Playlist
Show Playlist
Hide Playlist
Bacterial Meningitis: Diagnosis
-
Slides CNS Infections Meningitis.pdf
-
Download Lecture Overview
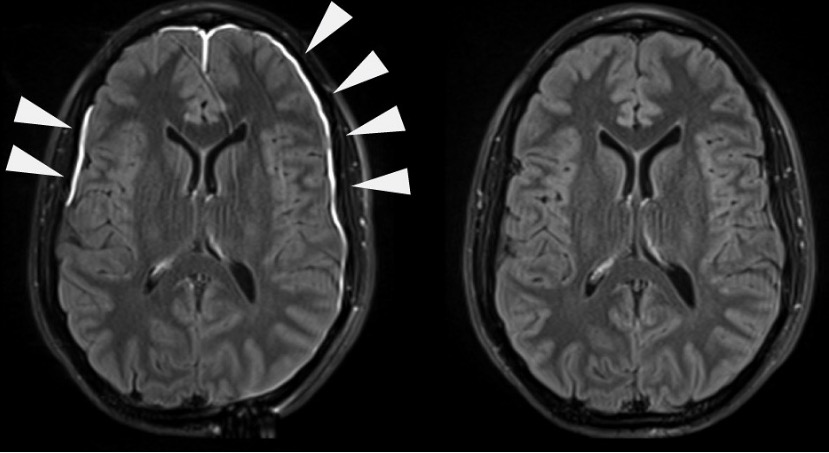
00:00 How do we diagnose meningitis? Well it starts with a good history and a comprehensive neurologic exam looking for signs of meningeal irritation and potentially signs that we're in a dire strait with late complications like papilloedema, abducens nerve palsies, and Cushing reflex. Then we need to do a laboratory assessment. Look at the complete blood count, comprehensive metabolic profile, maybe coagulation test, and a pregnancy test. Complete blood count is important for looking at the white blood cells. Is there evidence of a systemic infectious process? Are metabolic profile looks at the kidney and the liver? Liver enzymes can be elevated in viral processes. Kidneys can be dysfunctional in patients who are dehydrated. And coagulation studies are not required but in selected patients are important prior to doing a spinal tap. Sometimes we'll look for a source of a systemic infection with a chest x-ray to look for pneumonia or blood cultures or urine cultures to look for some site of an initial infection that then travelled to the brain. We see pneumonias that go to the brain and urosepsis, UTIs that go to the brain and bacteremia that goes to the brain and to the CNS space and so those are important places to look. But ultimately, usually the test of choice is the lumbar puncture and we're looking for signs of infection and we're thinking about that word pleocytosis. And that means too many cells in the spinal fluid, too many white blood cells means infectious and really inpoints us in the direction of an infectious meningitis. Do we need to do imaging before our spinal tap? Well, oftentimes patients get imaging. They come in to the emergency department and a CT of the head is done and we know what that looks like before the spinal tap but not always. And there are 5 indications for getting imaging, a CT of the head, a computed tomography, a CAT scan of the head or an MRI prior to lumbar puncture. 01:53 And these are the 5. If the patient has a focal neurologic deficit, there could be a mass lesion in the brain, that mass could cause a pressure differential and we wouldn't want to LP that patient without looking at the imaging. If there is a new onset seizure. New onset seizure means a mass lesion in the brain until proven otherwise, and if there is a mass lesion in the brain there could be a pressure differential and we need imaging before evaluating that patient. Papilloedema. Papilloedema means increased intracranial pressure until proven otherwise, and that is coming from a mass, again until we have imaging that says that it's not. If there is a mass lesion, there could be a pressure differential. We wouldn't want to LP that patient unless we have imaging. Abnormal level of consciousness. We can't do a comprehensive exam in many of those patients to look and be convinced that there is not a focal deficit or some type of papilloedema. And so again, abnormal level of consciousness impairs our ability to look on exam for a new mass lesion for a pressure differential and those patients need imaging. And then the last indication for imaging before LP is an immunocompromised state. Weird things happen, different things happen and patients don't always present with the typical symptoms so it's harder for us to trust our history and exam in patients who are immunocompromised and we need imaging to show that there is not a pressure differential, that there is not a risk of herniation with the spinal tap and we get imaging before spinal tap in those patients. So the 5 indications for imaging prior to LP. 03:25 Once we do the spinal tap, we need to know how to approach it and we ask a series of questions to guide us in interpreting the finding. The first thing we want to know is "Is there an infection?" And we look at the white blood cells. If the white blood cells are elevated, we call that a pleocytosis and this indicates infection until proven otherwise. If the white blood cells are not elevated, we need to think of other considerations in the differential for this patient. If we're dealing with a pleocytosis, if white blood cells are elevated, we want to know if it's bacterial, viral, or fungal. And there is a different signature for each of those. For bacterial infections, we often see elevated polymorphonuclear cells and increased PMNs should favor bacterial infection over viral, fungal, or some other type of organism. With viral infections, we see monocytes, a lymphocytic predominance, not the polymorphonuclear cells but lymphocytes often with mildly elevated protein and normal glucose and that signature should point us in the direction of a viral infection. For fungal infections, we also see increased monocytes, lymphocytes, that's what responds to a fungal infection but here we often see low glucose, hypoglycorrhachia, and that signature should point us towards a fungal process. 04:44 So this table helps us to walk through the types of infectious organisms that we'd be concerned about based on CSF findings. And as a reminder, when we look at CSF we're going to think about the opening pressure, the white blood cells, how elevated they are or not, the differential of those white blood cells, the glucose level, the protein, and in some cases the presence of red blood cells. For bacterial infections, we see that the opening pressure is often elevated, there is significant pleocytosis, increase in white blood cells, we see either sometimes upwards of 200 white blood cells in the CSF. The differential on those white blood cells is they are frequently polymorphonuclear cells, this is an acute infectious process and acute inflammatory response to that. The glucose is low and there is not a normal value of glucose. 05:35 CSF glucose is based off the serum glucose and we see that CSF glucose and bacterial infections is frequently less than 60% that in the serum, the protein level is very high and there can be a few red blood cells. With the viral process, again, we can see slightly elevated opening pressure, there is a pleocytosis but not as prominent as with bacterial infections usually less than 200 cells though this is highly variable. It's monocytic, lymphocytic predominant with normal glucose and normal protein unless there is a vigorous inflammatory process associated with the virus. For fungi, we see normal to high and in some fungal infections significantly elevated opening pressures with the pleocytosis but much milder than what we see with bacterial infections, typically we see monocytic or lymphocytic predominant pleocytosis with low glucose. This is an important difference between viral and fungal infections and often with high protein or mildly elevated protein. And then with TB, an important atypical cause of meningitis, we often see elevated opening pressure, a mild pleocytosis, lymphocytic predominant, low glucose, and high protein. So here's a table that can guide us in evaluating that most important spinal tap.
About the Lecture
The lecture Bacterial Meningitis: Diagnosis by Roy Strowd, MD is from the course CNS Infections.
Included Quiz Questions
Which of the following is an indication for performing a brain computed tomography (CT) scan prior to lumbar puncture?
- Papilledema
- Headache
- Hypotension
- Leukocytosis
- Meningismus
What is the test of choice for bacterial meningitis?
- Lumbar puncture
- Computed tomography (CT) scan
- Blood and urine cultures
- Complete blood count
- Complete metabolic panel
Which of the following CSF findings is consistent with bacterial infection?
- Opening pressure = 25 cm H2O
- White blood cells = 40/mm^3
- Glucose = 60 mg/dL
- Red blood cells = 200/mm^3
- 80% monocyte predominant
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |