clinically by turning, by asking the patient how many infections a year they get? And how much sputum they produce each day? Clearly, patients who are having six infections a year have more severe disease than those who are having only one infection a year. 00:45 And if somebody is producing half a cup of <inaudible> of phlegm each day, that marks them out as somebody with quite marked disease compared to those who only produce a teaspoon for or only intermittent amounts of sputum. 00:56 Lung function is very important because as I've mentioned, obstructive lung disease is the modality that causes death and respiratory failure in this patients. 01:03 So, you need to do spirometry. 01:06 And it's known that if you have somebody who has colonized their pseudomonas then they will have more severe disease so sputum culture identify those patients. 01:13 And you used to test to identify the potential cause of bronchiectasis as well. 01:19 Now, the CT appearances are dilated bronchi. 01:23 The bronchus is bigger than the accompanying vessel. 01:25 That's the basic underlying principle of diagnosing bronchiectasis in the CT scan. 01:30 The other thing about the bronchi is that the bronchi should normally taper as they go out to the periphery, in bronchiectasis they stayed non-tapering. 01:37 And you may get the consequences of airway obstruction visible on the CT scan with air trapping on the <inaudible> And when patients have really active disease bronchiectasis This is all goo, and gunk present in the small airways and that shows up as what we called tree in bud changes. 01:53 And the cause of bronchiectasis is somewhat indicated by the CT scan. 01:57 So most cases of bronchiectasis are both lower lobes, but some cases cystic fibrosis, allergic bronchopulmonary aspergillosis tends to be more upper lobe. 02:08 So how do you identify the potential cause? The history. 02:11 Somebody has rheumatoid arthritis and bronchiectasis there is likely to the rheumatoid arthritis that's causing the bronchiectasis. 02:17 If you ask the patient, they said "Yes I had these problems my cough and phlegm ever since a bad whooping cough as a child." I would suggest that there was a childhood infection that caused the bronchiectasis. 02:28 Fertility problems up airways disease indicates patients who may have cystic fibrosis, or ciliary dyskinesia. 02:34 And this CT scan here, what you see is a very focal area bronchiectasis. 02:38 Other tests you might want to do IgG levels that's very simple to measure in the blood, and will identify patients who have IgG deficiency and that's important because they can be treated with IgG replacement therapy. 02:48 There are various blood tests for allergic bronchopulmonary aspergillosis which I will discuss later. 02:53 And then if you really do think somebody has cystic fibrosis, you need to do the test for that again, which I'll discuss later. 02:59 And primary ciliary dyskinesia there are some very specialized tests on the particular centers, for cilia function that you might consider doing. 03:07 How do we treat bronchiectasis? The fundamental treatment is to try and prevent the recurrent infections, and minimize chronic phlegm production. 03:17 And we do that by advising the patient, teaching the patient how to clear their chest of phlegm. 03:22 So, they do regular physiotherapy. 03:23 And that will reduce the effective exacerbation frequency. 03:28 You should treat the cause clearly. 03:30 So, if somebody's IgG deficient, you give them intravenous immunoglobulin replacement therapy and that has a very beneficial effect on their health. 03:37 You need to know what the bugs are present in that patient's lung, so that you can guide, that will help guide your antibiotic therapy. 03:44 So sputum culture is important. 03:45 And when patients present with infective exacerbations, we will treat them with antibiotics. 03:50 And unlike normal acute bronchitis, they will need treatment for 10 to 14 days. 03:55 That will ensure that the infective exacerbations are less likely to recur quickly. 04:00 Many patients bronchiectasis get treated for four or five days of antibiotics. 04:03 And then the affection comes back within three or four weeks. 04:06 Whereas, if they given 14 days worth of antibiotics the first time, actually, they'll stay clear of infection, for several months. 04:12 And the antibiotics are dictated by which pathogen Haemophilus influenzae, Moraxalla, pneumococcus. 04:18 We normally treat amoxicillin, coamoxiclav, doxycycline. 04:21 When patients develop pseudomonas colonization then we are limited in which antibodies we can give the patient, and rarely the only oral one that's beneficial is ciprofloxacin. 04:31 And they frequently need intravenous antibiotics. 04:34 If somebody is getting recurrent exacerbations, then prophylactic antibiotics might be necessary and they can be given as tablets or nebulized form. 04:43 And because of the airways obstructions associated with bronchiectasis you may need to treat the patient with inhalers, etc. 04:50 As you would normally, for somebody with COPD or asthma.
About the Lecture
The lecture Bronchiectasis: Diagnosis and Treatment by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following causes of bronchiectasis most commonly affects the lower lobes?
- Immune deficiency
- Allergic bronchopulmonary aspergillosis
- Cystic fibrosis
- Tuberculosis
- Chronic hypersensitvity pneumonitis
Which of the following is LEAST likely to cause bronchiectasis?
- Recurrent upper respiratory infections during childhood
- Tuberculosis
- Allergic bronchopulmonary aspergillosis
- Bacterial pneumonia
- Cystic fibrosis
Which of the following is NOT associated with bronchiectasis?
- Flattening of inspiratory and expiratory flow-volume curves
- Obstructive spirometry
- Hemoptysis
- Dilated bronchi on CT scan
- Increased sputum
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |