Playlist
Show Playlist
Hide Playlist
Upper and Lower Motor Neuron Diseases: Diagnosis and Management
-
Slides Diseases of the Motor Neurons.pdf
-
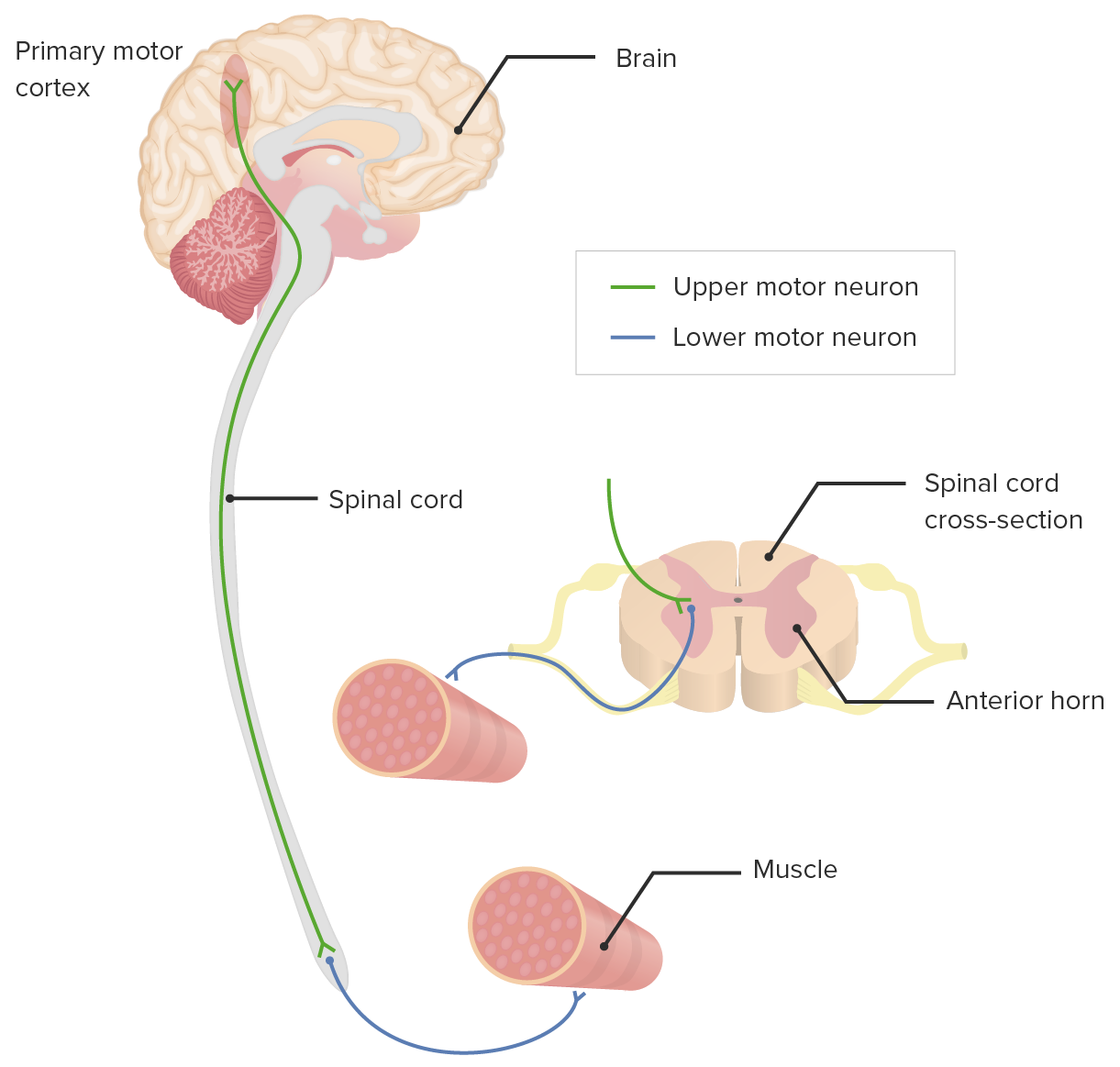
Download Lecture Overview
00:02 Now let's talk about the diagnosis. 00:03 How do we diagnose motor neuron diseases? Well, first we start with our history. 00:09 And this is really important. 00:10 There is no diagnostic test that says that this patient has a motor neuron disease, we're putting together the symptoms from the history and the signs from physical exam, as well as some of our diagnostic testing to exclude alternative conditions. 00:23 First, we want to define the symptoms and we've talked about some of the symptoms that are suggestive of upper and lower motor neuron conditions. 00:31 The onset of the disease is often insidious. 00:34 There's not a day when the patient develop weakness, but this slowly develops over the course of months. 00:38 It's a chronic onset condition that develops over time. 00:44 We see that typically, motor neuron diseases progress and they begin chronically and then progress consistently, relentlessly steadily over time. 00:53 This typically is not rapid though there are some variants of motor neuron disease that can progress more rapidly. 00:58 But it's typically gradual in its progression and evolution over time. 01:03 We don't see exacerbations on remissions. 01:05 In the presence of an exacerbation and remission such just some alternative etiology, an autoimmune condition or a paraneoplastic process or perhaps an infection or occupational exposure. 01:16 And this should send us down an alternative diagnostic workup. 01:20 And then there are a host of symptoms that can affect the patient's life. 01:22 And so we want to hear about those symptoms that would evaluate and establish the diagnosis as well as to support the patient regardless of what the diagnosis ends up being. 01:34 And then how about on examination, we're looking at the motor and muscle examination and patients presenting with weakness from motor neuron disease, we're looking at muscle bulk inspecting for atrophy, which we can see with lower motor neuron lesions, muscle tone, which we're inspecting for spasticity or a rigidity that we could see from an extrapyramidal syndrome. 01:53 But spasticity or that clasp knife rigidity is seen ith upper motor neuron lesions. 01:58 We're looking forfasciculations which is very important in these patients who present with weakness and muscle atrophy, to look for fasciculations, which would be indicative of a lower motor neuron disease. 02:09 And then we're looking at the weakness, patients typically present with a chief complaint of weakness and we want to interrogate what is the distribution. 02:15 When we see lower motor neuron symptoms in the same spinal segment as upper motor neuron symptoms, that pattern of weakness and findings is highly suggestive of a motor neuron disease. 02:26 And we want to test for proximal weakness and also look at distal weakness and typically, motor neuron disorders do not cause a typical proximal or distal distribution, but both can be involved. 02:39 When we're doing the diagnostic exam, complete neurologic exam is important, looking at cranial nerves for bulbar involvement, including tongue atrophy and fasciculations, looking at the motor and the sensory exam to exclude sensory findings and then also reflexes looking for the presence of upper and/or lower motor neuron findings on reflex exam EMG is often performed in these patients. 03:02 There's not an EMG signature that establishes the diagnosis of motor neuron disease, but we can see findings that are supportive of this diagnosis and exclude alternative etiologies. 03:12 With EMG nerve conduction, we typically see abnormal electrical signals in the muscles that are affected by the motor neuron disease and this typically is in the form of reduced amplitude. 03:22 There are less motor nerves. 03:24 Those motor nerves carry signal and because there's less of them, we see reduced amplitude, reduced size of the signal traveling through that motor nerve. 03:34 We can detect spontaneous depolarization of denervated muscle fibers as there are loss of nerves innervating the muscle. 03:41 The muscles do what they want, and they fire automatically and that spontaneous depolarization is something we can see on our EMG needle exam and is suggestive of a denervation process. 03:52 Importantly, the nerve conduction study is critical and we're looking at both involvement of motor nerves and sparing of sensory nerves which is helping to establish that motor neuronopathy that motor nerves are the primary nerves that are involved. 04:07 And then lumbar puncture is often performed not to establish the diagnosis of motor neuron disease, in which case usually the lumbar puncture is normal, but to look for alternative etiologies - infections, inflammatory disorders or neoplasms that could masquerade as a motor neuron disease. 04:25 Additional laboratory studies to rule out other causes include a complete metabolic panel. 04:29 We talked about the importance of B12, copper levels, but B12 and copper deficiency can present or mimic ALS or motor neuron disease and HIV antibody testing. 04:40 And then MRI is important to again rule out alternative etiologies. 04:45 MRI of the brain and spinal cord may be important to rule out tumors. 04:48 We can look for stroke, inflammatory disorders that could present similarly infectious syndromes that affect the brain or the spinal cord and multiple sclerosis is also an important consideration in a patient presenting primarily with an upper motor neuron pathology. 05:06 And then let's talk a little bit about the management of motor neuron diseases. 05:11 So in terms of management, there is no standard treatment for the underlying disease process for most motor neuron diseases. 05:17 And supportive care for the complications and the symptoms and signs that we see and can develop in motor neuron disease must be a primary focus in managing these patients. 05:30 First thing we think about is physical therapy. 05:33 And stretching and strengthening exercises to reduce stiffness are critical. 05:37 We want to prevent and treat contractures, that continuous tightening of the muscles that results in pain and stiffness and and can limit hygiene and cleaning and those sorts of things. 05:48 We want to help improve posture, prevent joint immobility, slow muscle weakness and atrophy and there are a number of ways that we work with physical occupational therapists and other therapy groups to help support patients with these symptoms. 06:02 Speech therapy is critical for patients with cortical bulbar involvement. 06:06 We want to minimize physical, emotional, and psychological effects of dysarthria, dysphasia, which can result in severe weight loss or nutritional dysfunction, and speech therapy is important for that. 06:18 Speech synthesizers can be used to enhance and maintain communication in patients who have lost the ability to speak. 06:28 We also think of assistive devices, mobility aids, canes, wheelchairs, walkers, motorized wheelchairs, braces and other orthotics can be helpful for patients who have an isolated foot drop or significant weakness or are paralyzed and and need to support patients. 06:45 And these assistive devices are critical in helping to overcome deficits that develop and persist And then other therapies are also important to consider in these patients. 06:57 Feeding tubes may be required to maintain good nutrition in patients with severe dysphasia. 07:02 An early initiation of a feeding tube to maintain nutrition is important for maintaining patient's physical functioning. 07:08 Late initiation of feeding tube does not improve morbidity or mortality in these patients and so identifying the right time to initiate that therapy is important. 07:17 In addition, non invasive positive pressure ventilation or BiPAP and CPAP or other assistive ventilation devices can be integrated into the home for patients with severe respiratory muscle weakness. 07:28 And we often monitor in ALS and motor neuron disease clinic, respiratory function gradually over time and patients who reach a tipping point where their respiratory muscles are developing significant weakness are candidates for home BiPAP and other limp ventilatory support. 07:47 And then what about surgeries? Surgery doesn't fix the underlying motor neuron disease but can help patients with symptoms if the patient has voluntary control of extremities, lengthening procedures to get over spasticity and reduce spasticity or contractures to increase a patient's level of function can be considered for patients that are not able to use the extremity. 08:09 They may need muscle origin release myotomy, tenotomy, neurectomy or other procedures to help reduce pain stiffness and other morbidities from chronic weakness and spasticity.
About the Lecture
The lecture Upper and Lower Motor Neuron Diseases: Diagnosis and Management by Roy Strowd, MD is from the course Diseases of the Motor Neurons.
Included Quiz Questions
MRI of the brain and spine is likely to be normal in which of the following conditions?
- Lower motor neuron disorders
- Stroke
- Multiple sclerosis
- Spinal cord tumors
- Encephalitis
CPAP is a useful treatment for which of the following symptoms seen in motor neuron disorders?
- Respiratory muscle weakness
- Dysphagia
- Trouble ambulating
- Contractures
- Atrophy of the interosseous muscles
Which treatment modality is likely to help patients with ALS who have bulbar symptoms?
- Speech therapy
- Physical therapy
- Occupational therapy
- Orthotics
- Stretching and strengthening exercises of the lower extremities
On exam, what specific finding is indicative of bulbar involvement in a patient with a motor neuron disorder?
- Tongue fasciculations
- Decreased grip strength
- Shuffling gait
- Clasp-knife spasticity
- Decreased sensation on the forehead
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |