Playlist
Show Playlist
Hide Playlist
Abnormal Uterine Bleeding (AUB): Introduction and Classification
-
Slides AbnormalUterineBleeding ReproductiveEndocrinology.pdf
-
Download Lecture Overview
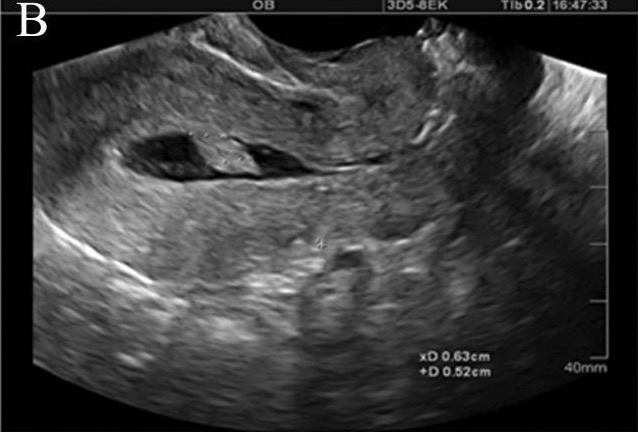
00:00 Hi. Now we’re going to discuss abnormal uterine bleeding. This is abbreviated AUB, so you’ll hear me say that over and over again during the lecture. Abnormal uterine bleeding or AUB was traditionally called menorrhagia. The research standard for menstrual blood loss was greater than 80 mL. However, on average, women menstruate about 25 mL to 30 mL. Metrorrhagia was bleeding in between periods. So, again, recall menorrhagia was heavy bleeding, metrorrhagia was bleeding in between your normal scheduled period. Polymenorrhea is bleeding that occurs more often than every 21 days and that’s just really annoying. Oligomenorrhea is when your period doesn’t come as often as it should. Oligomenorrhea is less than every 35 days. So, as you can probably imagine, the normal period is between 21 and 35 days in length between the time you bleed to the next cycle. Let’s talk now about AUB classification. This is a newer classification and it starts with AUB, AUB-HMB, which is heavy menstrual bleeding, which was formerly referred to as menorrhagia, intermenstrual bleeding which was formerly referred to as metrorrhagia and there are different causes. So if you look at structural causes, the first thing that you see in the new classification system is AUBP. AUBP stands for polyp and a polyp can cause any one of the above bleeding abnormalities. AUB-A stands for adenomyosis which is a common cause of chronic pelvic pain and there is another lecture that you can refer to about chronic pelvic pain. Then there’s AUB-L, which is leiomyoma or fibroid as it’s traditionally called. Within leiomyoma or AUB-L, you’ll see here that you can have a submucosal myoma, which is within the cavity and that is abbreviated AUB-LSM for submucosal or you can have other myoma and that's AUB-LO for another myoma. We’ll review myoma shortly. Then, the M under PALM of the PALM-COEIN system, which is the new system, is malignancy or hyperplasia and this is referred to as AUB-M. 02:40 You may see this in a chart once you start on your clinical rotations. Now, let’s look at non-structural causes: coagulopathy, AUB-C, is one; ovulatory dysfunction, meaning you probably have oligomenorrhea or AUB-O; endometrial causes, so there’s something wrong with the endometrium like endometritis, this is AUB-E; or iatrogenic, AUB-I, which means we’re giving the patient something that causes them to have more bleeding than they normally should. Okay, let’s now discuss some specifics about the structural causes of AUB. Here we have AUB-P. As you remember, that stands for polyp. Endometrial polyps are an overgrowth of cells that are usually benign and present with bleeding but usually they can be asymptomatic. However, if a patient says, “You know, I have a history of bleeding in between periods,” that is intermenstrual bleeding or metrorrhagia. You could consider polyps as a diagnosis. Well, how do we diagnose polyps? Well, the best way is to do a saline-infused sonogram and here you can see an ultrasound followed by an ultrasound with saline infusion, so we actually use a catheter which we put saline through using a syringe and we’re able to actually open the walls of the uterus and see if there’s any pathology. If you stuck a camera directly into the uterus, you would see, via hysteroscopy, polyps that look like these in the last picture. You can see it’s nice and pink. It looks like the normal endometrium. It’s just an overgrowth. Let’s talk about the risk factors for developing polyps. Obesity which is very common in the US, hypertension which goes along with obesity, diabetes which also correlates with hypertension and obesity and advancing age. Recall that tamoxifen usage is associated with polyp development. So, in a lot of women who’ve had breast cancer that is estrogen-receptor positive, will be on tamoxifen. Let’s now talk about adenomyosis, AUB-A. Adenomyosis was formerly termed endometriosis interna, which in some ways was an interesting name because endometriosis, which is covered in another lecture, chronic pelvic pain, is actually the presence of stroma and glandular tissue that should normally be in the endometrium inside the actual myometrium of the uterus. Classically, an adenomyotic uterus is large, boggy, globular and usually these patients suffer from chronic pelvic pain. Let’s now discuss abnormal uterine bleeding due to leiomyomas. This is AUB-L. Uterine leiomyomas are also called myomas or fibroids. 05:40 They are usually benign and come from 1 single cell, actually undergoing expansion into a large tumor. They’re unlikely to be cancerous but less than 1% are reported to be so. More than 80% of African-Americans actually have leiomyomas and more than 70% of Caucasian or European descendant Americans also have leiomyomas. So they’re very, very common and it actually increases as time goes on in the reproductive lifespan. There are lots of detail specifics about leiomyomas and so if you’re in a rush you might want to skip through this and go on to the other causes of AUB. But I’ll review this now. You can see here that African-American versus Caucasian women have a three-fold increase of having fibroids. The age of diagnosis in African-Americans tend to be 3 to 5 years younger, and the severity, that means the pain, the pressure that they may be experiencing, or the bleeding, such as the AUB that we’re discussing, has a five-fold increase. 06:51 Fibroid growth at older ages is actually increased seven- to eight-fold. The risk of having a myomectomy, which is a surgery where you remove the fibroids, is a six-fold increase and the risk of hysterectomy is a two- to three-fold increase. So you can see here that African-American have a higher incidence and also suffer more from fibroids. Here, this is a pathology slide of a smooth muscle tumor, which is what you would see with leiomyomas. Remember that most of them are benign but we still need to check the pathology to make sure that’s true. This is a lovely diagram that shows where leiomyomas can occur. There have been abnormal locations such as on the bowel but they usually occur within the uterus. Their location differs by how we describe them. 07:44 Rather we describe them differently based on their location. So you can see here that a fibroid that’s inside the uterus in the lining is called a submucosal fibroid. A fibroid that’s within the muscle of the uterus is called an intramural fibroid. A fibroid that’s kind of just hanging, whether it be a submucosal or subserosal, is a pedunculated fibroid. Subserosal means it’s just under the tissue that lines the outside of the uterus. Depending on their location, they can cause bleeding, pain, and pressure in the patient. This is a view of a uterus at laparoscopy, which is a minimally invasive surgery where we look in with a small camera usually through the belly button. You can see here this uterus is distorted by the presence of fibroids. This patient is likely going to be undergoing a laparoscopic myomectomy. They can be opened or abdominal myomectomies as well or a hysteroscopic myomectomy. Let’s now move on to AUB-C, coagulopathy. Again, these next following AUB slides will be non-structural causes. Approximately 20% of patients who are adolescent with AUB will have an underlying coagulopathy. So, remember on your exam to check for the presence of abnormalities and their bleeding times or potentially, platelet function disorders, Von Willebrand disease or other coagulation factor issues. Usually, these patients have some type of history that they will give you. The initial screening though should include questions that specifically pinpoint these historical issues. So, you want to ask them, "Did you have heavy menstrual bleeding since the beginning of your periods?" That’s referred to as menarche. So, if they report either a postpartum hemorrhage or surgery-related bleeding or bleeding associated with dental work, that should be a clue that they may have a coagulopathy. If they report one of those but 2 of these, which is bruising over 1 or 2 times per month epistaxis, which is nosebleeding 1 or 2 times a month, frequent gum bleeding 1 or 2 times a month or even once a month and family history of bleeding, you should be concerned. So, again, one of the first category and two of the second category makes you think that there could be AUB-C or coagulopathy. Let’s talk now about AUB-O, ovulatory. Anovulatory cycles result in a range of disorders. Amenorrhea means you have no menstrual period but you then can have a period which can be irregular and very heavy because you’re not shedding as you should every month. The most common cause is due to polycystic ovarian syndrome. There is another lecture about PCOS or polycystic ovarian syndrome that you can look at to explain more. Let’s now review AUB-E, endometrial. This classification refers to endometrial causes. Of course, we discussed endometritis which is very common in young women who may be susceptible or have STIs. Let’s now review one of the final classifications which is AUB-I or iatrogenic which means we, as healthcare providers, have actually caused the AUB through some type of medication, whether it be contraceptives that cause breakthrough bleeding or regular bleeding with a levonorgestrel IUD for the first 3 to 6 months, or anticoagulants, or antipsychotics chemotherapy which decreases the overall clotting ability, or spironolactone which is the medication that we talk about in the hirsutism lecture, or drugs related to dopamine metabolism such as antidepressants and antipsychotics.
About the Lecture
The lecture Abnormal Uterine Bleeding (AUB): Introduction and Classification by Lynae Brayboy, MD is from the course Reproductive Endocrinology. It contains the following chapters:
- AUB: Introduction and Classification
- AUB-P (Polyp), AUB-A (Adenomyosis) & AUB-L (Leiomyoma)
- AUB-C (Coagulopathy), AUB-O (Ovulatory), AUB-E (Endometrial), AUB-I(Iatrogenic)
Included Quiz Questions
Which of the following is a non-structural cause of abnormal uterine bleeding?
- Coagulopathy
- Polyp
- Adenomyosis
- Hyperplasia of the endometrium
- Leiomyoma
Which of the following is NOT a risk factor of polyps in the female genital tract?
- Smoking
- Obesity
- Hypertension
- Advancing age
- Diabetes
Which drug is associated with the formation of endometrial polyps?
- Tamoxifen
- Oral contraceptive pills
- NSAIDs
- Macrolide antibiotics
- Clomifene citrate
Which of the following features is NOT characteristic of an adenomyotic uterus?
- Asymmetrical enlargement of the uterus
- Boggy
- Globular mass
- Trabeculated areas on cut sections of uterus
- Multiple hemorrhagic spots within the myometrium
Which population has a higher risk of developing uterine leiomyomas?
- African Americans
- Caucasians
- Asian Americans
- Latin Americans
- Native Americans
Which of the following types leiomyomas is more likely to undergo torsion or strangulation, and cause abdominal pain?
- Pedunculated leiomyoma
- Sub-mucosal leiomyoma
- Intramural leiomyoma
- Atypical leiomyoma
- Cellular leiomyoma
Which of the following scenarios is considered sufficient to suspect a coagulopathy in a patient with AUB?
- Massive bleeding associated with dental work
- Epistaxis one or 2 times a month
- Bruising one or 2 times a month
- Frequent gum bleeding
- Family history of bleeding disorders
Which of the following is NOT an iatrogenic cause of abnormal uterine bleeding?
- Antitubercular drugs
- Contraceptives
- Anticoagulants
- Chemotherapy
- Spironolactone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |