Playlist
Show Playlist
Hide Playlist
Anticholinergic Drugs
-
Slides Anticholinergic Drugs.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
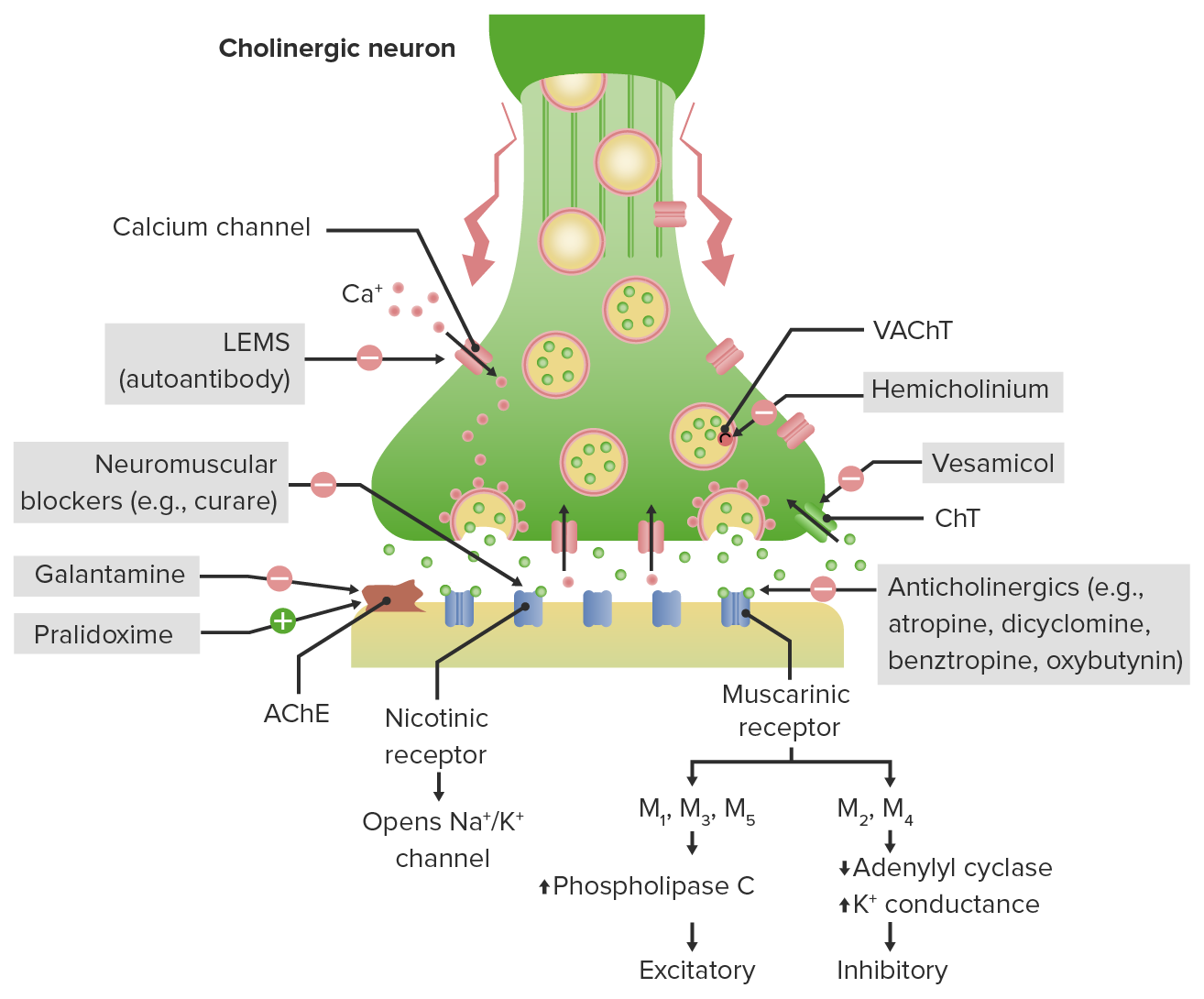
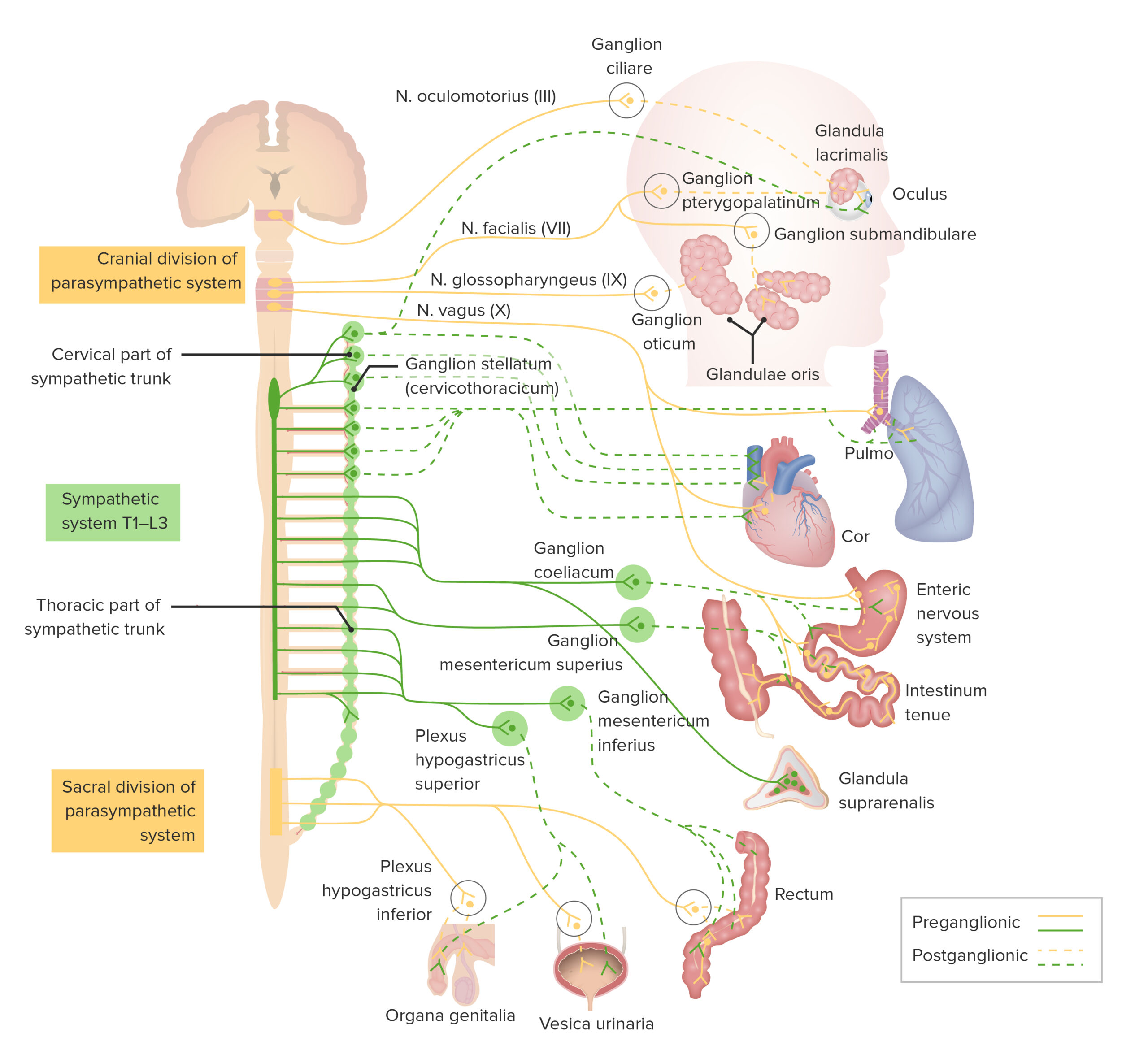
00:01 Let's move on to anticholinergics. 00:04 Cholinergic receptor antagonists can be anti-nicotinic and these are ganglion blockers, neuromuscular junction blockers. 00:15 Let's talk about the ganglionic neurons remember I was telling you that, gangs go out in smoke so ganglionic neurons are nicotinic. 00:24 Let's move on to the smooth muscle and neuromuscular neurons. 00:28 Now, the smooth muscle neuromuscular neurons are muscarinic. 00:36 The other types of end organs are sweat glands which are also muscarinic. 00:42 How do I remember that? Musky smell, means, sweat and muscles, so that's how I tend to remember, That smooth muscle and neuromuscular neurons are muscarinic. 00:56 What are these antagonists? Anti-muscarinic antagonists, the non-selective one is atropine, I already told you that it's used as an antidote in sarin gas exposure. 01:08 It's also used in cardiac codes, the M1 selective antimuscarinic drug. 01:14 Now drugs ending in “oxime,” like pralidoxime are cholinesterase regenerators. 01:22 We spoke before about cholinesterase inhibitors, this is where the double negative comes in the central nervous system. 01:30 A cholinesterase inhibitor, inhibits the enzyme that breaks down acetylcholine. 01:36 So, a cholinesterase inhibitor increases the amount of acetylcholine. 01:44 A cholinesterase regenerator increases cholinesterase, so, you reduce the amount of acetylcholine in the synaptic cleft. 01:55 So, pralidoxime and other drugs in its class will act on that synaptic cleft to cause that effect. 02:06 Okay, we also use anti-muscarinic agents in Parkinson’s disease. 02:11 Benztropine, biperiden, triphenidyl, these are drugs, that we're going to talk about later. 02:16 We use scopolamine in motion sickness. 02:20 It's available as a pill or patch, most people know what a scopolamine patch is. 02:24 It's a very effective anti-nauseant. 02:28 And one other thing that I think you need to remember for when you're on the wards, is benztropine. 02:33 Benztropine is an antidote to acute dystonia, where people are contracted and unable to move and they often will have their head turned to one side as far as it'll go. 02:45 So benztropine is an antidote to that. 02:47 We're going to cover that in a later lecture as well. 02:50 What are the effects on the eye? Anti-muscarinic agents cause dilation, okay. 02:59 Atropine acts over 72 hours, homatropine acts over 24 hours and this one acts over 30 minutes. 03:10 Now atropine is derived from the belladonna plant, which I have illustrated here. It's a tertiary amine, it's lipid soluble, it does cross the blood-brain barrier and its duration of action is around four hours. 03:26 In the lung, anticholinergics, cause mild bronchodilation. 03:30 So, the prototypical drug for the lung is ipratropium, it's also known as atrovent. 03:36 So atrovent is the green inhaler. 03:38 The other bronchodilators like tiotropium are also available and are really making a huge impact on respiratory therapy. 03:47 We're going to be talking about that in our respiratory pharmacology lecture. 03:52 There is also a mild reduction in airway secretions. 03:56 Atropine can sometimes be used as a direct agent, when you're trying to intubate somebody and they have tons of mucous secretions and you can't see where you're going with the intubation instrumentation. 04:08 We've also used it, I’ve also used it personally, when I’m doing bronchoscopies, because it does reduce airway secretion. 04:17 Okay, what about the effect on the gut it's an anti-muscarinic agent. 04:22 Old treatments for peptic ulcer disease, we no longer use them. 04:25 I just mentioned them here for your own interest, it is not going to be on an exam and it's not a big part of our thought processes anymore. 04:35 In terms of the urinary tract, anti-cholinergic effects reduce urgency and mild cystitis and overactive bladder syndrome. 04:44 These are the various drugs that we have available. 04:47 They're very commonly used in nursing homes. 04:50 It's worthwhile knowing these drugs when you get out into practice. 04:54 Unfortunately, we use the trade name so much, that the generic names kind of fallen by the wayside and it's because they sound so much like they would relieve urinary symptoms and they are listed here. 05:09 Okay, what about toxicity. 05:12 So, what happens if you take too many anticholinergics. 05:16 We call this anticholinergic crisis and this is a very old saying and patients are dry as a bone, hot as a pistol, red is a beat and mad as a hatter. 05:27 So, patients who are dry, have what we call, “Atropine fever.” They're very dry, they're very warm, they've lost the ability to properly thermoregulate. 05:37 They're “Red as a beat,” because they have peripheral vasodilation and “Mad as a hatter,” they will have psychosis and very bizarre kind of behavior. 05:50 Treat anticholinergic toxicity with physostigmine. 05:55 That is the antidote for that type of toxicity. 06:00 Well, there you have it, we did a very difficult topic, I think you guys are great to have lasted until the end of this lecture. 06:06 This is the kind of stuff that does show up on exams, so, if you want to watch this lecture again, I do encourage it. 06:13 I found it difficult when I was studying, so, I tried to make it as easy as possible and we do have some questions for you, so, I encourage you to do practice questions in this, so, that when you get to your exam, you'll nail it. 06:25 Thank you very much.
About the Lecture
The lecture Anticholinergic Drugs by Pravin Shukle, MD is from the course ANS - Pharmacology.
Included Quiz Questions
Receptors in the autonomic ganglions are mainly of which type?
- Nicotinic cholinergic
- Muscarinic cholinergic
- Nicotinic adrenergic
- Muscarinic adrenergic
- None of the options provided is correct.
What best describes hexamethonium?
- Nicotinic receptor antagonist
- Dopamine receptor antagonist
- Muscarinic receptor agonist
- Nicotinic receptor agonist
- Muscarinic receptor antagonist
Which receptor is typically present in the neuromuscular junction of skeletal muscles?
- Nicotinic
- Adrenergic
- Muscarinic
- Dopaminergic
Which receptors typically occur in the brain, heart, and smooth muscles and mediate parasympathetic activity?
- Muscarinic receptors
- Nicotinic receptors
- Alpha adrenergic receptors
- Dopaminergic receptors
- Beta adrenergic receptors
Which medication is commonly used in the acute treatment of dystonic reactions?
- Benztropine
- Phenylephrine
- Doxycycline
- Betamethasone
- Clonidine
What is NOT a side effect of atropine?
- Diarrhea
- Decreased airway secretions
- Dry mouth
- Pupillary mydriasis
- Anhidrosis
Which medication may be used to treat anticholinergic poisoning?
- Physostigmine
- Benztropine
- Atropine
- Phenytoin
- Dexamethasone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Just what is needed for the clinics and exam Bare minimum leads to better retention and the results.
1 customer review without text
1 user review without text