Playlist
Show Playlist
Hide Playlist
Benign Liver Tumors
-
Slides GIP Benign Liver Tumors.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
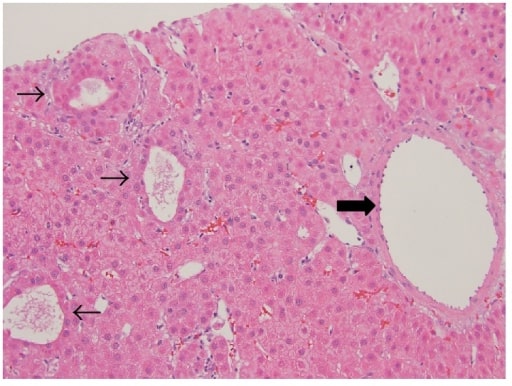
00:01 Hello there, welcome. 00:02 We're going to be talking about benign liver tumors. 00:06 So there are three things that we have to keep in mind when we talk about these benign tumors of the liver. 00:11 Hemangiomas, focal nodular hyperplasia, abbreviated FNH. 00:15 And hepatocellular adenomas, also called hepatic adenomas. 00:19 And we're going to cover these each and sequence. 00:22 And then at the end of this, you will know 95%, of benign liver tumors. 00:28 Epidemiology. 00:30 So for hemangiomas, it is the most common benign liver tumor. 00:33 In fact, many of you who are watching this video have one. 00:37 So relatively high prevalence, upwards of 1/5 of the population has one, I know that I have about four. 00:44 So I'm special. 00:47 It occurs more frequently in women than in men. 00:49 And it may have to do with hyperestrogenic states, giving rise to increase vascular proliferation. 00:55 And it's very typically not found because there's any symptoms but found incidentally, at the ages of 30 to 50. 01:04 Focal nodular hyperplasia, or FNH is the second most common benign liver tumor, and it has a much less prevalence in the population, not as much as 20%, but more in the range of 2% or 3%. 01:17 Women, again, are more commonly associated with FNH. 01:21 And it's found incidentally in the same age range. 01:25 And then finally, hepatocellular adenomas. 01:27 Relatively rare, especially compared to the other two. 01:31 Again, more common in women than in men. 01:33 And they're also found incidentally in roughly the same age range. 01:38 So let's go back, hemangioma. 01:39 Really, really common. 01:41 On gross examination, they're often solitary occasionally multiple, as in me. 01:46 Lesions, they have kind of a red brown, spongy mass, frequently with a capsule, most are less than five centimeters in cross sectional diameter. 01:56 On microscopic examination, there are cavernous, vascular spaces lined by endothelium. 02:01 So these are just vascular malformations of the liver and really common in the liver. 02:08 They may contain thrombi, and for certain giant hemangiomas, they may be thrombosed, which can lead to complications. 02:15 The pathogenesis, kind of unclear overall, it's likely a congenital vascular malformation, so you're born with them. 02:22 And over time, they may get slightly larger. 02:25 As already indicated, more frequently seen in women than in men, they may be associated with estrogenic states, so maybe associated with oral contraception, or pregnancy, and those may promote growth. 02:36 So a relatively small lesion that over the course of a pregnancy, for example, may grow somewhat. 02:44 The clinical presentation, as I've already said, they're typically found incidentally on some sort of other imaging, so they're most commonly asymptomatic. 02:53 The physical examination is often completely normal unless they're gigundo, in which case, you may have a palpable liver mass. 03:01 If they are sufficiently large, they may cause right upper quadrant pain or fullness. 03:07 They may compress other organs and they can manifest with nausea, early satiety, bloating, or as we'll see in a moment coagulopathy. 03:18 So, those that a rather large, these are giant hemangiomas, greater than 10 centimeters in diameter can give rise to a coagulation disorder associated with kind of slow percolating flow of the bloodstream through this hemangioma. 03:37 This is the Kasabach-Merritt syndrome. 03:40 So, because there is kind of turgid sluggish flow, there is a tendency to get thrombosis and it may be a reason that you use up platelets and you have a consumptive coagulopathy. 03:53 So you get thrombosis within the lesion within a hemangioma. 03:58 But then, by consuming platelets and coagulation factors, you get systemic bleeding other places. 04:04 Depending on the size of the hemangioma. 04:07 There can be a mortality rate as high as 35%. 04:11 But if we recognize what's causing this, we can carve them out in most patients, and in most cases, patients will do quite well. 04:19 How to make a diagnosis of hemangioma, small or large, ultrasound is a great way to do it, it's non invasive, and you will see a homogeneous hyperechoic mass. 04:29 They can also be visualized by MRI and CT. 04:32 You would not biopsy it because if you biopsy them, there's a risk of bleeding. 04:37 They're just big dilated vascular malformations. 04:41 Management in most cases, you'll let them be, but if they are symptomatic, say in Kasabach-Merritt, or the rather large in causing pain, you can resect them by surgery. 04:53 That's everything you want to know about hepatic hemangiomas. 04:56 Let's talk about focal nodular hyperplasia or FNH. 05:00 On gross examination, they are firm solitary lesions without a capsule, they don't have kind of the redness and the sponginess that we saw on hemangiomas. 05:10 On the other hand, these are quite fibrous, they tend to have a central stellate scar that's characteristic. 05:16 Again, the size is usually less than 5 centimeters like hemangiomas. 05:21 What we see on microscopic examination are grouped hepatocytes with fibrous septa, kind of radiating out from a central scar. 05:30 All of the septa contain normal architecture, normal things found within the portal triads, arteries, portal veins, bile ductules, and Kupffer cells. 05:40 The pathogenesis is thought to be a regenerative response of the liver to alter perfusion from an anomalous artery. 05:48 So you have an artery that is intermittently twisted or torsed or not perfusing very well and you get an area of necrosis that gives you that central scarring, and then as the liver tries to regenerate, with kind of malperfusion in that area, you get the kind of stellate appearance overall and the focal nodular hyperplasia. 06:11 There is no malignant potential whatsoever, and in diseases such as hereditary hemorrhagic telangiectasia, otherwise known as Osler-Weber-Rendu, there is an increased risk of FNH occurring. 06:23 And this has to do with aberrant arterial circulation. 06:28 The clinical presentation is it's almost totally asymptomatic, found most commonly incidentally on imaging. 06:35 If there are symptoms, they tend to be abdominal pain with rather large FNH. 06:40 Usually, the physical exam is non revealing, but there may be an abdominal mass but that's exceptional. 06:46 The diagnosis is based on ultrasound or MRI, which is showing a central area of fibrosis and kind of a radiating lesion that has a different density and then the surrounding liver. 07:00 For asymptomatic patients, don't do anything. 07:04 The lesion rarely grows, you don't even have to follow up. 07:07 If the patient is having pain, you may want to undergo arterial embolization. 07:13 So you would want to identify the vessel that's feeding into this area and ablate that and all of the lesion will go away. 07:20 You can also do radiofrequency ablation, or you can do a surgical resection. 07:25 Okay, now you've known everything, there is to know about focal nodular hyperplasia. 07:31 The last entity is a hepatocellular adenoma. 07:34 Relatively rare, these tend to be solitary lesions, a well defined margin, but they can occur as multiple lesions, There are various sizes, These tend to lack a fibrous capsule, and therefore if there's any trauma to, especially the larger ones, there's risk for rupture and for bleeding. 07:52 On microscopic examination, we have sheets of distended hepatocytes that have small nuclei, lots of glycogen and lots of lipid. 08:00 It's basically a benign hepatic proliferation. 08:06 There will be no portal tracts, no bile ductules, this is to distinguish it from focal nodular hyperplasia, and that because it's a pure proliferation of hepatocytes. 08:17 It is a benign epithelial tumor, Associated findings, or associated risk include oral contraception, and anabolic steroids which can engender the proliferation of epithelial cells within the liver. 08:32 There may be certain genetic syndromes where we see this occurring glycogen storage diseases, and familial adenomatous polyposis. 08:40 And it is also associated with obesity and metabolic syndrome, for unclear reasons. 08:45 The pathogenesis, so in the majority of cases, where we know what is causing them, it's a loss of function mutation, in hepatocyte nuclear factor-1 alpha, this is going to be associated with increased proliferation. 09:03 About 40% of cases will have this mutation. 09:06 It is associated with steatosis predominantly occurs in women. 09:10 So there's an estrogen component at very low risk of malignant transformation. 09:16 And it's also associated with mature onset diabetes of the young Mody type 3. 09:21 And again, for reasons that I'm not entirely clear about. 09:25 You can also have mutations in the beta-catenin gene or other pathway or other molecules involved in the WNT catenin stimulatory pathway. 09:36 It's a lesser frequency, roughly half of the number of cases associated with hepatocyte nuclear factor-1 alpha, and those mutations occur more frequently in men. 09:46 Again, these are lesions or mutations that are going to drive local hepatocyte proliferation but they have essentially no risk of malignant transformation. 09:57 These hepatic adenomas may be largely asymptomatic, but in a quarter of the patients they get sufficiently large that they present with pain or a mass in the right upper quadrant. 10:09 There is increased risk of hemorrhage when they're greater than five centimeters, and bleeding into the lesion can present with acute abdominal pain. 10:18 And severe cases rupture into the peritoneum presents with severe pain and you can even have hypotension with the possibility of exsanguination. 10:26 So recognizing these as an entity. 10:29 The diagnosis is made on any of a variety of imaging modalities, probably CT or MRI is going to be your best bet. 10:36 Ultrasound can also see them and we see it circled here on the right hand panel with a rather large hepatic adenoma, totally benign proliferation, and this one probably would need to be resected just so we don't have a massive bleed within the peritoneum. 10:52 So how are we going to manage it? Well, we try to get rid of the causes that drive us so we know anabolic steroids, oral contraception can be major drivers of the proliferation so you can discontinue those. 11:06 The association with obesity and metabolic syndrome would suggest that weight loss might be helpful. 11:13 You can definitely undergo surgery, which is probably the mainstay, but in patients who are not otherwise surgical candidates, because of associated morbidities. 11:24 You may do a trans arterial embolization and just inject material that cause thrombosis of the vessel that feeds into the adenoma. 11:34 With that you have covered the three major benign tumors of liver: hemangioma, focal nodular hyperplasia and hepatic adenoma.
About the Lecture
The lecture Benign Liver Tumors by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What is the most common benign liver tumor?
- Hemangioma
- Adenoma
- Focal nodular hyperplasia
- Hepatocellular carcinoma
- Liver metastasis
Which statement about focal nodular hyperplasia is true?
- It has a 2%–3% prevalence in the population.
- It is more common in men than in women.
- It is most common between ages 10 and 20.
- It is most common between ages 50 and 60.
- It is equally common among men and women.
What is the most common presentation of a benign liver tumor?
- Incidental finding in an asymptomatic patient
- Palpable liver mass
- Nausea
- Abdominal bloating
- Hypercoagulation disorder
What is a rare coagulation disorder associated with giant hemangiomas?
- Kasabach-Merritt syndrome
- Acute brain syndrome
- Gilbert syndrome
- PEHO syndrome
- Kartagener syndrome
What is the appearance of a hemangioma on liver ultrasound?
- Homogeneous hyperechoic mass
- Homogeneous hypoechoic mass
- Heterogenous hypoechoic mass
- Heterogenous hyperechoic mass
Which test has the best diagnostic accuracy for focal nodular hyperplasia?
- MRI
- Ultrasound
- CBC
- CT scan
- Arterial embolization
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |