Playlist
Show Playlist
Hide Playlist
Amyotrophic Lateral Sclerosis (ALS) and Other Motor Neuron Diseases
-
Slides Diseases of the Motor Neurons.pdf
-
Download Lecture Overview
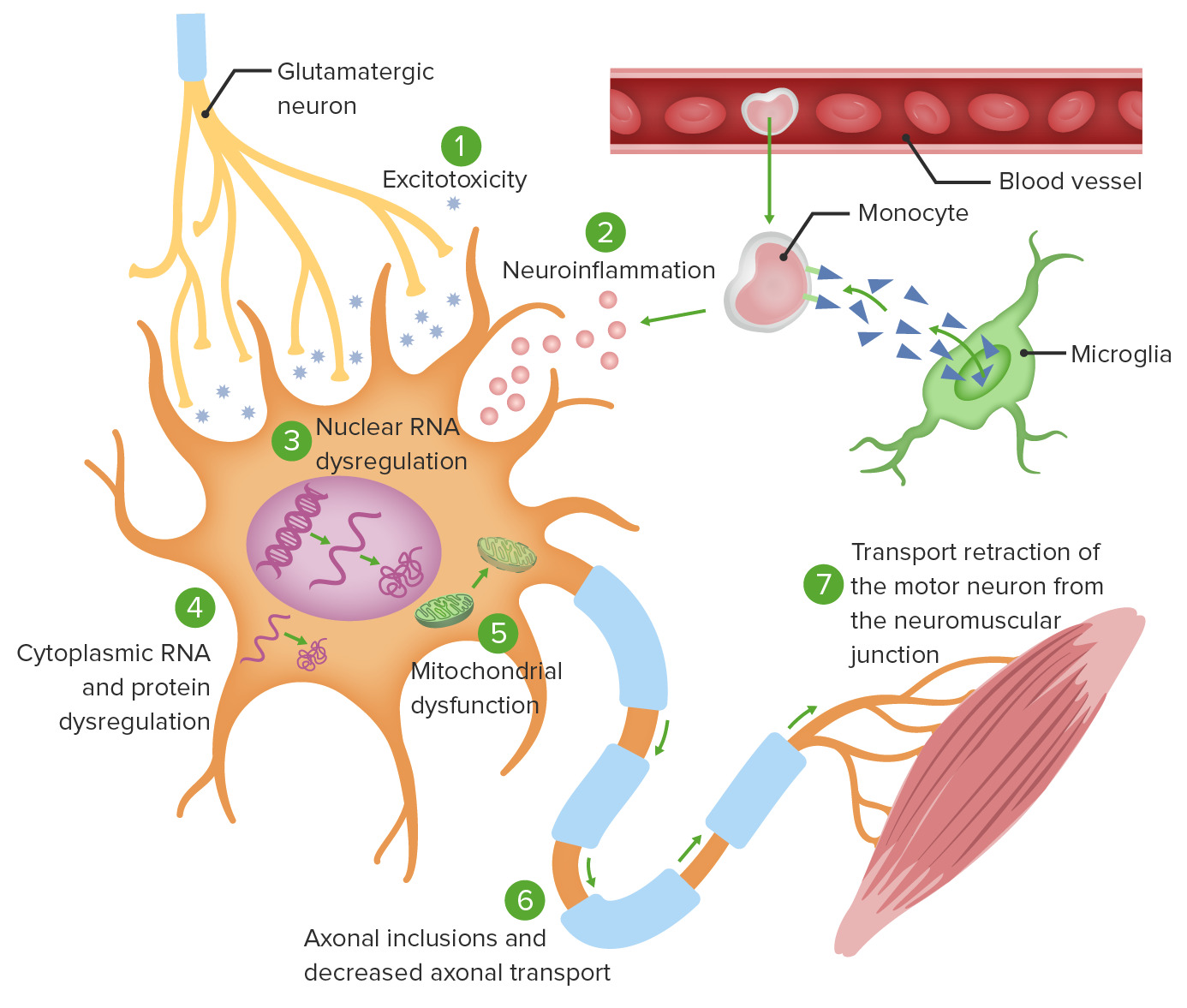
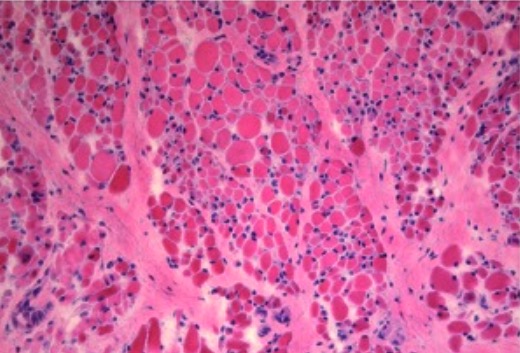
00:01 Now let's talk a little bit more about ALS, and the diagnosis of ALS will be by exclusion, excluding many of those other causes, but we can also be supported in the appropriate clinical setting. 00:14 First, let's start with a definition. 00:15 This is a neurodegenerative disease involving both upper and lower motor neurons. 00:19 There's degeneration of the primary and secondary motor neurons. 00:24 It's also known as Lou Gehrig's disease from a famous individual early in the description of this syndrome. 00:32 It is a progressive disease. 00:34 Patients begin with chronic onset of symptoms that is relentlessly progressive over time. 00:39 Patients become weaker and weaker as the condition progresses, eventually leading to paralysis and ultimately death, typically from dysphasia, or pulmonary dysfunction, weakness of respiratory muscles, and pneumonia. 00:52 And there is no cure for this condition. 00:56 How about the epidemiology? This is one of the most common progressive motor neuron diseases that we see, 90 to 95% of cases are sporadic. 01:05 There is this small group of cases that are inherited and a number of genes have been described, though the vast majority of patients do not have an underlying genetic, single genetic etiology. 01:17 And the case is sporadic in onset. 01:20 And the underlying etiology in those cases is unknown. 01:24 And here we're looking at a patient who has significant atrophy of multiple muscle groups throughout the upper and lower extremities and may have for fasciculations again supporting the lower motor neuron findings in this patient. 01:37 In terms of pathologies, one of the things that we see typically at autopsy, because biopsies aren't typical for this condition, are degenerative changes in the motor neurons in both the cortex and the anterior horn cells, the cell bodies of the primary and secondary motor neurons and we see these inclusions, these Bunina bodies, which are eosinophilic inclusions that are contained within the neurons and are pathognomonic for this condition. 02:03 Now let's talk a little bit about the clinical manifestations and the diagnostic investigation. 02:08 What do we look for on exam to support a diagnosis of ALS? Well, again, we're looking for upper and lower motor neuron findings and those upper motor neuron findings are spasticity slowed, rapid alternating movements from spasticity, a spastic gait, spontaneous clonus or hyperreflexia. 02:26 Those are suggestive of upper motor neuron pathology. 02:30 We can also look for lower motor neuron symptoms and signs and that includes prominent muscle atrophy, fasciculations which has very good specificity for lower motor neuron disorder. 02:41 Proximal arm and leg weakness, poor heel and toe walking from weakness of the proximal muscles of the legs. 02:48 Poor rise from a chair, also a proximal muscle weakness symptom, foot drop, waddling gait and hyperreflexia. 02:56 Asymmetrical weakness can be one of the earliest signs and is not uncommon in patients presenting with ALS. 03:05 Fasciculaitons is very important and I cannot underscore this enough. 03:08 You don't see it if you don't look and you have to look in this condition. 03:12 Fasciculations are visible, involuntary contractions of an entire motor unit, a motor nerve and all of the muscles that it innervates. 03:20 This occurs secondary to reinnervation of denervated fibers that spontaneously depolarize and we can see this anywhere in the body. 03:28 Some of the places we frequently look or the first dorsal interosseous muscle, the upper extremity muscles, lower extremity muscles and the tongue and the presence of tongue fasciculations should strongly suggest a consideration for a diagnosis of ALS. 03:46 Some of the other clinical manifestations, we can see limb weakness, cramping in the early morning, instability of gait, falling due to spasticity or weakness, fatigue when walking now that may suggest neuromuscular junction disease, but we can also see it with other causes of weakness. 04:01 Stiffness in the affected limbs, particularly stiffness in limbs that have significant atrophy is indicative of a combination of upper and lower motor neuron signs and in coordination of the affected limbs. 04:13 Pain is not common in this condition, and we really shouldn't see pain early in the disease. 04:18 Late in the disease, we can see pain, and that's commonly due to spasticity or decreased mobility and so the more spastic and less mobile that joint is, the more pain we can see in that condition and some of our treatments and management is to reduce pain in those patients. 04:29 and some of our treatments and management is to reduce pain in those patients. 04:33 Traumatic injury from falls is also not uncommon and can be a source of pain, but pain should not be present, typically is not present at the time of initial presentation. 04:44 ALS is one type of motor neuron disease. 04:47 It's the most common motor neuron disease but not the only one and there are a number of variants. 04:51 One is progressive muscle atrophy and this is a lower motor neuron variant. 04:55 This typically occurs sporadically in adults. 04:58 There are no known occurrences of the disease within family, and this has a lower motor neuron variant. 05:03 Spinal muscle atrophy is another lower motor neuron variant that is inherited. 05:08 So the sporadic form is progressive muscle atrophy and the inherited form is spinal muscle atrophy and this typically occurs in children, though there are a number of variants that can present early in life, early in childhood and then sometimes rarely in adolescence or rarely in adulthood. 05:24 Progressive bulbar palsy is bulbar face cranial bulbar predominant motor neuron disease and there are a couple of conditions to consider here. 05:33 One, Fazio-Londe Syndrome or spinal bulbar variant in children and then Kennedy's disease, spinal bulbar variant in adults. 05:42 This can also be associated with areflexia and gynecomastia, which we don't actually see in the clinic very often, but can be tested in various settings. 05:51 And then there are a number of other variants of motor neuron disease that we can see and need to consider, which are quite rare. 05:58 When I'm thinking about these ALS variants, I really like this graph, and the schematic for how to think through what's the type of motor neuron disease I need to be worried about. 06:07 ALS is the most common. 06:08 So if you see something that has combined upper and lower motor neuron pathology, throwing out ALS as the most common motor neuron disease is always the right answer. 06:17 But we can divide the other motor neuron diseases into those that are sporadic, or just acquired over the course of life, or inherited. 06:25 And we can look at those that are upper motor neuron predominant versus lower motor neuron predominant. 06:31 So let's start with the sporadically occurring motor neuron diseases. 06:34 The upper motor neuron variant is primary lateral sclerosis, and the lower motor neuron variant has progressive muscle atrophy with ALS right in the middle presenting with a combination of upper and lower motor neuron findings. 06:47 There's also a bulbar variant and we talked about two of those, Fazio-Londe in kids and Kennedy's disease in adults and those present with prominent bulbar findings initially. 06:58 There are also some inherited conditions that can masquerade as ALS. 07:02 The upper motor neuron variant is hereditary spastic. 07:05 Paraplegia, common in adults and spinal muscle atrophy is the lower motor neuron variant, more common in very young children. 07:14 Now let's talk about the treatment and prognosis for patients with ALS. 07:19 First of all, in terms of treatment, there is no cure for this condition. 07:22 We're looking for supportive care and disease modifying therapies that prolong life but nothing cures this disease. 07:29 Rilutek or Riluzole increases life expectancy in the order of several months and there continued to be studies and ongoing developments in the management and treatment of ALS. 07:38 So it's then in the future, hopefully, we have more treatments for this condition. 07:42 Additional disease-modifying treatments for ALS include edaravone and sodium phenylbutyrate-taurursodiol. 07:51 Edaravone is a free radical scavenger which reduces oxidative stress and may slow functional decline. 07:57 Sodium phenylbutyrate-taurursodiol is a histone deacetylase inhibitor which can reduce neuronal cell death and slow the rate of functional deterioration. In terms of prognosis, the life expectancy ranges from 3 to 5 years, but this is highly variable. 08:15 Some patients have a more rapidly progressive course, when there's significant dysphasia or respiratory weakness, patients have typically a more rapid course, and others have a more protracted or prolonged course. 08:26 It's important that we evaluate pulmonary function and swallowing and we do that by looking at pulmonary function. 08:33 And we see this drops to a concerning level. 08:36 Patients may be considered for non-invasive positive pressure ventilation, and for patients with significant dysphasia, weight loss or nutritional concerns. 08:45 A percutaneous endoscopic gastrostomy tube or PEG tube can be placed for alternative means of nutrition and they may impact both the morbidity, quality of life and mortality, the length of life in patients. 09:01 ALS is associated with a number of complications that also need to be considered and managed. 09:05 We can see laryngospasm, which can result from fasciculations of the laryngeal muscles Siallorhea from oropharyngeal weakness, pseudobulbar affect from damage of the brain and we can see this commonly in patients with certain variants of ALS. 09:20 Tongue weakness, offen with fasiculations, respiratory muscle weakness, and cognitive impairment is present in somewhere between 20 to 30 or 40% of patients. 09:30 Importantly, I want to mention this association between ALS and FTD, Frontotemporal dementia. 09:35 Increasingly, there has been recognition of an association between ALS, motor neuron disease and frontotemporal dementia. 09:42 We see a number of patients who have significant cognitive dysfunction as a result of this link. 09:47 These two conditions have been linked in FTD, specifically linked to ALS variants, particularly the bulbar predominant ALS in which patients often develop pseudobulbar affect that emotional lability, as well as dementing conditions. 10:00 There's some evidence from FTD genetic abnormalities and genetic studies that suggest that the spectrum of ALS and FTD is related to an underlying genetic link. 10:14 Lastly, I want to review some of the ALS variants. 10:17 Things that are on the differential diagnosis and we'll go through these quickly. 10:20 You need to know the names of these conditions and some of the key features but not all the details. 10:27 First, let's start with Stiff Person syndrome. 10:30 Stiff person syndrome is an autoimmune condition that typically is a result of antibody production against glutamic acid decarboxylase or GAD. 10:41 We see increased GAD levels in these patients who become very stiff and muscle groups throughout the arms and legs. 10:47 When we think about clinical manifestations of stiff person syndrome, there's waxing and waning stiffness with spasms that can be quite debilitating and painful. 10:55 This begins in the axial muscles of the trunk and then can spread to the proximal lower extremities. 11:01 Initial complaints include back pain, upright posture, worse with tension and stress. 11:05 Patients are very stiff, but it can fluctuate, which is different from typical motor neuron disease. 11:10 Later in the disease, their patients can develop stimulus-induced spasms and stiffness at the proximal upper and lower extremities. 11:16 This is an inflammatory immune mediated disorder that we treat with immunomodulating therapy. 11:23 Long term complications include bony abnormalities, joint deformities, and we can see an association with diabetes, seizures, thyroiditis, and breast cancer. 11:34 Next, let's talk about tropical spastic paraparesis. 11:37 This is another important differential diagnosis of ALS. 11:41 Tropical spastic paraparesis is also known as HTLV-associated myelopathy because it's a myelopathy, a spinal cord disorder associated with HTLV infection, and that's what you're looking at here in this pathology slide. 11:54 This is a slowly progressive condition that presents as a myelopathy. 11:57 So paraperesis, stiffness in the legs hyperreflexia and the etiology is this association with human T-lymphotropic virus, or HTLV-1 which is primarily transmitted through sexual or intimate contact. 12:12 This is an important consideration in patients presenting with an upper motor neuron-predominant syndrome The next condition that presents on the differential diagnosis with motor neuron disease is Tropical Ataxic Neuropathy or TAN. 12:27 The next condition I want to talk about is Tropical Ataxic Neuropathy. 12:30 This is an ataxic neuropathy, lower motor neuron predominant presentation, we see sensory neuropathy common in malnourished patients thought to be related to cyanide toxicity from cassava intake. 12:42 patients present with subacute to chronic burning pain in the hands and feet and difficulty walking and can have a range of neuropathy, ataxia, hyperreflexia as well as sensory neural hearing loss and the key feature here is there is prominent sensory findings in these patients which is really different from our typical motor neuron disease. 13:01 Primary Lateral Sclerosis is that sporadic upper motor neuron form of motor neuron disease. 13:08 These patients typically present with leg weakness with spasticity. 13:12 There can be spastic bulbar dysfunction as well. 13:14 But the key is there's upper motor neuron pathology with cortical bulbar and corticospinal tracts. 13:20 It's often asymmetric. 13:22 This often begins with spasticity followed by weakness, whereas with ALS, you often see weakness followed by spasticity. 13:28 And some associated features include abnormalities with eye movements, saccades caused by a volunteer goal directed eye movements, urinary dysfunction and cognitive dysfunction. 13:39 Then there's also primary muscle atrophy. 13:41 This is the lower motor neuron variant, it's a sporadically acquired condition and accounts for 10% of motor neuron diseases. 13:49 It's more common in men, presents with progressive weakness with no other known etiology. 13:54 So you need to rule out other neuromuscular junction and myopathies and peripheral nervous system disorders. 14:01 And the prognosis is better than ALS, it's more slowly progressive than the typical ALS
About the Lecture
The lecture Amyotrophic Lateral Sclerosis (ALS) and Other Motor Neuron Diseases by Roy Strowd, MD is from the course Diseases of the Motor Neurons.
Included Quiz Questions
What percentage of ALS cases are inherited?
- 10%
- 80%
- 50%
- 25%
- 1%
Which of the following is a common finding early in the disease course of ALS?
- Asymmetric weakness
- Neuropathic pain in the feet
- Bilateral lower extremity sensory loss
- Dysphagia
- Respiratory muscle weakness
Which ALS variant affects adults and has a predominance of spinobulbar symptoms?
- Kennedy syndrome
- Fazio-Londe syndrome
- Brachial amyotrophic diplegia
- Spinal muscle atrophy
- Progressive muscle atrophy
Which of the following ALS variants is inherited and mostly affects children?
- Spinal muscular atrophy
- Hereditary spastic paraplegia
- Progressive muscular atrophy
- Primary lateral sclerosis
Which is TRUE of stiff-person syndrome?
- Patients commonly present with back pain and worsening posture with stress.
- It is an ALS variant of infectious etiology.
- It is caused by autoantibodies to acetylcholinesterase.
- It initially affects the extremities before moving on to axial muscles.
What virus is associated with tropical spastic paraparesis?
- HTLV-1
- HIV
- HSV
- EBV
- CMV
What clinical manifestation would lead one to favor the diagnosis of primary lateral sclerosis versus amyotrophic lateral sclerosis?
- Muscle spasticity followed by weakness
- Bulbar involvement
- Asymmetric presentation
- Sensory involvement
- Cognitive dysfunction
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |