Playlist
Show Playlist
Hide Playlist
Aortic Dissection: Stanford Classification, Signs and Symptoms, Consequences and Diagnostics
-
Slides Aortic Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
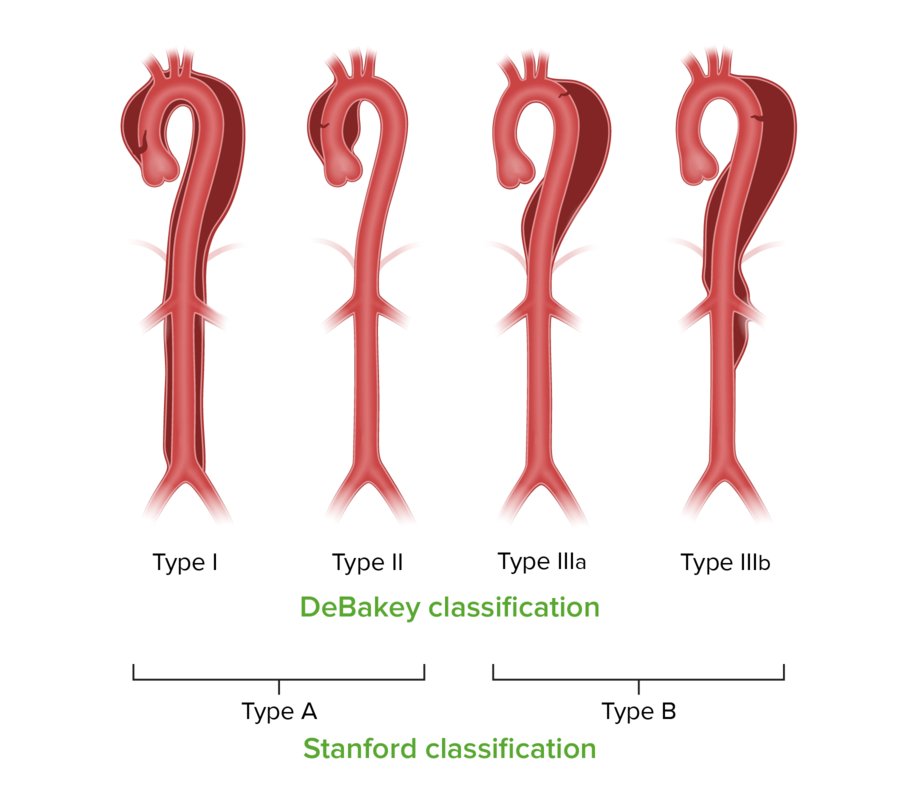
00:01 When we talk about aortic dissections, we use the Stanford Classification for the most part. 00:07 There is also something called the DeBakey classification. 00:10 Let's start with the Stanford classification which is shown here. 00:12 Stanford is divided into type A and type B dissections. 00:17 So this means that we involve if it's a type A, the proximal aorta and it may involve the distal aorta too but it doesn't have to. 00:26 Anytime we have a dissection involving the proximal aorta, above the levels or before the great vessels of the arch, that would be a type A dissection. 00:35 And then, if it involves the aorta distal to the great vessels it's called a type B dissection. 00:42 Those two distinctions type A and type B are important because type A almost always require surgical intervention. 00:49 And type B can usually not always but can usually be managed medically. 00:55 Now DeBakey from Texas, developed a slightly different system, which is not used as much anymore, but you may want to be aware of it. 01:05 And in a Type l dissection. 01:09 It's the entire aorta that has now got a dissection plane, the blood gets into the separating layers of the media and just unzippers it all the way down. 01:19 That's a Type l. 01:21 And Type ll dissections involves the ascending aorta, but it kind of stops at the great vessels. 01:27 This may be due to scarring or other things happening within the aorta. 01:32 And then Type lll is a classical Stanford Type B. 01:36 Okay. 01:38 So signs and symptoms of aortic dissection and they're mostly compression symptoms. 01:44 So if you have dissection, you have expansion of the thickness of the aorta. 01:49 In the same way aneurysms can cause dysphagia, so too, can aortic dissection. 01:55 So you can get esophageal compression associated with that. 01:58 You can get hoarseness because of impingement of a expanding aorta and impacting the left recurrent laryngeal nerve. 02:07 You can get Horner syndrome, and this is the superior cervical sympathetic ganglia, and you get ptosis on that side and you get anhidrosis and you get myosis. 02:17 So the classic Horner syndrome is ptosis, that's the eyelid drooping. 02:21 Myosis, so you get dilation constriction of the pupil, and you get anhidrosis, you don't get normal sweating on that side. 02:30 Sudden onset of severe tearing chest pain is typical. 02:34 It's typically described as a tearing chest pain that starts either in the anterior chest or starts between the scapulae in the back and then progresses to go more distally. 02:45 And it's described as severe, terrible, tearing pain as if you're being stabbed with a knife and the knife has been dragged down. 02:53 Neurological symptoms can include syncope, altered mental status, or stroke, depending on the vessels that are compromised. 03:00 Also, depending on the degree of sympathetic tone that's elicited, because of the severe pain. 03:05 Painless dissection can occur. 03:08 And in about 10% of individuals, usually with a connective tissue disorder, they may have a transient dissection that gets initially into the media, and then luckily finds its way back in to the lumen of the aorta. 03:24 When that happens, we don't have a dissection that goes all the way down aorta, it only goes for a very limited period. 03:33 Other kinds of signs and symptoms. 03:35 So patients will present with asymmetric pulses. 03:38 Again, depending on where the dissection occurs, and the compromise of vasculature, you may have more prominent bounding pulses in the right side versus the left side, or you may have differential pressure. 03:52 So if I measure blood pressure, it should be the same in the right and left arm. 03:56 And not only that, should be pretty much the same in arms as in legs. 04:00 But if there's an aortic dissection, patients will typically have normal pressure in the right limb, diminished pressure in the left limb and diminished pressures in the legs. 04:09 So asymmetric pulses or asymmetric pressures are a sign of aorctic dissection. 04:15 Tachycardia. 04:16 This is in part due to the pain but it's also because we now have blood flow that is not going to the appropriate locations. 04:24 It's in a false lumen. 04:27 And that is reflected or is felt by the heart as diminished volume. 04:34 So you can get tachycardia. 04:36 You can get a murmur of aortic insufficiency or aortic regurgitation, and that's when you get dilation of the aortic root due to the dissection plane. 04:47 That aortic regurgitation murmur is in a typical location for the aortic valve left of the sternal border. 04:54 And it's usually a very soft, high-pitched, early diastolic decrescendo murmur. 05:00 You also have wide pulse pressures. 05:02 What does that? Well it actually means that the pressure differential which is normally 120 mm of mercury systole versus 80 mm of diastole, that pulse pressure is 40 mm of mercury. 05:15 When the aortic valve is regurgitant, now that pressure rapidly runs off, so you will have a peak of 120 and a bottom sometimes a 40. 05:26 So, you have a widened pulse pressure. 05:30 And on X-ray you can see sometimes not always and you shouldn't count on it. 05:35 But you can see a widen mediastinum and a very prominent aortic knob, and this is because of expansion of the aorta. 05:46 Other signs and symptoms depend on where the dissection plane goes and depending on what vessels are compromised by the movement of blood in the media, you can have diminished or absent peripheral pulses in one or more extremities. 05:59 The tissue in that area may be very pale because you're not perfusing it. 06:03 You may have pain associated not only with the primary dissection, but with the relative ischemia of a particular tissue. 06:10 You may also have abnormal paresthesias, a tingling sensation because the nerves are not being perfused and are not working. 06:17 And normal thermal regulation may be compromised depending on again where the dissection is happening. 06:23 You may get motor deficits affecting the nerves, but also because of ischemia of the tissue. 06:31 Long term not longer term but important, almost immediate consequences. 06:35 So depending again on where the dissection plane goes, if it goes retrograde into the pericardial sac. 06:42 You will have hemopericardium, which is demonstrated here. 06:46 That pericardial sac is tense filled up with blood, the oxygenated blood from a patient who had an aortic dissection that travelled retrograde got into the pericardial sac and quickly within about 10 sec, filled up with 250 cc's of blood and the patient died of cardiac tamponade. 07:06 You can also have retrograde dissection around the coronary arteries that are coming off the ascending aorta, in which case that dissection may compromise the flow of the coronary arteries giving rise to a myocardial infarct. 07:19 You can have rupture of a dissection into the thorax, hemothorax and exsanguinate into your thorax, or exsanguinate into the peritoneum. 07:28 Or if you're really really lucky, you have a dissection, and then it finds its way back into the lumen, the normal lumen of the aorta and all you end up with is a double-barreled aorta with a true lumen and a false lumen where you had the dissection but you were lucky and it came back instead of going out. 07:50 Diagnostics for this and basically that's going to be an echocardiogram or CT angiogram. 07:57 So computer tomography takes longer and by introducing dye you potentially — depending on how the dye is installed — you may or may not actually make the dissection worse. 08:10 So echocardiogram is probably the diagnostic imaging of choice that can be done very quickly at bedside. 08:20 The important thing is to be able to tell the surgeons where is the intimal flap. 08:25 Where is the blood entering this defective media and where's the dissection starting? Because the surgeon needs to know that so that when he or she goes in, they can make sure that flap is closed off. 08:38 X-ray is used. 08:39 X-rays, simple chest X-rays are relatively insensitive and not useful but CT, computerized tomography angiography such as what is shown here can also be very, very helpful. 08:52 The laboratory workup is basically looking for evidence of activation of the coagulation pathway. 08:58 So you look for D-dimers. 09:00 So if a patient has the right kind of symptomatology in terms of a tearing acute onset chest pain. 09:06 Unequal pulses, a flap that you can demonstrate by echocardiogram and a positive D-dimer. 09:11 They've got an aortic dissection, you need to get them to the operating room as soon as possible. 09:16 And with that, we conclude our discussion on dissections and aneurysms.
About the Lecture
The lecture Aortic Dissection: Stanford Classification, Signs and Symptoms, Consequences and Diagnostics by Richard Mitchell, MD, PhD is from the course Aortic Disease.
Included Quiz Questions
Which type of aortic dissection involves only the ascending aorta?
- Stanford Type A, DeBakey type II
- Stanford Type A, DeBakey type I
- Stanford Type B, DeBakey type IIIa
- Stanford Type A, DeBakey type IIIb
- Stanford Type C, DeBakey type I
Which of the following symptoms is consistent with Horner syndrome?
- Anhidrosis
- Hyperhidrosis
- Astigmatism
- Dysphagia
- Diplopia
What is the most common symptom of aortic dissection?
- Sudden tearing chest pain
- Gradual tearing chest pain
- Sudden pleuritic chest pain
- Gradual pleuritic chest pain
- Sudden tearing back pain
What is a classic finding on chest radiographs in aortic dissection?
- Widened mediastinum
- Lobar consolidation
- Atelectasis
- Left atrial enlargement
- Pleural effusion
What is a rapid, lethal complication of a retrograde aortic dissection?
- Hemopericardium
- Acute limb ischemia
- Myocardial infarction
- Renal insufficiency
- Pleural effusion
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |