Playlist
Show Playlist
Hide Playlist
Neuroepithelial Tumors: Astrocytoma
-
Slides 08 Tumors of the CNS Neuropathology II.pdf
-
Download Lecture Overview
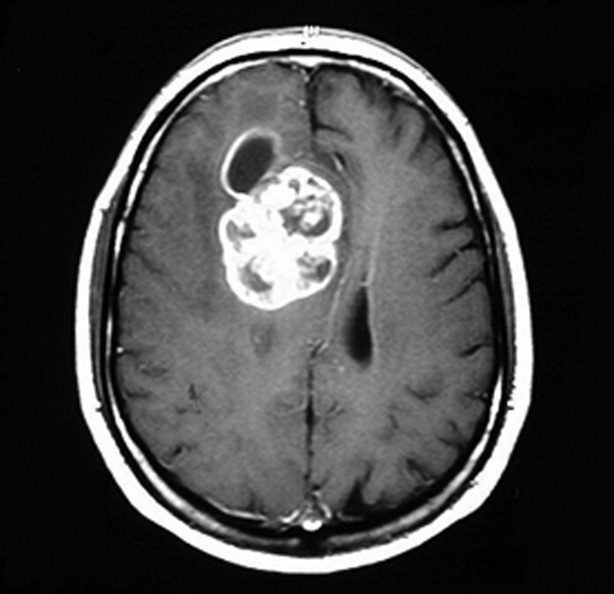
00:01 Our topic here is neuroepithelial tumor. 00:04 To begin with, where are we in terms of organization? Primary metastasis, this is primary CNS tumor. 00:12 Under primary CNS tumor, we're looking at neuroepithelial tumor. 00:17 The classification of neuroepithelial tumor would be your astrocytic or astrocytomas. Let’s take a look. 00:26 Definition. Tumor derived from, as you can imagine, astrocytes. 00:30 You think of these as being glial cells and how often have you come across a description, a reading or a narration or let us say a CPC, a pathologic conference in which you're seating around and you hear the term anglioma, right? Well, this is what we're referring to. 00:50 So the fact that you have an astrocytoma, please be aware that anatomically, these cells, glial cells, and at some point these would then be referred to as being gliomas. 01:02 The types. We’ll take a look at low grade astrocytoma. 01:09 Anaplastic is never a good thing. 01:11 A glioblastoma multiforme, we’ll be spending time with this one in great detail and the reason for that is, it is one of the most common unfortunate brain tumors that occurs in adults but really could be seen across the spectrum. 01:26 Then we have an astrocytoma that occurs almost exclusively in children, and this is then referring to your pilocytic astrocytoma and you'll be focusing upon the cytic and I’ll tell you why in a bit. And then you can have your what's known as your pleomorphic xanthoastrocytoma. 01:48 Let’s take a look at astrocytoma further, and under here, 80% of adult primary brain tumors will be an astrocytoma, that’s how important these gliomas are, 80% of adult primary brain tumor, you wanna put yourself into the category of astrocytomas, let it be your fibrillary, anaplastic or anglioblastoma multiforme. 02:16 Usually arise in the cerebral hemispheres as you can imagine because we're not dealing with our meninges usually presents with as you can imagine once again the brain parynchema so therefore perhaps focal neurologic deficit, maybe there's headache and maybe there's new onset seizures. 02:33 This is an important point pay attention to the clinical presentation understand why these would be seen because we are referring to the brain parynchema. 02:43 Pathogenesis, inactivation of p53. As soon as you have p53 there's been knocked out and really nothing that is modulating or regulating your cell cycle and so therefore the cell is allowed to remain within the cell cycle forever and so therefore may then result in increase proliferation. 03:01 Please note over expression of platelet derived group factor A or alpha, PDGF, memorize that please for astrocytoma specifically, aka gliomas and here we have adult. 03:15 You'll notice here that the astrocytoma that’s missing in adult primary brain tumor is which one? Pilocytic. 03:24 Let’s talk about the gross examination of your brain tumors. 03:32 The one that you wanna pay attention to here is what, where glioblastoma multiforme, areas are firm and white or soft and yellow areas representing your areas of necrosis. 03:43 And what's so dangerous about glioblastoma is that even when you're trying to surgically correct it there's every possibility that these will then come back and in addition, this particular neuroplastic cells would then seed, in terms of spread and by seeding we mean it is then going to pop into adjacent structures maybe perhaps even your cerebrospinal fluid. 04:10 Microscopically, fibrillary mild to moderate increase in number of glial cell nuclei, that should make perfect sense. 04:20 This is an absolute malignancy, this is an astrocytic origin and so therefore we expect nucleus-to-cytoplasm ratio to be quite high extreme activity in the nucleus. 04:33 We have nuclear pleomorphism, intervening what's known as feltwork and make sure that you memorize, GFAP. 04:42 With anaplastic, what does that mean to you? Complete chaos that’s taking place within the nuclei, so increased cellularity and nuclear pleomorphism beyond belief. Marked mitotic activity, anaplastic complete, complete, for prognosis. 04:58 And then we have glioblastoma multiforme. 05:02 You have a greater nuclear pleomorphism, I would highly recommend that you know in great detail of the microscopic feature of glioblastoma. 05:10 Increase mitotic figure with necrosis in vascular and we have perhaps endothelial cell proliferation representing your angiogenesis, glioblastoma multiforme.
About the Lecture
The lecture Neuroepithelial Tumors: Astrocytoma by Carlo Raj, MD is from the course Tumors of the CNS.
Included Quiz Questions
Which of the following is involved in the pathogenesis of astrocytomas?
- Inactivation of the p53 gene
- Inactivation of the p21 gene
- Inactivation of the PDGF-A gene
- Inactivation of the EGFR gene
- Activation of the BCR/ABL gene
Which of the following is characteristic of glioblastoma multiforme?
- Necrosis and endothelial cell proliferation
- Perivascular rosettes and rod-shaped blepharoplasts
- Spindle cells concentrically arranged in a whorled pattern
- Cystic spaces, calcifications, and "wet" keratin
- Low mitotic rate
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I'm writing this review just to thank Dr. Raj for his great lectures. Thank you!