Playlist
Show Playlist
Hide Playlist
Aortic Dissection: Pathogenesis
-
Slides VascularDisease CardiovascularPathology.pdf
-
Download Lecture Overview
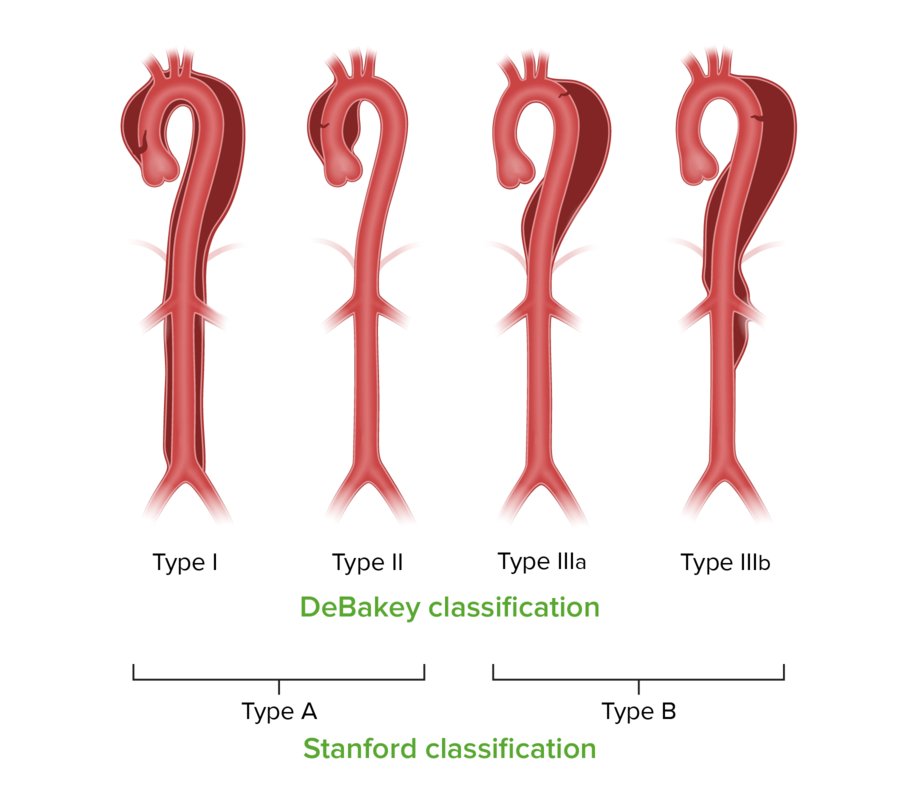
00:00 Now, let us take a look at aortic dissection. 00:03 Now, we have completed peripheral vascular disease, we have walked through venous insufficiency and we also talked about peripheral arterial disease. Let us take a look at aortic dissection. 00:13 What does that mean to you? It means that literally the aortic, now what I'd like for you to do is come out of the left ventricle, come out of the aortic route, come through the ascending aorta, the arch and then thoracic, stope there, please. Why? Because clinically speaking there are two major dissections, these are called Stanfords. And it is important that you know the exact location of that aortic dissection. I had you stop at thoracic aorta. Are you picturing this? And the two major components would be the ascending part of the aorta or the thoracic aorta. Are you picturing it? Good. These are the two places where, if the aortic dissection was to take place, you will then call it either Stanford type A, A for ascending aorta or Stanford type B as in thoracic aorta, distal aortic dissection. Is that clear? Now, what are some of the predisposing factors for developing an aortic dissection? Well let's take a look. It is an emergency, stabbing back pain because there is an actual dissection. The pressure dissected right through the aorta during the dissection, the lining of the aorta, the intima tears and so now the intimate most is the innermost, the middle portion is the media, m and m. Those are the two layers that I want you to pay attention to specifically. Those are going to tear and when they do so this is not a good situation. You might have blood which then does what? Well they'll rob the blood from the subclavian, it will lead the blood perhaps back proximally into the pericardial cavity, may result in cardiac tamponade. Sudden rush of blood, isn’t this cardiac tamponade? Of course, it is. Is this an emergency? Yes, it is. What do you want to do? Remove. Surgery is what you are thinking. Risk factors include. This should make sense to you. There is too much blood pressure, excessive hypertension. Over a period of time, it might cause complete rupture and dissection. Marfan, you pay attention to "f" in Marfan. 02:42 Who is your patient with Marfan? Think about Abraham Lincoln as an example of a typical patient with Marfan. Tall, lanky, you have your fingers that are quite elongated like a spider, arachnodactyly. May be visual disturbance because the f in Marfan is coding for the fibrillin gene with chromosome F-15 which is then coding for what part of your tissue? Elastin. So this elastic tissue is not present, suspends your ligament that places or holds the lens in place, not there. Dislocation, subluxation of the lens. So that is your patient with Marfan. 03:35 Go into aorta, what happens? Either the is thoracic aorta or the ascending portion in which the elastic tissue is not present what happens? You are now prone to a dissection. 03:48 But before that, what then happens? A cystic medionecrosis. It mean to say that the media which is what portion of the blood vessel? The middle portion of the aorta specifically, will undergo necrosis in which you will form a cyst like a cavity. If that is not properly identified and corrected you are worried about a dissection, which was which again? Stanford type A. 04:13 A is an ascending. Stanford type B would be the thoracic aorta dissection. 04:20 Atherosclerosis risk factors. Ehlers-Danlos. What do you know about this? Deficiency of collagen depending as to which type and then coarctation of the aorta. How much pressure is there in coarctation of aorta? "Well Dr. Raj, you didn’t tell me where." I understand that. 04:38 If it is distal you don’t have enough pressure, but proximally what you have done? You have introduced a resistor in a series. What happens to the pressure proximal to the resistor? Increased. That is where the problem is, Too much pressure there, are you prone to dissection? Yes, you are.
About the Lecture
The lecture Aortic Dissection: Pathogenesis by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following statements regarding aortic dissection is FALSE?
- Stanford type B aortic dissection may involve the aortic arch.
- Aortic dissection is due to a tear in the tunica intima.
- Aortic dissection may result in cardiac tamponade.
- Stanford type B aortic dissection may involve the abdominal aorta.
- Stanford type A aortic dissection may involve the aortic arch.
Which of the following is NOT a common risk factor for aortic dissection?
- Aortic stenosis
- Atherosclerosis
- Ehler-Danlos syndrome
- Coarctation of the aorta
- Hypertension
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |