Playlist
Show Playlist
Hide Playlist
Anatomy of the Testes
-
Slides Anatomy of the Testes.pdf
-
Reference List Anatomy.pdf
-
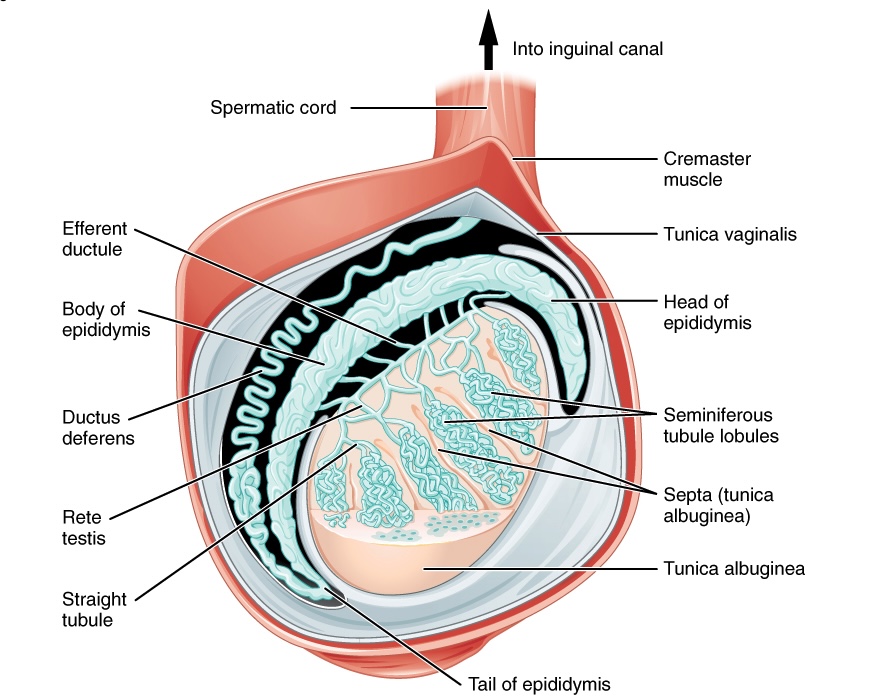
Download Lecture Overview
00:01 In this video, we're going to start looking at the male reproductive organs with the testes. 00:08 So here we can see the male reproductive system and we have some important structures here. 00:13 We can see at the bottom of the screen. 00:15 We have our two testes. 00:17 Either side of the penis, which we can see anteriorly. 00:20 We can also remind ourselves of the pubic symphysis we can see and the bladder. 00:25 So here we can see our two testes, which would be enclosed within the scrotal sac. 00:30 So really, these are suspended outside of the various body cavities. 00:34 And that's to help reduce the temperature of the testes to optimize spermatozoa production. 00:40 Emanating away from each of the testes. 00:42 We have the epididymis position on the posterior superior aspect of each of these testes. 00:48 And then they give rise to the Vas or the ductus deferens. 00:51 Some textbooks may call it the vas deferens, but traditionally we call it the ductus deferens. 00:57 Each of these tubes emerging away from each testi to pass into the abdomen, and then the pelvic cavity. 01:04 They enter into the abdominal cavity via the inguinal canal. 01:07 We'll come back to that in a moment or two. 01:09 If you haven't already, then you probably should go and look at the anterior abdominal wall lecture because that talks about the inguinal canal in more detail there. 01:19 So the ductus deferens is passing away from each of the testes. 01:22 They enter into the pelvic cavity, and they pass over the superior surface of the bladder and then onto the base of the bladder. 01:29 You can see them associated with the ureters and then running next to them we have a pair of seminal vesicle. 01:36 And these helped to produce the semen, a very fructose rich lubricating fluid that helps the sperm to pass from the penis into the vagina, and then into the uterus. 01:48 and the fructose there helps the highly mobile spermatozoa the mitochondria in there have sufficient energy and ATP to carry on their journey through the vagina and then into the uterus. 02:01 So the semen produced by the seminal vesicle is really important. 02:05 It also has a slightly alkaline pH which helps to neutralize some of the acidic urine that is within the urethra as it passes through the penis. 02:14 But we can also see that the seminal vesicles connect to the urethra via the ejaculatory duct. 02:20 These pass through the substance of the prostate to then enter into the urethra. 02:25 We'll look at this in more detail in the next slide or two. 02:28 We also need to pay attention to the bulbo-urethral glands. 02:32 These are a pair of glands either side of the urethra. 02:35 They're analogous to the Bartholin's glands in the female. 02:38 And these produce what's known as the pre-ejaculate. 02:41 So before ejaculation of the spermatozoa from the penis into the vagina. 02:47 This pre-ejaculate is a heavily alkaline fluid that runs through the penis in advance of the sperm within the semen and that helps to neutralize the acidic environment that the urine left behind within the penis. 03:01 So the bulbo-urethral glands are really important in producing that pre ejaculate. 03:06 We can then see the length of the penis, which has the urethra now containing the sperm enclosed within that seminal fluid passing through the urethra of the penis. 03:19 Let's just remember that the testes didn't actually start off within the scrotal sac. 03:24 They migrated down from the posterior abdominal wall. 03:28 So here during embryological development, Notice we're now calling the dorsal abdominal wall, but they reside on that dorsal aspect of the abdominal wall. 03:36 And then they passed through the inguinal canal to end up within the scrotal sac. 03:42 That's why it's important to remember the structures of the inguinal canal, which we'll come to in the next slide. 03:48 So here we can see now the sagittal section through the scrotal sac. 03:53 So we've gone through just lateral aspects to the penis. 03:57 We've gone through the scrotal sac and looking at a testes within the scrotal sac, and we can see that it's connected via spermatic cord. 04:05 So what makes up the spermatic cord? Well, we need to remember that the testes started on the posterior or dorsal abdominal wall, and they migrated through the inguinal canal. 04:15 Now we know there's various muscular and fascia layers that form the anterior abdominal wall. 04:21 And as that testi passed through those layers, they took various coverings with them. 04:27 So here we can see the testi within the scrotal sac. 04:30 And here we can see the ductus deferens emerging from the epididymis. 04:35 That ductus deferens is associated with a number of layers, and those layers in combination form the spermatic cord. 04:43 Let's have a look at those spermatic cord structures in more detail. 04:47 So here we have the skin of the scrotal sac, and then we have the outermost layer of the spermatic cord, which has come from external oblique aponeurosis. 04:57 So remember, as the testi passed through the inguinal canal, it went through the superficial inguinal ring. 05:06 The superficial inguinal ring was that defect that aperture within the external oblique aponeurosis. 05:12 So the most external layer of the spermatic cord is that last wall that it penetrated. 05:18 The external oblique aponeurosis. 05:21 So as it passed through that layer, it took this outermost covering, and this around the testi becomes the external spermatic fascia. 05:31 The next muscular layer, it passed through as it went through the inguinal canal was the internal oblique muscle. 05:37 Now, as this passed through internal oblique muscle, it also took a covering, and that covering then remains forming spermatic cord, but this is known as the cremasteric fascia or the cremaster muscle. 05:50 This muscle is still functioning and when it's particularly cold in the external environment. 05:55 This muscle can contract and it helps to elevate the testis closer to the body cavity helping to maintain the temperature. 06:02 So it's a temperature regulation mechanism. 06:06 Muscle fibers of internal oblique muscle retained within the spermatic cord as the cremaster muscle. 06:12 This helps to allow mobility of the testes as they can be drawn up closer to the body cavity. 06:19 The final muscle layer that it passes through as it passes from the abdomen into the scrotal sac isn't actually a muscle, it's a fascia layer. 06:28 It's transversalis fascia. 06:31 Now, if you remember the formation of the inguinal canal, transverse abdominus muscle doesn't actually form part of the deep or the superficial inguinal ring. 06:41 So, therefore, as the testi passes through, it doesn't take that layer. 06:45 What it does do is it passes through the layer that's deep to transversus abdominus and that is transversalis fascia. 06:53 So here we have the innermost layer of the spermatic cord, which is the internal spermatic fascia and that is formed from transversalis fascia and we can see that here. 07:04 So, various layers formed the spermatic cord. 07:07 We have the outer layer, which is the skin. 07:10 We then have it passing through external oblique aponeurosis, external spermatic fascia. 07:17 We have it passing through internal oblique muscle, which becomes the cremasteric fascia, retaining some muscle fibers. 07:25 Finally, it passes through transversalis fascia, and this becomes the internal spermatic fascia, which we can see here. 07:33 So some important layers that form the spermatic cord. 07:38 What you can notice, however, is that there's two areas of purple coloring, above and below the circle indicating the spermatic cord. 07:45 And this is the parietal peritoneum. 07:48 We can see here that the final deepest layer so most posteriorly, within the anterior abdominal wall was the parietal peritoneum. 07:56 Remember external oblique, internal oblique, transverse abdominus, transversalis fascia, then the parietal peritoneum. 08:05 So this is the most posterior layer of the anterior abdominal wall. 08:10 Now, the testi passes through the parietal peritoneum, but it doesn't become continuous with it still, like the other aspects of the spermatic cord. It breaks off. 08:19 And this forms this peritoneal pouch within the testi surrounding the testi within the scrotal sac, and this is known as the tunica vaginalis. 08:31 So here we can see the tunica vaginalis, which retains layers that are synonymous with all of the peritoneal cavities within the body. 08:40 So it has a parietal layer that lines the cavity in which the testes retained. 08:45 So the scrotal sac and its various layers. 08:48 It also has a visceral layer that is tightly adhered to the testi. 08:53 So we can see the parietal and the visceral layers. 08:56 Remember, they are continuous, like all other layers of peritoneum. 09:01 Between those two layers, we have a peritoneal cavity so to speak. 09:06 This will retain a thin layer of fluid, which helps the testi to be mobile within the scrotal sac. 09:11 And allows it to become, like I say, quite mobile, it can move around, and it gives it some flexibility and some agility within that space. 09:20 This is known like I said, as the tunica vaginalis. 09:24 We also have a layer that surrounds the testes, and that's called the tunica albuginea. 09:29 And this is a tough fibrous capsular layer. 09:32 And what that does is that helps to structure a whole series of seminiferous tubules. 09:37 And these seminiferous tubules are where the spermatozoa are created. 09:42 All of the spermatozoa once created from the seminiferous tubules pass into a kind of network that gathers them all before passing them towards the epididymis via the efferent ductules, which we can see here. 09:56 The passing of this spermatozoa from the seminiferous tubules passes to what's known as the rete testis, and this is in an opening of the testi we can see there. 10:07 And that passes to the head of the epididymis. 10:10 via these efferent ductules. 10:12 Efferent because these spermatozoa are exiting the testes to go to the head, the body, the tail of the epididymis, which we can see there. 10:22 The tail of the epididymis is then continuous with the ductus deferens which we picked up. 10:28 So the testi and the production of sperm is quite complicated. 10:31 There's lots of structures here. 10:33 but essentially sperm are produced within the testi. 10:36 Once they've been produced, they pass via the seminiferous tubules into a network that filters and channels all of the sperm into the epididymis passing through the rete testi, the efferent ductules and then the head, body, and tail of the epididymis. 10:53 This is allowing that mass concentration of spermatozoa that have been produced that can then pass into the ductus deferens. 11:00 The ductus deferens then runs within the spermatic cord. 11:03 It passes from the spermatic cord into the superficial inguinal ring, inguinal canal, deep inguinal ring, and then passes in to the abdominal pelvic cavity.
About the Lecture
The lecture Anatomy of the Testes by James Pickering, PhD is from the course Anatomy of the Male Reproductive System.
Included Quiz Questions
The epididymis gives rise to which structure?
- Ductus deferens
- Urethra
- Ureter
- Seminal vesicle
- Penile bulb
What is the function of the seminal vesicle?
- Secrete part of the fluid in semen
- Carry semen from the testicle to the epididymis
- Carry semen from the epididymis to the prostate
- Supply blood to the prostate
- Recycle semen
What structure forms the pre-ejaculate?
- Bulbourethral gland
- Prostate
- Ejaculatory duct
- Seminal vesicle
- Epididymis
Which statement is correct about the testes?
- They descend through the inguinal canal during embryogenesis.
- They descend medial to the inguinal canal during embryogenesis.
- They descend from the renal pelvis during embryogenesis.
- They do not move during embryogenesis.
- They ascend through the obturator canal during embryogenesis.
What is the most external layer of the spermatic cord?
- External oblique aponeurosis
- Skin
- Internal oblique muscle
- Cremasteric fascia
- Cremasteric muscle
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |