Playlist
Show Playlist
Hide Playlist
Acute Tubular Necrosis: Diagnosis and Treatment – AKI
-
Slides Nephrology Acute Kidney Injury.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
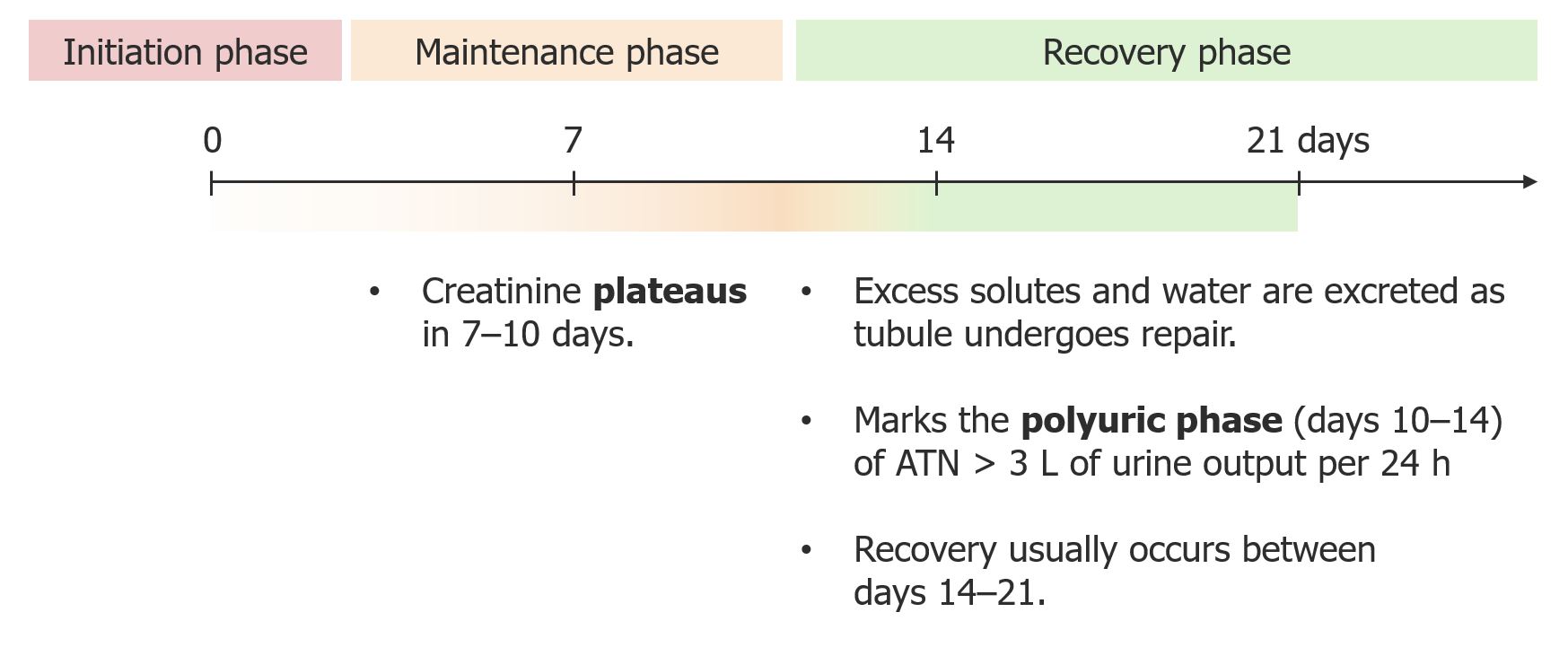
00:01 So, once our patient has ATN, what is our diagnostic workup and how can we actually come to that conclusion? Just as we have in every other portion, we're gonna be a good detective. 00:13 We're gonna look at that history and do a very thorough chart review. 00:15 So we wanna see, has our patient had any period of time where they've had prolonged hypotension in the ICU or in any other circumstance? Did they have any evidence of ischemic hits to the kidney or low blood pressures? Have they been exposed to radiocontrast? Now with the advent of electronic medical record, that's very easy to see. 00:35 We can just look under our diagnostic imaging, under our cardiac cast and see if those patients were actually administered iodinated contrast from either an angiogram or CT scan. 00:45 And then , we also want to see if our patient had a period of sepsis. 00:48 Did they have septic physiology? Were they in the ICU for a period of time? These are all things that can lead us to the right direction of more risk factors that can be involved in acute tubular necrosis. 01:00 We're also looking for drugs so looking under medication administration record in our AMR, we're able to see was that patient actually administered aminoglycosides for a bacterial infection? Amphotericin B for a fungal infection? or did they have a crush injury or were they found down for a prolonged period of time. 01:16 It's not uncommon for us to see at our hospital patients that are brought in because of the fact that they've been found down either from a drug overdose or another phenomena where they're down for a long period of time and they end up with a crush injury to muscle. 01:30 And that would be rhabdomyolysis. 01:34 So, there's some laboratory evaluations that make it very helpful to see what's going on. 01:38 So when we look at our serologies, we're looking at BUN and creatinin. 01:42 And specifically oftentimes with pure ATN, you could really see that BUN to creatinine ratio being less than 10-15:1 This is as opposed to pre-renal, remember we talked about that being greater from 20:1. 01:54 This is about 10-15:1. 01:56 And if you think about why that's happening, remember what we said pathophysiologically what's happening. 02:01 We have that patch necrosis in the S3 segment and the thick ascending limb in the loop of Henle. 02:05 This is also areas where we're going be reabsorbing urea, so if we don't have that because these tubules are damaged, then we see less urea nitrogen in our blood. 02:15 So that's why the BUN to creatinine ratio is a little bit less. 02:18 Our urine sodium and chloride are going to be high, typically greater than 20 mEq/L again because we are spilling sodium into our urine because we are not absorbing that at that proximal tubule and the thick ascending limb of the loop of Henle. 02:32 When we calculate our FENa which we learned about in our pre-renal section, it's going to be greater than 2% and that's important because that tells us that that patient most likely is not going to be responsive to volume resuscitation. 02:45 Then of course, we want to look at the urine. 02:47 And the urine always tells a lot so typically these patients are isosthenuric, They have a specific gravity that's relatively normal. 02:54 They can't really concentrate because they've lost that ability. 02:57 Why? because the medullary gradient is really washed out and not maintained because again if you think about where the injury is, it's at that thick ascending limb of the loop of Henle and that's critical in order to maintain your medullary gradient. 03:10 And the urine osmolality in our patients because of this is typically less than 450 mOsm/kg oftentimes it's isoosmolar to the serum osmolarity. 03:22 Our patients may also have low-grade proteinuria, typically it's between 500 (mg) to 1 gram within a 24-hour period of time. 03:31 And that's oftentimes because of impaired reabsorption of protein at thst proximal tubule. 03:36 So it's not necessarily glomerular damage but we do absorb proteins other than albumin at that proximal tubules so again if proximal tubule is damaged, we're gonna see some proteinuria. 03:46 And then my favorite part being a nephrologist which I talked about before is I get to look at the urine underneath a microscope and that's exciting because there are clues there for me that tell me and that can tell you whether or not your patient has ATN. 03:59 In this situation, we get to see these really wonderful cellular cast called pigmented granular cast. 04:06 And they look just like this, this is from one of our patients who had ATN and you can see you have these kind of beautiful brown cylindrical cast that are granular in quality and they populate the entire field, this is looking at the 10x view. 04:19 And that's great because the specificity is high and it tells us that that patient does have a tubular injury Sometimes if you're lucky enough, you can actually see a tubular epithelial cell free-floating in the urine as well. 04:32 And these are all things that ar e gonna tell you that this patient likely has acute tubular necrosis. 04:38 So in terms of the the clinical course and how people do with ATN, they oftentimes go through kind of a 3-phase approach. 04:47 So they have the initiation phase where injury occurs and sometimes gets augmented, And then the maintenance phase, this is where the creatinine plateaus. 04:57 Typically, it occurs anywhere from 7-10 days after the injury And then the recovery phase, where the excess solutes and water tend to be excreted as the tubule undergoes repair. 05:08 And that oftentimes will mark the polyuric phase, anywhere from days 10-14 of ATN And this important because our patient's actually changed in their clinical appearance . 05:17 Instead of being oliguric, they are now polyuric - they're making lots of urine. 05:22 3 liters or more of urine. 05:23 And again, part of this is because they're just removing these extra solutes that they built up when when they have renal failure. 05:29 But part of this too is that they've lost that concentration gradient in their medullary interstitium and so because of that again, they are quite polyuric and they're unable to concentrate their urine. 05:41 Recovery in the typical phase will usually occur somewhere between 14-21 days. 05:46 I do want to say that this is textbook approach and it would be wonderful if our patients always behave this way, but oftentimes, ATN can either be shortened or it could be much longer. 05:56 And sometimes it takes up to 3 months for our patients to recover from their tubular injury. 06:04 Okay, so what do we do once our patient is diagnosed with ATN, How can we treat them or what can we do to prevent that from happening? We just said that this is one of the most serious types of AKI because of the mortality association with it. 06:17 So it's important to really identify people who are at risk, so people who are undergoing major surgery, why? Because there's a real chance for a drop in mean arterial pressure during surgical cases. 06:29 People who are in shock, right? They might have these dilatory shock, cardiogenic shock, our patients who have comorbid conditions that would put them at risk. 06:38 That would be patients with chronic kidney disease, we already talked about how they're really vulnerable to having an acute tubular injury. 06:46 People who have peripheral vascular disease, diabetes is coming up once again, people with malignancies, heart failure and malnourished patients. 06:54 So people who have these comorbid conditions really are at an increased risk when they're coming into the hospital to develop acute tubular injury. 07:03 So things that we can do to decrease that risk in addition to identifying those people who are at risk is we want to really optimize volume status and maintain hemodynamic stability. 07:12 That's really critical, we want to avoid any points of ischemia. 07:17 We want to avoid nephrotoxic exposures. 07:20 I definitely do not want to be giving my patients NSAIDs during their stay if I feel that they are a population who are at risk of developing a tubular injury. 07:28 Similarly, I don't want to give them nephrotoxic medications like Amphotericin or aminoglycosides, and then contrast-induced nephrotoxicity. 07:37 There's a couple of things that we can do to mitigate that injury. 07:40 So I know that my patient has to have contrast because the CT scan is critical and being able to diagnose what's happening with them or they need an angiogram because they're coming in with acute coronary syndrome and they have to have dye in order to place a stent or diagnostically see what's going on with them And then I'm gonna do a couple of things. 07:59 I want to make sure that their volume status is really optimized. 08:03 They can't go into that procedure hypovolemic. 08:05 So I'm gonna volume expand them with crystalloids, something like normal saline pre and post contrast in order to maintain the hemodynamics and dilute that contrast and try to wash that away as soon as possible. 08:18 I also am going to be talking to my radiology colleagues as well as my cardiology colleagues and I'm gonna ask them to minimize the amount of contrast that they're using for my patient. 08:26 Sometimes, we can get away with using much less or we could even use an alternative contrast agent like CO2 in order to light up our vessels, and that could really help us. 08:35 I do just want to make one comment because there's been some thought processes in the past that perhaps if we gave diuretics at the same time when our patients were getting these contrast that they would do better, We know that definitively evidence has shown that diuretics are not helpful in the course of ATN. 08:52 We do use them if our patient is volume overloaded and we have to mobilize volume. 08:57 But we're not using them in order to essentially convert their renal failure to a non-oliguric state or essentially see urine output, so do keep that in mind. 09:08 Okay so that's ATN. 09:10 And again the big things that I really want to stress is that this is such a serious injury because of its association with mortality. 09:17 And there's a lot of things that we can do in terms of identifying populations at risk and then being able to mitigate or prevent some of the things from happening.
About the Lecture
The lecture Acute Tubular Necrosis: Diagnosis and Treatment – AKI by Amy Sussman, MD is from the course Acute Kidney Injury (AKI).
Included Quiz Questions
Which of the following would you expect to see on urine microscopy in a patient with acute tubular necrosis?
- Pigmented granular casts
- Rouleaux red blood cells
- White blood cell casts
- No cells or debris
A man fell and broke his hip during the night and was not able to access his phone to call for help until the morning. He was noted to have dark urine with a FeNa concentration of >2% on admission, and he reported generalized pain in the hip region. Which of the following is most likely present?
- Intrinsic renal disease
- Prerenal disease
- Postrenal obstruction
- Normal kidney function
A woman is admitted for sepsis, related to a urinary tract infection, and is found to have acute tubular necrosis. Fourteen days after discharge, she is complaining of significant urine output of more than 3 L a day. What is the most likely cause of this polyuria?
- Recovery of kidney function after the accumulation of solutes during intrinsic kidney disease
- The urinary tract infection resolving
- Serum creatinine levels stabilizing
- Protein in the proximal tubule that is reabsorbed after recovery
Which of the following patients is most at risk for acute tubular necrosis?
- A patient with spleen laceration requiring 4 units of packed red blood cells
- A patient with type 2 diabetes taking acetaminophen 500 mg for occasional headaches
- A patient with mild to moderate dehydration after running 5 km on a 32°C (90°F) day
- A patient with benign prostatic hyperplasia causing urinary retention
Which of the following can minimize the risk of acute tubular necrosis?
- Volume expansion before and after radiocontrast for computed tomography
- Giving packed red blood cells for fluid replacement in trauma
- Treatment of a bacterial infection with an aminoglycoside
- Treating chronic heart failure with diuretics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |