Playlist
Show Playlist
Hide Playlist
Aortic Stenosis – Valvular Heart Disease
-
Slides Valvular Heart Diseases.pdf
-
Reference List Cardiology.pdf
-
Download Lecture Overview
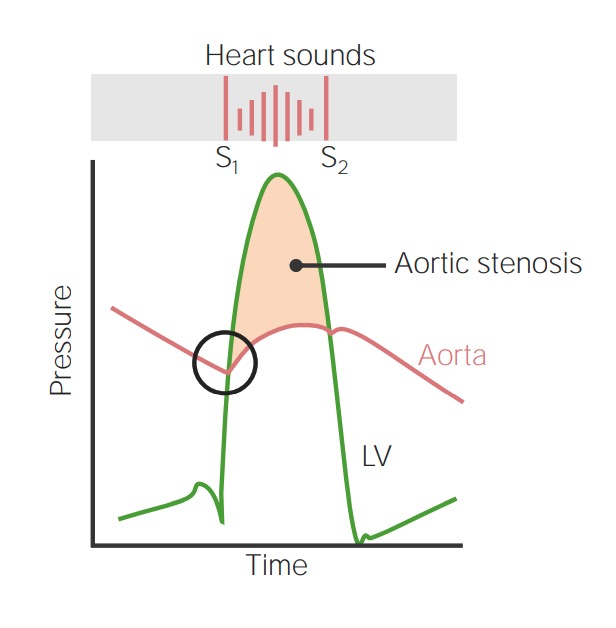
00:00 Let’s talk a little bit about the effects of aging on the aortic valve. The aortic valve is made of the similar tissue that is on the inside of arteries, the endothelium. And consequently, it should be no surprise that the endothelium can be affected by atherosclerosis. What happens is as time goes along, the aortic valve begins to thicken, it begins to get atherosclerosis in… within the leaflet and eventually, these changes can result in severe scarring of the valve usually with aortic stenosis, but occasionally, with aortic regurgitation, that is a leaking aortic valve. 00:42 Now, let’s talk again then about the etiologies or the causes of aortic stenosis. As I’ve already told you, there are, of course, congenital causes. There are two congenital causes. One is when the patient is born with an aortic valve where the valve leaflets are not separated. 01:00 This is a very severe condition in infancy. I mentioned it in the Congenital Heart Disease lecture and in fact, one has to intervene very early in these children. The pediatric cardiologist often have to put a balloon across that valve and open it, stretch it open so that the child can survive. Usually, that means an aortic valve replacement sometime in later life, late adolescence or even early adulthood. Then there’s the rheumatics, as I’ve already said, they're disappearing rapidly. Another form of congenital is the bicuspid aortic valve. I’m going to talk some more about that in a moment, but it turns out, approximately 1% of the population is born with a bicuspid. That is a valve that has two cusps instead of the normal three cusps. This puts extra strain on the valve and is real talk about eventually in most individuals, leads to either stenosis or regurgitation. 01:58 And then, the group that I’ve mentioned already which is the most common form of aortic stenosis that we see, that is the elderly who have developed atherosclerosis in their aortic valve usually causing aortic stenosis. Here’s a lovely picture done by the very famous medical illustrator, Netter. This shows the progression of both kinds of aortic valve disease. On the top, you see rheumatic valve, you can see that the edges of the valve leaflet are thickened. They fuse and eventually lead to severe aortic stenosis. At the bottom, you can see that one of the commissures that is one of the separations of a tri-leaflet valve is fused at birth leading to a bicuspid or two cusp valve and you can see that progresses also to calcific aortic stenosis. When the patient presents at surgery, you often can’t tell whether this had been a bicuspid valve or whether this was an atherosclerotic valve because the valve is so severely destroyed by fibrosis, that is by scarring and by calcification. 03:09 This shows a diagram from a demographic study from the Mayo Clinic done some years ago and you can see that what it shows you is that... so called degenerative aortic stenosis which is what they’re calling atherosclerotic aortic stenosis, is rising rapidly over the years while the bicuspid and… and particularly post-inflammatory, which is rheumatic, are declining with rheumatic declining most aggressively just as I said before because rheumatic fever is disappearing in North America and Western Europe. 03:45 This is an autopsy specimen of a patient who died with severe calcific aortic stenosis. 03:53 What you see on the right is a markedly thickened ventricle with a small cavity. In other words, there was marked left ventricular hypertrophy here and you can see on the top, the highly calcified stenotic aortic valve and I would guess, although I don’t know for sure that this was from a very elderly patient, given that that’s the kind of pathology we see in the elderly patient with severe atherosclerotic calcific aortic stenosis. 04:24 As I said before, when patients with aortic stenosis are asymptomatic, that is they don’t have any symptoms, they usually do well, but once symptoms begin to develop, then the patients usually have a high incidence of complications and often fatality. 04:43 Here is from a study done some years ago from Finland that shows you in a group of elderly individuals with either no aortic stenosis, mild aortic stenosis, moderate aortic stenosis or severe aortic stenosis. The mortality rises steeply in the moderate to severe group whereas there’s not so much mortality with time in the individuals with minimal aortic stenosis or no aortic stenosis. So, when you identify aortic stenosis in an elderly patient, it really has important implications for the prognosis or the risk of dying for that particular patient. You can see that aortic stenosis in the elderly is quite common. 05:26 Here, we see report from the United States in whites, Caucasians, in blacks and in Hispanics and you can see that it’s a little more common in women. Why is it more common in women? Because women survive longer than men and so, become more elderly and since this is a complication of atherosclerosis of the elderly, you can see why there’s a few more women than men although there’s a substantial number of men and you can see, it’s quite a substantial portion of the population who develop aortic stenosis at these advanced ages. Now, let’s talk a little bit about the clinical features. Let’s say, the patient has no symptoms, but in a routine physical exam, you hear the murmur of aortic stenosis. I think I demonstrated it to you once before. 06:19 Let me go over it with you because you can guesstimate from the physical examination how severe the aortic stenosis is. When it’s very very mild, the murmur is restricted to the earliest part of systole and as the lesion gets more severe, the murmur extends and eventually even replaces the second heart sound in very severe aortic stenosis. 06:42 Let me give you a little imitation of that. So here’s mild aortic stenosis. First let’s do the normal heart sounds - lub dub, lub dub, lub dub. Now, this is aortic sclerosis or just a little scarring or a very, very mild aortic stenosis - lub chi dub, lub chi dub, lub chi dub. As the aortic stenosis gets more severe, the murmur extends - lub chich dub, lub chich dub, lub chich dub. And now, let’s do very severe aortic stenosis - lub swoosh, lub swoosh, lub swoosh. You don’t even hear the second heart sound. Sometimes the murmur sounds... has a sort of groaning sound to it in severe aortic stenosis like this - houm, houm, houm. In any case, when you put your stethoscope on the chest and you hear something like that, you know that the patient has quite severe aortic stenosis and that’s usually confirmed by an echocardiographic study later. 07:38 The three symptoms that are of most concern is… in a patient with aortic stenosis are angina, heart failure and syncope. Syncope is the worst possible symptom. It’s due to arrhythmias and as my Professor Lewis Dexter used to say, “Syncope in a patient with aortic stenosis is a boarded sudden death,” that’s a patient very high at risk for dropping dead and needs urgent valve replacement. I’ve already gone over with you the physical findings and often, I like to play this game with the residents. I have them not tell me what the echo showed in terms of how tight the valve was and I try and guesstimate it from listening with the stethoscope. How prolonged is the murmur and how close does it come to the second heart sound which I already mentioned, demonstrates increasing severity of aortic stenosis.
About the Lecture
The lecture Aortic Stenosis – Valvular Heart Disease by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following is a more accurate description of murmur associated with aortic stenosis?
- A harsh, late-peaking systolic ejection murmur
- A systolic ejection murmur heard best at the apex
- A crescendo-decrescendo diastolic murmur heard best at the apex
- A crescendo-decrescendo diastolic murmur heard best at the base of the heart
- A constant murmur heard in both systole and diastole
Which of the following is most commonly affected by atherosclerosis?
- Aortic valve
- Mitral valve
- Pulmonary valve
- Tricuspid valve
- Interventricular septum
An infant is born with aortic stenosis due to a unicuspid aortic valve. She has signs of heart failure. Which of the following is the most appropriate treatment in this neonate?
- Balloon valvuloplasty
- Surgical valvotomy
- Surgery valvular repair
- Medical therapy for heart failure
- Close monitoring without intervention
Chronic aortic stenosis is most likely to cause which of the following complications?
- Left ventricular hypertrophy
- Right ventricular hypertrophy
- Right atrial hypertrophy
- Left atrial hypertrophy
- Thickening of the interatrial septum
Which of the following is the cause of syncope in a patient with aortic stenosis?
- Tachyarrhythmia
- Left ventricular hypertrophy
- Atherosclerosis
- Bradycardia
- Excessive vasoconstriction
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
He is such a great lecturer, demonstrating heart murmurs with his own voice better than the actual murmurs we hear through a stethoscope. That was an exaggeration but you get my point. He is fantastic.
As someone who loves neuro, cardiology is not my strong suite. These lectures have been monumental in my education. Thank you for these great explanations and examples of the heart sounds!
Such a good teacher. He makes difficult things easy. Wonderful teacher.
Amazing vocal representation of heart murmur sound! Thoroughly impressed. Easy to pay attention to voice. One of my favourite lecturers!