Playlist
Show Playlist
Hide Playlist
Birth Control
-
Slides Contraception ReproductiveEndocrinology.pdf
-
Download Lecture Overview
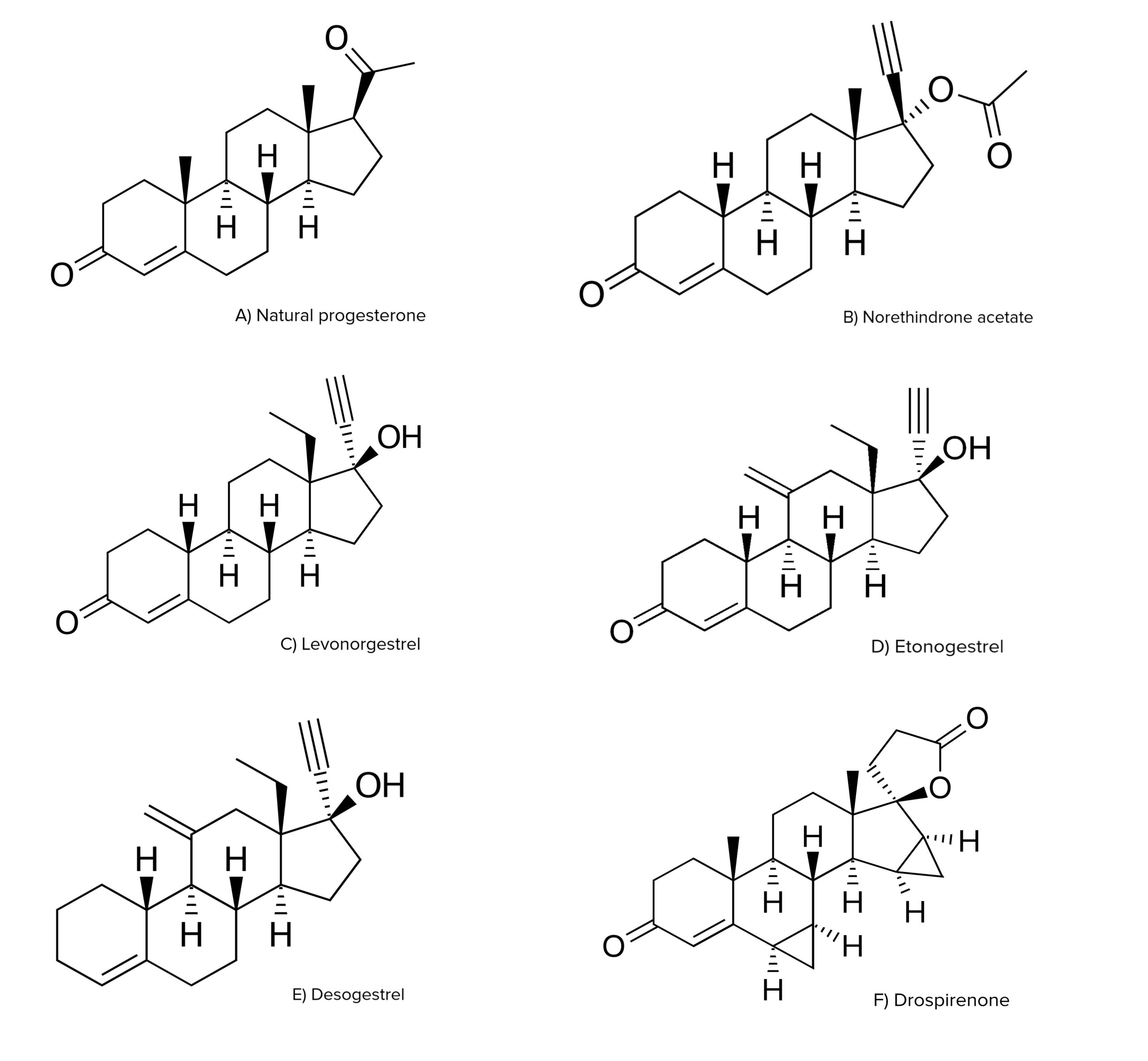
00:00 Hello. This lecture is about hormonal contraception. Pay attention, you may have an occasional question on your exam. Let’s talk about how birth control actually works. There are 2 main components. Usually, ethinylestradiol and a progestin. Ethinylestradiol actually suppresses FSH, which suppresses ovulation. Also, the progestin actually causes atrophy of the line of the endometrium and it causes the cervical mucus to thicken. There are other mechanisms of progestin as well. We think that it actually alters the peristalsis of the fallopian tubes as well as inhibiting LH surge which actually causes ovulation and myosis to resume. Let’s talk about birth control pills in general. Typically, you have a hormone-free interval of some length. Traditionally, we had a 7-day hormone-free interval. We noticed that FSH rises after the fourth pill-free day. 01:11 Therefore, you can select the dominant follicle and potentially your birth control method may fail. Therefore, we've started to do shorter hormone-free intervals that reduce ovarian activity, they lessen menstrual symptoms, and you have a shorter withdrawal bleed or your period on the birth control. Let’s talk about some of the short hormone-free interval pills that are available. 01:39 You won’t be required to know any trade names but be familiar with the contents of the birth control pill. Loestrin Fe has norethindrone acetate, ethinylestradiol, and ferrous fumarate. 01:53 Ferrous fumarate doesn’t have any activity to suppress ovulation. It’s just there as an added bonus. Yaz has drospirenone and ethinylestradiol. Seasonique has levonorgestrel and ethinylestradiol. 02:08 Lybrel has levonorgestrel and ethinylestradiol. Let’s now talk about some other methods.You can take other methods besides oral contraceptive pills. In the US, we actually do have a patch that's transdermal. It delivers 20 mcg of ethinylestradiol and 150 mcg of norelgestromin. As you can see with increasing weight, up to over 80 kg is associated with a higher failure rate. Therefore, patients who are over 198 pounds cannot use Ortho Evra or the transdermal patch. Let’s now talk about implants. There are several implants that are available, one of which is Implanon. 02:56 This contains 68 mg of etonogestrel. It’s placed in the arm and can last for a very long time up to 3 years. Another option for younger women is Depo-Provera. You may have heard of Depo-Provera. 03:15 It’s also called Depot-medroxyprogesterone acetate. It’s usually an injectible form. 03:22 Depo provera given once every three months intramuscularly. 03:27 In other countries, it may be every month. 03:30 However, the typical preparation in the United States is for it to occur as a three month every three month injection. 03:39 It can cause amenorrhea and actually some bone loss that will return to baseline after stopping it. Again, this is a better effective method for teenagers who may not remember to take a birth control everyday. 03:54 There are now four available levonorgestrel IUDs or intrauterine devices. 04:01 The trade names include Mirena, Kyleena Liletta and Skyla. 04:07 What's important to know about the levonorgestrel IUDs is that they all have similar effectiveness rates. 04:14 The Mirena has 52 milligrams of levonorgestrel IUDs, and it's approved for seven years of use. 04:19 Liletta, which has the identical mg of 52 milligrams, is only approved for six years of use. 04:26 This has to do potentially with how the devices were study. 04:31 Kyleena has 19.5 milligrams and is approved for five years of use, while Skyla has 13.5 milligrams and is approved for three years of use. 04:41 Let’s talk about how you put an IUD in. Usually, there is a device that comes with an intrauterine device that allows you to insert it into the uterus. This should be done by a trained professional as there are some risks that it go along with insertion. Insertion is associated with perforation, infection, and bleeding. No special medication needs to be given prior to insertion and insertion is typically performed in an office setting. Let’s now review emergency contraception. This means the morning after pill. 05:18 Perhaps your patient has had a sexual encounter that was unprotected. That means she didn’t have barrier method contraception and no ovarian suppression. There are different regimens but I want to call your attention to the things that are available in the US specifically plan B. Plan B also has One-Step. What happens is that you take a pill 12 hours apart from another pill and that usually prevents pregnancy within 72 hours. However, there is data that a longer time interval can actually be permitted but 72 hours is most effective. Also, we have access to ulipristal acetate or ELLA. This also needs to be taken within 72 hours and this works by modulating the progesterone receptor. Progesterone is necessary to carry on a successful pregnancy. Let’s now Copper IUD or Paragard, as it's known by its trade name, is currently approved for up to ten years of use. 06:19 However, there is data that show that it may be effective for up to 12 years of use. 06:26 Copper impairs sperm motility and prevents implantation. 06:30 However, levonorgestrel IUD at 52 milligrams is another option for emergency contraception if they are inserted within five days of unprotected intercourse. 06:41 progesterone receptor. Progesterone is necessary to carry on a successful pregnancy. Let’s now talk about female sterilization. Unfortunately, this is still a very common method in the United States but we have alternatives that are not permanent. Remember, in the US, female sterilization is usually told to the patient to be a permanent procedure. It is highly effective and does decrease the risk of ovarian cancer we think by altering the blood supply to the ovary which is shared with the fallopian tubes and the uterus. However, there are some distinct disadvantages with permanent sterilization in the female. These include regret, especially under the age of 30. 07:20 It requires a surgery and our current recommendations are to remove tubes completely with a salpingectomy. This decreases their risk of ovarian cancer in the future which is thought to start in the tube. However, as you can imagine, this is not readily reversible. If failure occurs, there is a higher risk of ectopic pregnancy if the tubes are still present.
About the Lecture
The lecture Birth Control by Lynae Brayboy, MD is from the course Reproductive Endocrinology.
Included Quiz Questions
Which of the following is NOT a mechanism by which progestin causes contraception?
- Suppression of FSH
- Progestin causes atrophy of the endometrial glands.
- Progestin causes thickening of the cervical mucus.
- Progestins alter the peristalsis in the fallopian tubes.
- Progestin inhibits LH surge.
Which of the following patients are not suitable candidates for a transdermal patch?
- Patients who is 220 pounds (99.7 kg).
- Patient who is 150 pounds (68 kg).
- Patient who is 120 pounds (54.4 kg).
- Patient who is 100 pounds (45.3 kg).
- Patient who is 80 pounds (36.2 kg).
What is the active principle in progestin implants?
- 68 mg of etonogestrel
- 52 mg levonorgestrel
- 13.5 micrograms levonorgestrel
- 100 micrograms norgestrel
Which of the following is an example of an injectable type of contraception that can be taken once a month?
- Depo medroxyprogesterone acetate
- Yuzpe regimen
- Plan B / next choice
- Plan B one step
- Ullipristal acetate
Women who have undergone tubal sterilization have an increased risk of which condition?
- Ectopic pregnancy
- Ovarian tumors
- Fallopian tube Cancer
- Rupture of fallopian tubes
- Ovarian cysts
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |