Playlist
Show Playlist
Hide Playlist
Acute Blood Loss
-
Slides Normocytic Non-Hemolytic Anemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
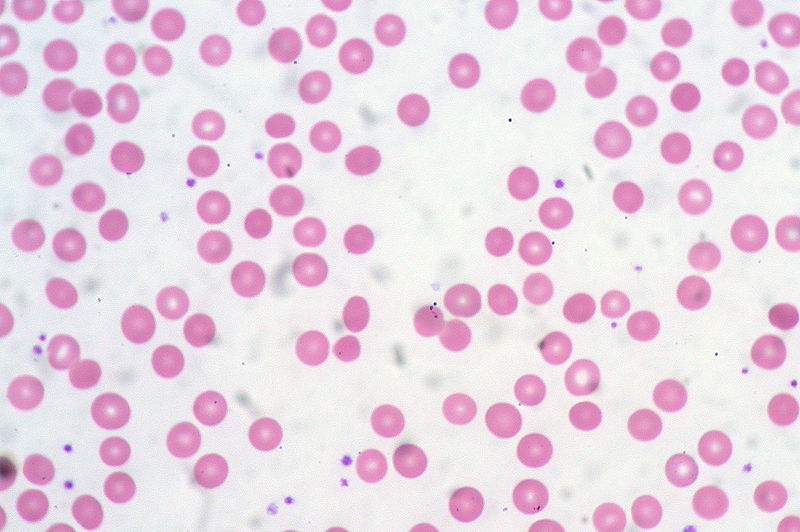
00:00 At this point, we're looking at the largest category of anemias and this would be normocytic. We'll begin our discussion by looking at non-hemolytic anemias with an MCV between 80-100. Of all of the non-hemolytic anemias, the ones the students tend to be a little confused with would be acute blood loss. Another reason for that is because the students feel as though that while the RBCs are being destroyed because you're losing it and then obviously externally they get destroyed but understand when you're actually losing it they're not being destroyed on the way out. So therefore, you still must consider this to be a non-hemolytic and then the reason that you call this normocytic or refer to it as being normocytic is because you're losing equal quantity of RBCs and then plasma. So this is whole blood that you're actually losing and so therefore when you actually conduct a measurement, you end up finding an MCV between 80-100. So that would be the trickiest but ones you understand the definition, then we can move forward and also think as to what you want to do with this patient. Oftentimes they would be a patient that is feeling hypotensive and so therefore IV fluid is something that you want to give and with that meaning to say that IV fluids do not contain RBCs. That is not packed RBCs. Is it? Major cause is trauma obviously if there is enough blood loss and this discussion with also being your best interest to bring some of those concepts that we looked at earlier in nephrology and as to what actually controls volume and also controls your osmolarity and when there is enough blood loss and volume loss, then the priority of the body is to then address the volume sometimes at the expense of your osmolarity and that discussion we have had prior. Now with anemia, what else might then cause acute blood loss? Well, GI bleeding. If there is a bleeding ulcer severe enough or secondary to poor hypertension, if there is esophageal varices that at some point extremely dangerous because you're worried about rupture and bleeding and diverticuli and by that at some point, remember one of the common causes of painless rectal bleeding is diverticulosis. And if there is enough blood loss, then your patient is going to be in a state of normocytic, non-hemolytic anemia because the blood is being evacuated from the body. Now, there are 2 ways that we can do this. We can leave it for physiology naturally for the plasma to then be replenished or more likely the scenario is going to be with this type of acute blood loss especially secondary to trauma the patient is now given saline and so therefore this replaces the plasma compartment only. Correct? So if it's only compartment that you're replacing is the plasma fluid, then obviously here you're going to then reveal the anemia because you're diluting the RBCs. So at first, the whole blood has been loss but then once you replenish the plasma, then it's the RBCs that are not there. "Oh, look at these." The anemia has now been unveiled." I hope that makes sense. Then as far as the bone marrow is concerned, it takes about well approximately a week, keep it simple, for it to then respond with reticulocytosis. What does that mean to you? It means that now the body recognizes "Oh my goodness." The RBCs are not present and so therefore the bone marrow has to now churn out more RBCs and as it does so well reticulocytosis. What's reticulocyte? It's an immature RBC by 24 hours. Okay. Completely different from a previous version where the progenitor is known as your erythroblast, your normoblast.
About the Lecture
The lecture Acute Blood Loss by Carlo Raj, MD is from the course Normocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
In acute blood loss, which organ is responsible for replacement of plasma?
- Kidney
- Pancreas
- Thymus
- Spleen
- Bone marrow
What is the amount of time that bone marrow takes to respond with reticulocytosis after blood loss?
- 1 week
- None of these
- 1 year
- 6 months
- 4 weeks
Why is anemia NOT seen initially in acute blood loss?
- RBCs are lost with plasma.
- Only plasma is lost.
- More RBCs are lost than plasma.
- More plasma is lost than RBCs.
- Only RBCs are lost.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |