Playlist
Show Playlist
Hide Playlist
Arthritis: Diagnosis with Case
-
Slides Arthritis ChronicCare.pdf
-
Download Lecture Overview
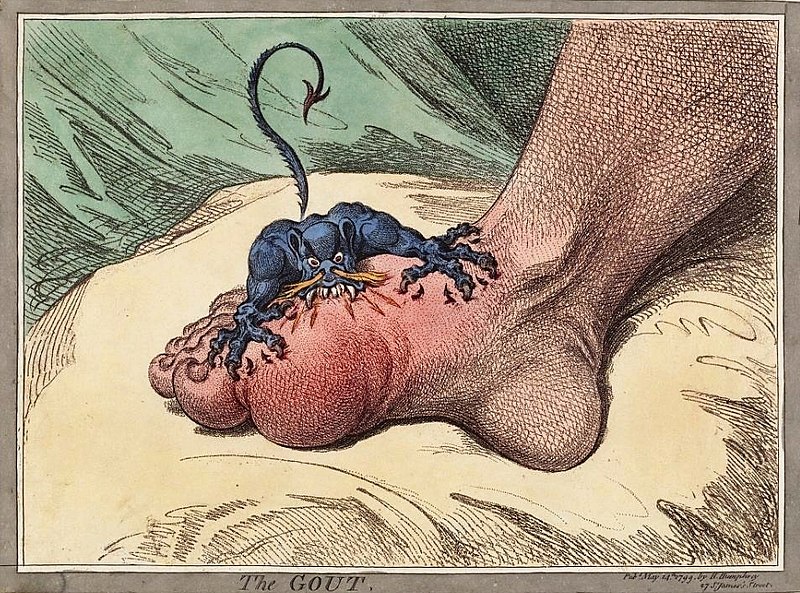
00:01 All right. 00:01 So, full disclosure. I went running this morning early. 00:05 And as my knees swelled to the size of a basketball as it does when I run, I thought, hey, I’m going to talk to the gang about arthritis today. 00:13 So, let's cover some arthritis. 00:15 And this is – I’ll try to keep my personal story out of it as much as possible. 00:19 But it’s something that all of us are going to contend with as we get a little bit older. 00:24 So, let’s talk about a case. 00:25 This is a 68-year-old woman who complains of left knee and right hip pain for the past two years. 00:30 And these have been been getting slowly worse overall. 00:35 The pain is worse in the evening or following activity. 00:38 She tried various over-the-counter analgesics with mild success in improving the pain. 00:43 Physical examination revealed some tenderness over the joints in the hip and the knee, but no calor, which means heat, no swelling. 00:51 So, what’s the most reasonable action based on this history. 00:54 Should we evaluate her hip and knee with an x-ray? How about an x-ray of her spine, hands and feet, plus her hips and knees because we’re worried about a broader arthritis? How about getting a C-reactive protein in an antinuclear antibody test just in case this is an autoimmune arthritis? Or should we just test for rheumatoid factor alone? What do you think? This patient's age, the slow onset of her symptoms in her knee and her hips specifically on opposite sides makes me think that this is very much likely to be osteoarthritis. 01:28 Therefore, we just need to start with their hip and their knee to confirm that diagnosis, with the understanding that many patients without pain at 68 years old have degenerative changes in those joints as well. 01:40 But we'll talk about the workup and how to differentiate those patients who need that workup for autoimmune arthritis versus those who don't. 01:48 She does not. 01:51 So, look at anatomic patterns first when you’re thinking about arthritis. 01:55 Where's the pain located? For things like rheumatoid arthritis, systemic lupus erythematosus, these patients are going to have pain in their smaller joints, often their hands and feet, and very importantly, this is the one that gives you symmetric symptoms. 02:12 So, it's very rare to have a patient with rheumatoid arthritis or lupus with unilateral hand pain with the other hand unaffected. 02:22 And they have other types of signs that may be associated with inflammation. 02:27 Fever is a good one. 02:28 Osteoarthritis, spondyloarthritides, they don't give you fever, for example. 02:33 Now, spondyloarthritis, including psoriatic arthritis, ankylosing spondylitis, this is asymmetric types of joints are affected. 02:41 Ankylosing spondylitis by definition affects the sacroiliac joint whereas psoriatic arthritis can affect that joint plus the smaller joints as well. 02:53 So, it's a multi-joint player. 02:55 It can really affect just about any joint in the body. 02:59 Osteoarthritis, think about those large joints. 03:01 They get affected the most. 03:02 The hips and the knees are the most common and it is asymmetric as well. 03:07 So, hopefully, just initiating a history of the patient, where they have pain, that’s going to point you to what type of diagnosis they have in terms of the arthritis. 03:17 Other patterns in terms of the pain itself, inflammatory arthritis is worse in the morning, it's a symmetric pain and it can occur even at rest whereas osteoarthritis worse with movement, worse with weight-bearing, so more with activity. 03:31 And septic arthritis, do not want to forget, although very rare, usually affects large joints. 03:37 Of course, it’s going to be asymmetric. 03:39 And this is where you get strong constitutional symptoms like fever and fatigue, but still can be difficult to diagnose, particularly if there's other things going on, maybe like a cognitive decline where patients can't really elucidate their symptoms as well. 03:55 So, first of all, with a laboratory evaluation, not everybody who comes in needs measures of inflammation, needs specific testing for a rheumatologic condition. 04:11 We overuse this testing in general. 04:14 And a lot of patients, like our case, absolutely don't need it in any way, shape or form. 04:20 Just remember that many adults have both a positive ANA and RF testing and they have zero illness whatsoever. 04:27 A few notes about some of these tests. 04:29 ANA is really helpful if it's negative. 04:31 It's not very helpful, particularly if it’s low-level positive. 04:34 When it’s negative, it almost rules out systemic lupus. 04:40 The favorites of using a SED rate or a C-reactive protein, again, most helpful if they’re negative. 04:46 But remember that 3% of patients with rheumatoid arthritis can have a normal SED rate. 04:52 Rheumatoid factor, often false positive. 04:55 It's associated with chronic infections, hepatitis, tuberculosis, but in some patients, without any reason, it's positive. 05:03 They carry a positive test even though they don't have rheumatoid arthritis. 05:07 And then uric acid, it’s frequently high even among patients without gout, particularly those who eat more cured meats, drink more beer get more uric acid. 05:20 How about other ancillary studies? Like using radiographs. 05:23 And here's our radiograph with some severe degenerative changes that you would see in rheumatoid arthritis. 05:29 So, the x-ray is really important for osteoarthritis. 05:32 That one, you can expect when the patient comes in, they’re symptomatic, you will see positive findings of degeneration right when they get their films. 05:41 Whereas in early rheumatoid arthritis, when treatment is really quite critical, when they want to initiate disease modifying treatment, the x-ray might be negative. 05:51 It takes a while. 05:53 And don't forget that really what you want you in cases of gout or calcium pyrophosphate disease or septic arthritis, you really need synovial fluid. 06:01 That's the ideal, and especially if it’s in a smaller joint. 06:05 Sometimes, it's worth thinking about using rheumatology, you will wonders with needles and drawing out small amounts of fluid to evaluate them, do the procedure of the arthrocentesis to get the diagnosis right.
About the Lecture
The lecture Arthritis: Diagnosis with Case by Charles Vega, MD is from the course Chronic Care.
Included Quiz Questions
A 72-year-old man with a history of osteoarthritis and early dementia is brought to urgent care for worsening left knee pain and swelling, fatigue and fever over the past 2 days. What is the next best step in evaluation?
- Synovial fluid analysis
- X-ray of the knee
- Serum uric acid levels
- Antinuclear antibodies
- Rheumatoid factor
Antinuclear antibody is most helpful for which of the following?
- Ruling out systemic lupus erythematosus
- Ruling in systemic lupus erythematosus
- Ruling in connective tissue disorders
- Ruling out polymyalgia rheumatica
- Ruling out connective tissue disorders
A 33-year-old woman presents to the clinic because of several weeks of bilateral hand and wrist pain and stiffness. Her symptoms are worse in the morning and become better during the day. Which of the following is the most appropriate next step in diagnosis?
- Serum markers for rheumatoid arthritis
- Hand X-ray
- Evaluation of response to bilateral wrist splint
- Aspiration of wrist joint fluid
- Lumbar X-ray
Ankylosing spondylitis characteristically involves which of the following joints?
- Sacroiliac joints
- Cervical joints
- Wrist joints
- Knees
- Small joints of the hands and feet
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |