Playlist
Show Playlist
Hide Playlist
Vitamin B12 Deficiency Myelopathy
-
Slides Diseases of the Spinal Cord.pdf
-
Download Lecture Overview
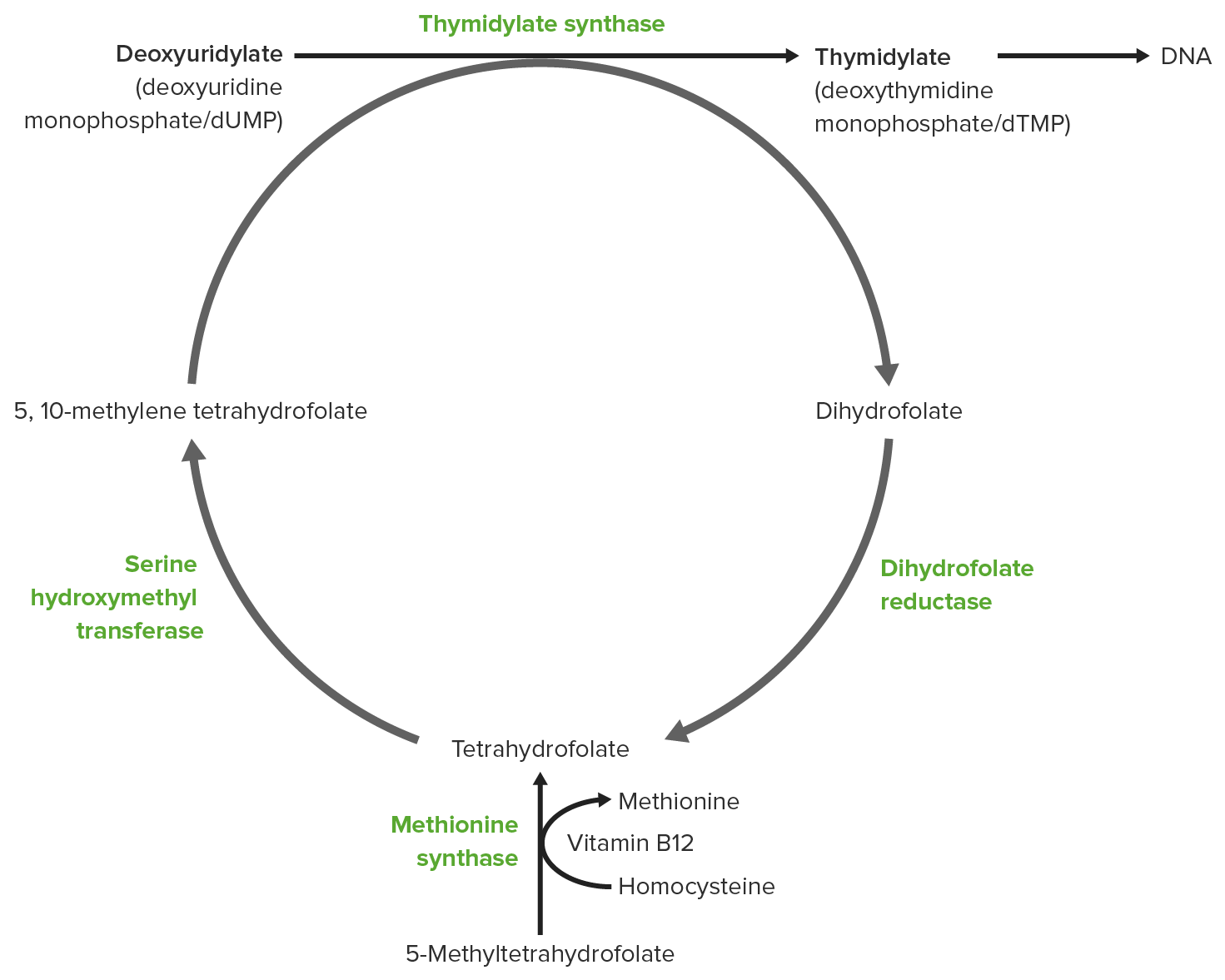
00:00 So let's talk a little bit more specifically about the B12-deficient myelopathy. This is common and the disorder that I would like for you to know and think about when you're considering a toxic metabolic myelopathy. Let's start with a definition. This disorder is characterized by subacute combined degeneration of the spinal cord and it's a neurologic complication of B12 deficiency. The subacute combined degeneration is helpful in understanding how these patients present. It's a subacute onset condition often presenting over the course of several weeks with weakness, upper motor neuron signs, and potentially some degree of dementia or cognitive dysfunction. And there is combined degeneration of the lateral corticospinal tracts and the dorsal column. 00:45 And so patients present with upper motor neuron signs owing from the corticospinal tract involvement and problems with vibrationand proprioception. Those sensory modalities are affected owing to disorders and dysfunction of the dorsal columns. 01:00 This may occur from nutritional deficiency, reduced absorption of B12, or due to intake of certain drugs and subacute combined degeneration is characterized by this combinatorial degeneration, which is very important in its pathophysiology and presentation. When we think about B12 deficiency, there are a number of different types of presentations. We can see dorsal column involvement, the lateral corticospinal tract involvement, and then also spinocerebellar tract degeneration. And we look for each of those findings in patients as we're evaluating their presentation. 01:37 Some of the symptoms we can see include sensory deficits, again involvement with vibration and proprioception, paresthesias, weakness or paraparesis is not uncommon, ataxia can be seen along with gait disturbances, and in severe untreated cases we can see spasticity and paraplegia when the condition is particularly fulminant. What about causes? What are some of the causes of reduced B12 in the body? Well, nutritional deficiency is one. We can also see this disorder in patients with gastric abnormalities, gastric surgery, gastritis, autoimmune gastritis where there is autoimmune damage to the distal small bowel, distal ileum resulting in pernicious anemia, small bowel disease, pancreatic disease, as well as several drugs including nitrous oxide and genetic abnormalities. In terms of work-up, we think about 4 steps in the work-up of vitamin B12 deficiency. First, we look for associated signs that may point us towards this disorder and that includes hematologic abnormalities that suggest a cobalamin or vitamin B12 deficiency. Second, we want to confirm that vitamin B12 is indeed deficient. 02:47 Three, we want to look for the cause of the vitamin B12 deficiency. And four is we look for any demyelinating lesions or findings on imaging that would be supportive of this diagnosis. So let's walk through each of those. Step 1 involves a complete blood count and potentially a blood smear, which helps to identify hematologic abnormalities that we can see in vitamin B12 deficiency. This includes a macrocytosis and anemia, so a macrocytic anemia, as well as hypersegmentation of neutrophils. And these findings support the diagnosis of B12, but may also be seen in folate deficiency in other conditions. Our second step involves confirmation that B12 is indeed low and we can do this in one of 2 ways. The first is to measure serum vitamin B12 levels and we suspect to see this as low although early in the condition we may still have a borderline or a borderline low B12 and in those cases methylmalonic acid and homocysteine can be helpful. These are intermediates in both B12 metabolism and they're elevation is used to confirm a B12 deficiency. And lastly, it's always important to consider ordering folate levels and those where we're considering B12 deficiency given the commonality of these in terms of their presentation, signs, and symptoms and we wouldn't want to miss a diagnosis of folate deficiency that can mimic B12-deficient myelopathy. 04:14 Our 3rd step is to evaluate the cause of vitamin B12 deficiency and there are a number of things that we may want to consider. We may test for autoantibodies to detect pernicious anemia and that includes anti-intrinsic factor antibodies. 04:28 Antiparietal antibodies may also be present and sometimes we consider serum gastrin levels and that may be indicated when there is high suspicion for pernicious anemia and an otherwise unremarkable work-up. Historically, the showing test was used to evaluate these patients but really is not used clinically these days. 04:46 And then our last step may be to look for and evaluate other confirmatory or suggestive signs of this condition. MRI may be normal in evaluating these patients who present with a myelopathy, but we can see characteristic changes in the spinal cord that support this diagnosis. And there is some difference in terms of whether the patient is evaluated early or late in the disease course. Early in the disease course, it's not uncommon to see hyperintensity in the dorsal columns of the cervical and upper thoracic spinal cord giving that characteristic inverted V sign. There is a predilection for the dorsal column so we see that signal abnormality confine to the dorsal columns and sparing other areas of the spinal cord. We don't see spinal cord edema or swelling, which would point us towards a neoplastic or inflammatory etiology. 05:35 And importantly, these findings may be present in patients with fulminant disease course or rapid progression of symptoms but the MRI may also be normal in cases of B12 deficiency. And so a normal MRI does not rule out this diagnosis. Later in the course, we may see T2 hyperintensity that have also appeared in the lateral corticospinal tract owing to the subacute and combined degeneration of those 2 white matter tracts. Now let's talk about management. In patients who are B12 deficient, the goal is to replete serum and circulating B12. Typically, we think about treatment with vitamin B12 at a dose of 1000 mcg orally once daily though patients with significant malabsorption may require higher oral doses and in those patients who present with neurologic dysfunction or significant manifestations of vitamin B12 deficiency, intravenous or subcutaneous injection and supplementation is often used. 06:33 So there, we administer 1000 mcg intramuscularly once a week for 1 month followed by once a month for about 6 months, and then transition to oral replacement.
About the Lecture
The lecture Vitamin B12 Deficiency Myelopathy by Roy Strowd, MD is from the course Diseases of the Spinal Cord.
Included Quiz Questions
Which drug(s) can cause vitamin B12 deficiency?
- Metformin
- Sulfonylureas
- Iodine
- Muscarinic agonsits
- Ibuprofen
What is the next step in the workup after identifying and confirming a vitamin B12 deficiency?
- Determining the cause of cobalamin deficiency
- Administering intramuscular vitamin B12
- Ordering an MRI to identify demyelinating lesions
- Ordering a methylmalonic acid (MMA) level
- Administering oral vitamin B12
What lab test may be ELEVATED in patients with borderline levels of vitamin B12 suspicious for deficiency?
- Methylmalonic acid (MMA)
- Folate
- Copper
- Zinc
- Serum gastrin levels
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |