Playlist
Show Playlist
Hide Playlist
ANCA-associated Small Vessel Vasculitides
-
I Rheumatology 05 Vasculitis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
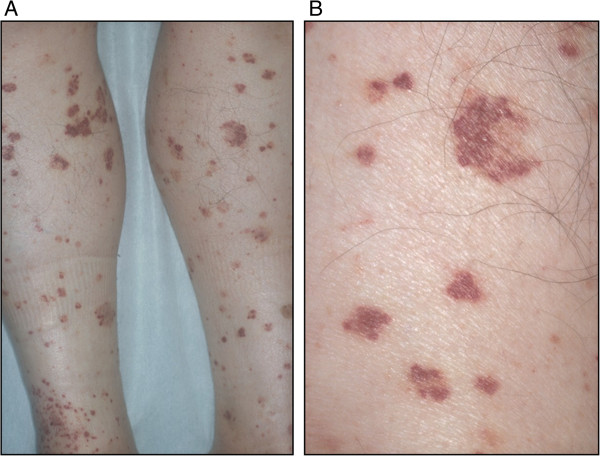
00:01 Next, we’re moving on to small vessel vasculitides. 00:05 Under small vessel, the way that we way will divide this is ANCA and non-ANCA association. 00:11 ANCA stands for antineutrophil cytoplasmic antibody, as we shall see, and there it is. 00:16 Please make sure you know what ANCA stands for—antineutrophil, or neutrophil, cytoplasmic antibody. 00:23 There are 2 major types of ANCA’s that we shall take a look at. 00:26 You probably have gotten accustomed to seeing both p- and c-ANCA. 00:30 You will no longer call it that. 00:33 You will know that p in ANCA stands for? Perinuclear. 00:37 And as we shall see, this p-ANCA, and now called MPO-ANCA, in other words myeloperoxidase; whereas if it’s c, c-ANCA, that c stood for cytoplasmic we, however, are now calling it with the third letter of the alphabet, A-B-C, yeah. C. 00:52 So PR3-ANCA, proteinase 3, as we shall see. 00:57 The manifestations, small vessel, and let’s say that it’s cutaneous blood vessels, skin manifestations. 01:05 Muscles and nerves could be affected. Lungs, big time, and therefore, we know what we used to call Wegener, which now we will call, technically, granulomatosis with polyangiitis. You’ve heard of hemoptysis—lungs, you also have hematuria—damage down to the glomerulus. 01:24 Here, we’ll take a look at ANCA-associated vasculitides, and here they are. 01:29 There are 2 forms—I’m going to walk you through this step-by-step so that, once and for all, this is firmly planted in your head. 01:37 First, the p in p-ANCA stands for perinuclear. 01:42 The c in c-ANCA is cytoplasmic. 01:47 Now we have to get more detailed. 01:49 The p in p-ANCA is MPO positive or myeloperoxidase. 01:57 Lots of p’s there to help you out. 01:59 I’m going to give you an example of what’s p-ANCA positive or PR3-ANCA versus your MPO-ANCA. 02:06 MPO-ANCA would be something like, you’ve heard of eosinophilic granulomatosis polyangiitis. 02:14 We’ll talk about Churg-Strauss, or microscopic polyangiitis (MPA). 02:20 Don’t worry, that’s to come. 02:23 Whereas, if it was c-ANCA, I’d like to remember this as being the third letter of the alphabet, or PR3. 02:30 PR stands for proteinase. 02:33 An example for this, of c-ANCA or PR3-ANCA, granulomatosis polyangiitis. I need you to get in the habit of knowing that it was formerly called Wegener. 02:43 We now call it GPA or granulomatosis with polyangiitis. 02:49 Now these are the antibodies that are thought to be pathogens in these vasculitides of the small vessel. 02:56 We often times call these ANCA-associated pathologies Pauci-immune. 03:05 Perhaps, you’ve asked yourself what does that even mean. 03:08 Pauci means little, okay, by definition. 03:13 So could there be immune involvement in these ANCA-associated pathologies? Absolutely, but is a significant no. 03:21 So it’s either non-immune or, technically, little immunity involvement meaning Pauci immune. 03:28 Whereas, let me give you an example or a pathology for comparison. 03:33 Henoch-Schönlein purpura is a pure immune complex small vessel disease. 03:41 But let’s first complete our discussion of ANCA-associated vasculitides. 03:45 Our first one is granulomatosis with polyangiitis. 03:48 I’ve mentioned this a few times now. Formerly called Wegener. 03:52 Now whose the patient walking through the door? A young patient? Sure. 03:56 And you take a look at their nose and it looks like something that you want to get on a horsy. 04:02 What do I mean? Saddle nose. Literally, there’s going to be necrotizing destruction. 04:06 You see my ugly nose with the septum here? Well the nasal septum could then be destroyed and necrotized. 04:14 And when it does, it takes on a saddle type. 04:17 In other words, a depression as I shall show you. 04:20 Now, you want to divide the issues in the lung for GPA into 2 parts. 04:28 These are the 2 parts that you must know. 04:31 I want you to first predict, and then I’m going to show you, so pay attention. 04:35 We have, #1: Recurrent sinusitis, so that will be the upper parts of the airways. Recurrent sinusitis. 04:44 #2: In the lower parts of the lung that could be affected, the patient is now presenting with hemoptysis. 04:53 Please know those 2. 04:55 Thirdly, small vessels down in the kidney may also be affected and now the glomerulus is undergoing necrotizing type of destruction. 05:04 So when the glomerulus gets completely necrotized guess what’s passing through there easily? Blood. Hematuria. 05:11 So we’ve got hematuria, hemoptysis, and sinusitis. 05:14 Let’s take a look at clinical manifestation. 05:17 We have recurrent sinusitis #1, #2 I told you about hemoptysis, and hematuria. 05:24 Those are the 3 that you’re taking out of the clinical manifestation. 05:28 In addition, you’ll have new ear tubes, elderly patients meaning granulomatosis polyangiitis. Look for that as a possible clue either when the patient is walking through the door or you’re reading about this patient. 05:44 In addition, I told you about the nasal septum and might undergo necrotizing destruction, we call this saddle nose. What does a saddle mean? Saddle of a horse; depression. 05:55 And skin issues, oftentimes, purpura. 06:00 Diagnostic study: Remember it used to be called c-ANCA but now we call it PR3-ANCA, and what is PR3? Or what does PR stand for? Proteinase. 06:11 On biopsy, what are you going to find? Look at the name. Granulomatosis. 06:16 Not exactly sure? There are a couple of theories out there as to what’s causing granuloma, but you do. 06:22 You have to find granulomas and there will be pulmonary hemorrhage, and Pauci-immune. There you have it. What’s Pauci mean? Little. 06:30 And GN stands for? Glomerulonephritis, giving you the hematuria. 06:34 Those are some of the diagnostic tools that you must find, most importantly the PR3. 06:39 Management: Well, you use cyclophosphamide to induce yes, cyclophosphamide to induce and methotrexate to maintain. 06:49 In addition, you have steroids and got plasmapheresis, and ultimately—be careful though, the cyclophosphamide, for organs that are threatened by the disease itself. 07:03 Our second major ANCA-associated issue here is clinically indistinguishable from granulomatosis with polyangiitis. 07:10 Clinically indistinguishable. 07:12 There are a couple of things here that I wish to point out to you to make your life a little bit easier. 07:17 The granulomas might not be as prevalent. The granulomas that you find in granulomatosis with polyangiitis, and if you don’t mind, I’m going to start calling it GPA. 07:26 But the granulomas that you find in GPA are not as prevalent in MPA. 07:32 You’re going to take this MPA when we get into diagnostic column here. 07:37 It will be positive for MPO-ANCA. 07:41 What ANCA was positive in GPA? PR3-ANCA. 07:46 So right off the bat, I’m giving you some clear distinctions of how you can differentiate between GPA and MPA. 07:57 Identical clinical manifestation; however, the granulomas are not going to be as pronounced in MPA, if at all actually. 08:06 MPA, microscopic polyangiitis, is MPO-ANCA. 08:11 It used to be called p-ANCA myeloperoxidase. 08:16 And biopsy most likely will not show granuloma. Is that clear? I couldn’t emphasize that enough. 08:24 Management here, pretty much on the same token as your GPA including your plasmapheresis, and once again, cyclophosphamide. 08:37 Continued discussion of ANCA-associated small vessel vasculitides. 08:42 We have our third most common or the one that often appears, would be eosinophilic granulomatosis with polyangiitis. 08:51 Eosinophilic is what you’re going to focus on. 08:55 None of the other, the other ANCA-associated pathologies which, what were they again? GPA and MPA. 09:03 Isn’t it nice to actually have something that you can abbreviate and know what it means? So we have GPA and your MPA. 09:10 In both of those clinical manifestations and diagnostic tools, we did not—did not, point out any eosinophils. 09:17 So as soon as you start seeing eosinophils, and you’re thinking about issues with ANCA’s, then eosinophilic granulomatosis, used to be called Churg-Strauss, should come to mind. 09:29 So now as soon as you think about eosinophils, and how is the patient going to present most commonly? Asthma-like. 09:38 Bronchospasm type of issues. Correct? So elderly patients with new onset asthma. 09:46 So look for bronchospasms. Allergies. 09:50 That should be clear now that eosinophilic granulomatosis is completely different from its clinical manifestation of both MPA and GPA. 10:01 Diagnostic tools: We have eosinophilia. 10:05 A chest x-ray might be abnormal. 50% of your patients will then be MPO-ANCA positive. 10:11 So then you have 2 conditions which we have MPO being positive, what are they again? MPA, microscopic polyangiitis, and eosinophilic granulomatosis. 10:22 On surgery, lung biopsy is Gold standard and here you would find your eosinophilic infiltration. 10:28 Look for that, look for that, look for that. 10:30 Management here, steroids would be the most common, cyclophosphamide to protect those organs that are threatened by the disease. 10:42 What you’re looking at here is a manifestation called leukocytoclastic vasculitis. 10:48 It might be seen with eosinophilic granulomatosis. 10:56 The picture on the left—we’re getting closer to our description of other vasculitides. 11:02 The picture on the left is showing you purpuric rash. 11:06 Now what purpura means to you is the fact that there is vasculitis taking place in which there is a leakage of blood from the blood vessel and; therefore, appearing as a rash. Purpuric. 11:17 Not petechiae but purpuric. Purpura is a little bit bigger, isn’t it? Later on, we’ll talk about purpura when we officially enter and we’ve left ANCA-associated and go into our non-ANCA-associated, and well this is a patient’s leg who’s a little bit older. 11:38 If later on I give you patient’s leg or you’re given a child’s leg with purpura, then you should be thinking about anasarca purpura. 11:47 But here, this is GPA. Granulomatosis polyangiitis. 11:51 Remember, you can have little blood vessels and you can have purpura Absolutely. Be careful. 11:56 So you want to observe the background of who this patient is; where do you think this patient is coming from, age so on and so forth, and you can tell a lot. 12:08 The patient on the right, the arrow is pointing to a depression of the nasal septum. 12:14 What happened in granulomatosis with polyangiitis? That’s your saddle nose. There is necrotizing destruction of the nasal septum and a depression that I was talking to you about earlier. 12:26 Also manifestation of granulomatosis with polyangiitis, but could you also find it with MPA? Yes you can. Remember, clinically indistinguishable. 12:36 If by chance these are the pictures of MPA, how would you distinguish this from your GPA? Help me out. 12:44 #1: What kind of ANCA would you find in MPA? MPO. Good. 12:50 What kind of ANCA would you find in GPA? PR3. Good. 12:56 Next, what if you were to do a biopsy on this patient and you did not find granuloma? Then which one would it be? Microscopic polyangiitis. 13:07 If you did do a biopsy on a patient and you did find granuloma, then it would be GPA. Clear? If not, make sure you come back and review to this point in your head mentally, distinguish between the 2 conditions of GPA and MPA.
About the Lecture
The lecture ANCA-associated Small Vessel Vasculitides by Carlo Raj, MD is from the course Vasculitis: Basic Principles with Carlo Raj.
Included Quiz Questions
A 54-year-old man presents with hematuria, hemoptysis, and sinusitis. He has no history of a serious illness and takes no medications. Laboratory studies are positive for anti-neutrophil cytoplasmic antibodies (ANCA). Which of the following conditions is the most likely diagnosis?
- Granulomatosis with polyangiitis
- Takayasu arteritis
- Giant cell arteritis
- Polyarteritis nodosa
- Eosinophilic granulomatosis with polyangiitis
PR3-ANCA (anti-neutrophil cytoplasmic antibody) is most characteristic of which of the following diseases?
- Granulomatosis with polyangiitis
- Polyarteritis nodosa
- Churg–Strauss syndrome
- Rapidly progressive glomerulonephritis
- Henoch–Schönlein purpura
Which of the following is NOT a typical drug in the induction and/or maintenance therapy of granulomatosis with polyangiitis?
- Heparin
- Glucocorticoids
- Methotrexate
- Cyclophosphamide
- Rituximab
Which of the following statements regarding granulomatosis with polyangiitis is FALSE?
- Renal involvement is more common than upper airway involvement.
- PR3-ANCA (anti-neutrophil cytoplasmic antibody) is positive in the majority of patients.
- Renal biopsy often demonstrates a pauci-immune glomerulonephritis.
- Small vessels are most commonly affected.
- There can be necrotizing destruction of the nasal septum.
A 70-year-old man presents with vasculitis of the lungs and kidneys without significant upper airway involvement. Myeloperoxidase-antineutrophil cytoplasmic antibodies (MPO-ANCA) are positive, but PR3-ANCA is negative. Biopsy reveals pauci-immune glomerulonephritis without granulomas. Which of the following is the most likely diagnosis?
- Microscopic polyangiitis
- Granulomatosis with polyangiitis
- Goodpasture syndrome
- Polyarteritis nodosa
- Eosinophilic granulomatosis with polyangiitis
Which of the following markers is most frequently present in a patient with microscopic polyangiitis?
- Myeloperoxidase-antineutrophil cytoplasmic antibodies (MPO-ANCA)
- Proteinase 3-antineutrophil cytoplasmic antibodies (PR3-ANCA)
- Anti-double stranded DNA
- Anti-centromere antibodies
- Anti-cyclic citrullinated peptide
What is the most likely diagnosis in a patient with a history of drug-resistant asthma, recent pulmonary infiltrates and hemoptysis, mononeuritis multiplex, palpable purpura, and peripheral blood eosinophilia?
- Churg–Strauss syndrome
- Granulomatosis with polyangiitis
- Microscopic polyangiitis
- Takayasu arteritis
- Asthma
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
I always know its going to be a good lecture when I see Dr. Raj teaching it
Mehmet K, and others thank you for your feedback! I hope this message finds you and your loved ones safe in 2021. I read your comments, and try to deeply reflect upon them. I thoroughly enjoy the feedback that I receive from you the medical students and doctors, fore; it allows me to improve upon the art that I have been fortunate enough to be part for the past 20 years. Thanks to individuals such as you who take the time out of your busy schedule to express what is on your mind, it allows me to always be improving as a medical educator. There are numerous other resources out there, as you are aware, and I feel privileged that you wish to invest your time and money with me and Lecturio. As any patient should receive 2nd and 3rd opinions about treatment protocol, and even encourage such behavior by doctors who are secure in themselves, I would recommend the same for you so that you are constantly being fed and inspired by medical knowledge! You live in golden age of medical education and possess tools at your disposal to excel in your medical school coursework, USMLE/PLAB/MER, etc. I hope you find a resource that you can relate to, if it's me, fantastic, if not, that's okay too, but the most important thing is that you/me, WE, continue on our journey of growth and humility. Thank you all for making me a part of your academic life, however brief it may be. ~Carlo Raj
this doc has a disgusting accent and teaching method. weird jokes and attitudes. if lecturio would like to improve itself, the very first thing is to sack this man and find a proper lecturer like anesthesiologist one.