Playlist
Show Playlist
Hide Playlist
Atrial Septal Defect (ASD)
-
Slides Obstructive heart disease and detour defects.pdf
-
Reference List Pediatric Nursing.pdf
-
Download Lecture Overview
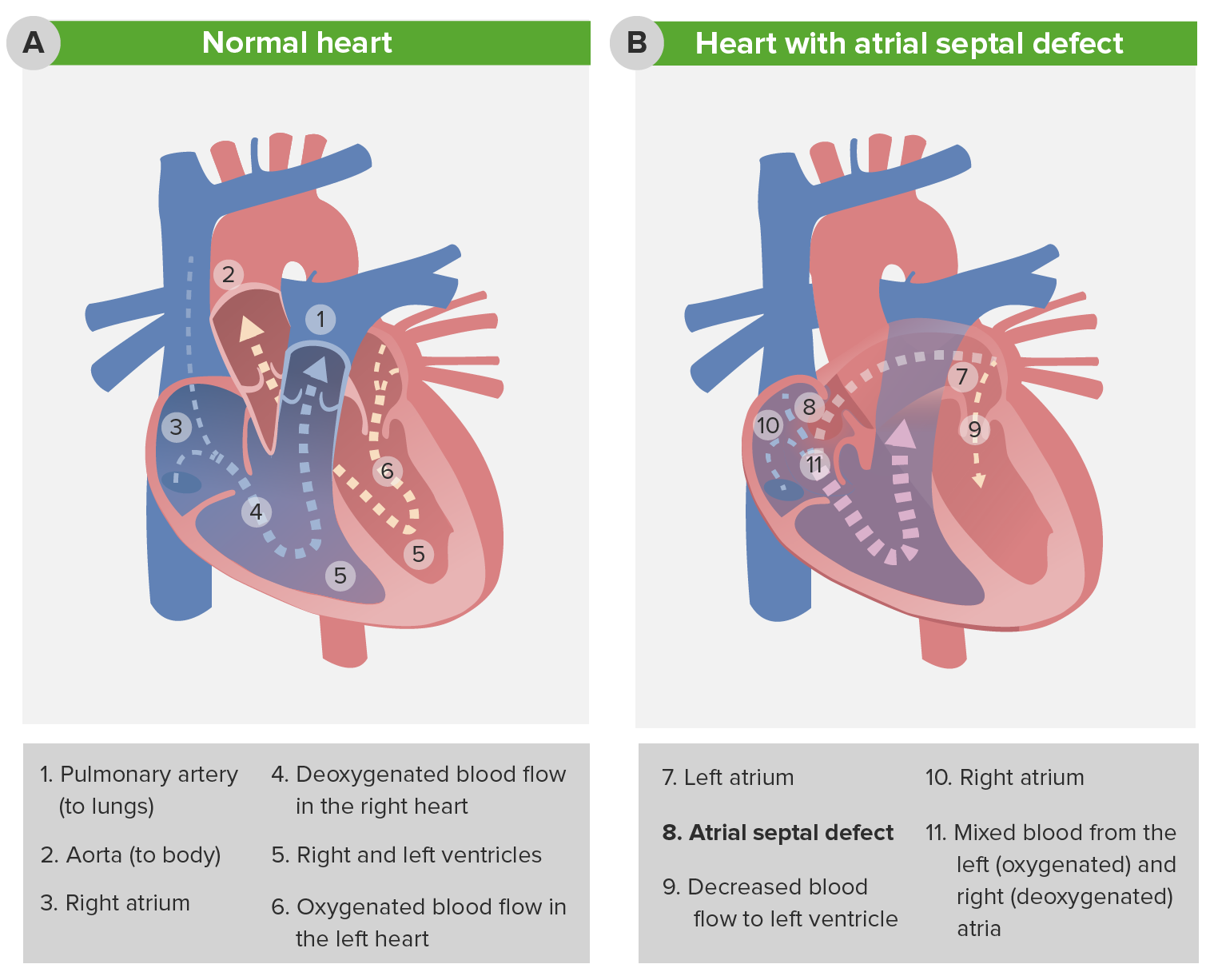
00:01 Move on to another one - this is the atrial septal defect. 00:05 In general, the atrial septal defect is a fairly benign condition. 00:11 It doesn't cause a lot of problems for patients. 00:14 If it needs to be repaired, it can usually be repaired through catheterization rather than open-heart surgery. 00:22 Basically, the blood is going from the left atrium into the right atrium. 00:29 Remember that the pressure difference between the left atrium and the right atrium isn't nearly as big as the pressure difference between the left ventricle and the right ventricle. 00:38 This minimal pressure results in relatively less blood flow. 00:43 But over time, as that blood is going backwards from the left atrium into the right atrium, you're getting a little bit of pulmonary overcirculation. 00:54 Gradually, this can lead to right ventricular hypertrophy and a little bit of tricuspid regurgitation as that area is being stretched apart. 01:06 When you see a patient with an atrial septal defect, you may not notice the murmur. 01:12 It's often a very soft murmur, it maybe absent. 01:15 But one clever thing you may hear is a fixed-split S2. 01:21 The split S2 is something you should practice listening. 01:24 You can hear it on yourself. 01:26 If you place your stethoscope right over your valves and you listen to your S2, you should hear, while breathing in, a slight difference in the time when the S2 hits. 01:42 That very, very slight difference is because you're having, when you're breathing in, a slight increase in venous return resulting in a little bit more filling of that right ventricle. 01:55 Starling forces cause an improved but delayed emptying of that right ventricle. 02:02 And so that pulmonary valve closes just a little bit later than the aortic valve. 02:08 When you're breathing out, the pressures are the same, and so those two close simultaneously. 02:15 In an atrial septal defect, there's always a little bit of pulmonary overflow. 02:21 That left to right shunt is always happening - so that pulmonary artery delay is always happening. 02:27 And so, the patient will have a split in their S2 pretty much all the time regardless of where they are in their respiratory cycle, and that may be the only only way you diagnose this condition, So listening to that S2 is critical. 02:41 You may notice on an EKG that, sometimes these patients have right ventricular conduction delay, but you really need an echo to make the diagnosis. 02:53 Most ASDs are small and most will spontaneously close on their own over time. 03:00 It may be that for this patient all you do is say, "Follow up with the cardiologist. Get an echo every now and then, we'll likely see this close." However, for very large ASDs, you may require surgery for closure and certainly you would require surgery for closure in symptomatic patients. 03:16 Patients who are symptomatic may have failure to thrive, sweating with feeds -- things along that line.
About the Lecture
The lecture Atrial Septal Defect (ASD) by Brian Alverson, MD is from the course Pediatric Cardiology.
Included Quiz Questions
Which of the following physical findings may be noted in a patient with Atrial Septal Defect (ASD)?
- A fixed splitting of S2
- A harsh holosystolic murmur
- Jugular venous distension
- Pansystolic washing-machine-like murmur
- A diastolic rumble
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
I think it's an excellent lecture. However, I do agree with another member, I would have liked to see for these diseases the prevalence number of the diseases. Otherwise I think the relevant information to think about the disease is in the lecture.
Engaging. Good clinical correlation from his own experience in practice. Good explanation of physiology and tie in with pathology.
too short vert underutilized lacks content..how to see longer videos