Playlist
Show Playlist
Hide Playlist
Testes and Mesonephric Ducts
-
Slides Testes and Mesonephric Ducts.pdf
-
Reference List Embryology.pdf
-
Download Lecture Overview
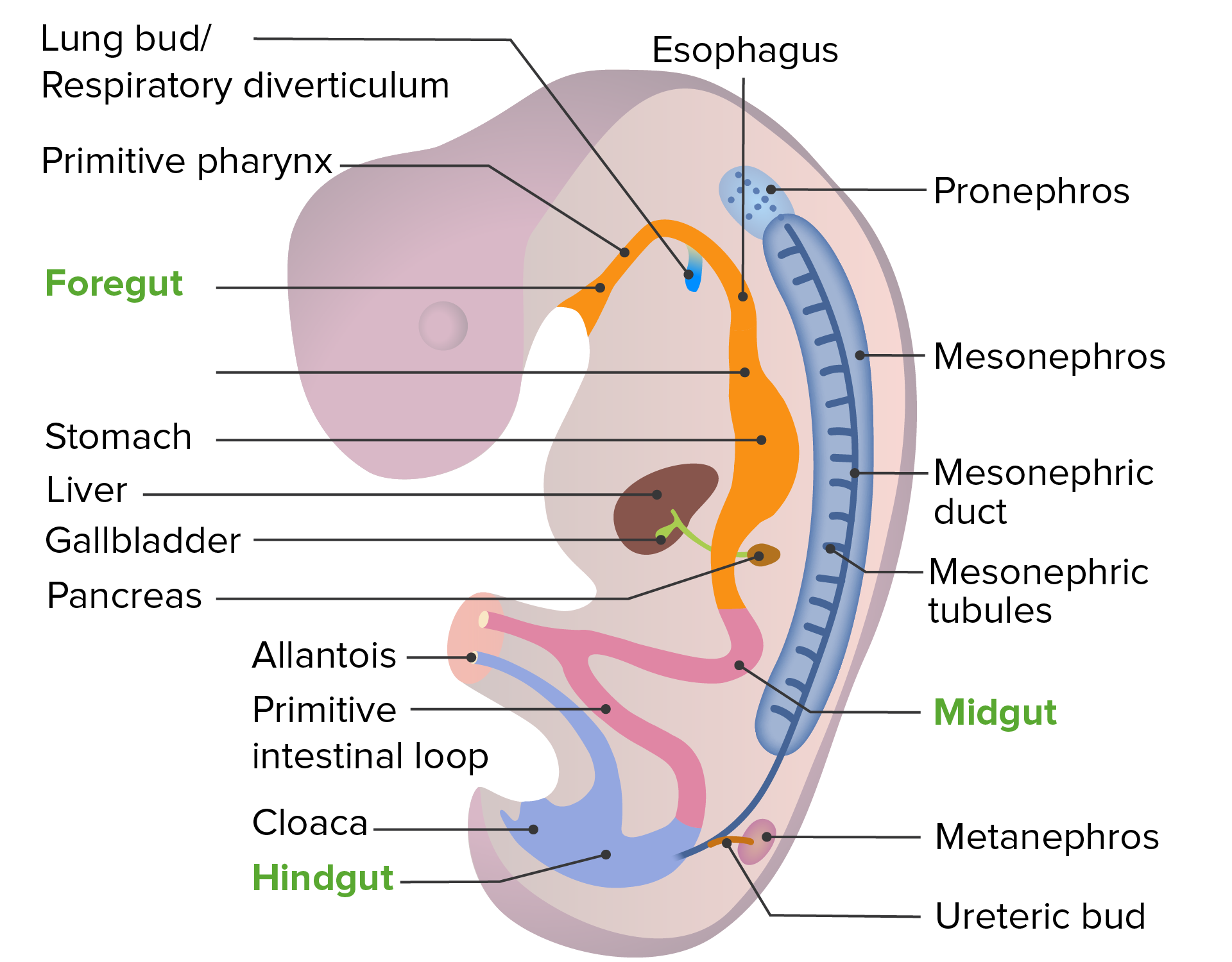
00:01 We will continue discussing the development of the reproductive system, turning our attention now to the testes and the mesonephric ducts that associate with them to create the internal genitalia of the male. 00:12 Initially, if an embryo is XY, has an X chromosome and a Y chromosome, a single gene on the Y chromosome, the SRY gene will transcribe the testis-determining factor. 00:26 This single event is enough to kick start male development as distinct from female development. 00:32 What happens next is that we’re gonna have proliferation of the primary sex cords on the outside of the indifferent gonad. 00:39 These are going to enlarge and expand into the intermediate mesoderm and associated with the cells that have migrated in there a little bit earlier that will eventually become the spermatocytes or the spermatozoa. 00:52 These cords will eventually hollow out to create the seminiferous tubules and other ducts that exist at the microscopic level within the testis. 01:00 The outer coating of the primary sex cords and indifferent gonad will thicken to become the tunica albuginea which is a very dense connective tissue structure that surrounds and protects the testis and will also send some septae or little divisions into the structure of the organ to support it and keep it intact as it develops further. 01:20 Testis-determining Factor and other downstream signaling molecules will kick start the formation of Sertoli cells from the medullary cord and Leydig cells. 01:30 Sertoli cells will associate with the spermatozoa and help them mature whereas Leydig cells will start producing testosterone. 01:37 And during the eighth week of development, the testosterone produced by these Leydig cells is going to be concentrated by the Sertoli cells and a more potent form will be created called DHT, dihydrotestosterone and the enzyme that creates this form of testosterone, DHT, is called 5alpha-reductase. 01:58 Testosterone is going to further develop the mesonephric ducts and actually make them expand and grow into the developing testis. 02:07 Another downstream effect of the Testis-determining Factor is Anti-Müllerian hormone and you may recall that the paramesonephric ducts are also referred to as the Müllerian ducts. 02:19 This Anti-Müllerian hormone is going to cause regression of the paramesonephric ducts leaving just the mesonephric ducts behind to form the ductus deferens and other structures related to the testis. 02:31 So as the paramesonephric ducts disappear, the mesonephric ducts send extensions into the developing testis and form a continuous connection with it and the primary sex cords. 02:44 The mesonephric duct will become the efferent ductules, then the epididymis, ductus deferens, seminal vesicles, and ejaculatory ducts that carry spermatozoa and other secretions of the male reproductive tract all the way to the prostatic urethra from where it can be expelled during ejaculation. 03:03 Tiny little remnants of the paramesonephric ducts may remain as little testicular appendages or sometimes epididymal appendages. 03:11 These are just little remnants that stay attached to the testis and form little tags on them and as with remnants of the mesonephric duct in females, they’re generally fairly asymptomatic unless they develop a tumor or become inflamed in some way. 03:26 So the prostate, the gland itself will develop off of the endoderm that’s lining the urethra and the prostate will grow outwards surrounding the ejaculatory duct and various bulbourethral glands will develop inferior to it. 03:42 The mesonephric duct and seminal vesicles are going to pierce the prostatic urethra and the seminal vesicles will develop outward and then, begin secreting fluid to the ejaculate once the male reproductive system is mature. 03:56 There may be a small little bump on either side of the mesonephric duct and ejaculatory duct’s entry to the prostate called the prostatic utricle. 04:05 That one little bump is the only remnant of the uterus left in the male reproductive tract. 04:11 In some cases, there is a deletion or an inactivating mutation of the S R Y gene. 04:18 This will result in a female phenotype - with a presence of ovaries, uterus, and vagina - despite carrying a Y-chromosome. In other cases, there is insensitivity in the receptor of testis-determining factor. 04:33 Again, a female phenotype will be present despite the carrying of a normally functioning S R Y gene. 04:41 Thank you very much and I’ll see you for our next talk.
About the Lecture
The lecture Testes and Mesonephric Ducts by Peter Ward, PhD is from the course Development of the Abdominopelvic Region.
Included Quiz Questions
Genetically, if the embryo is male (XY), the Y chromosome will transcribe which gene to create the testis-determining factor?
- The SRY gene
- The TDF gene
- The CFTR gene
- The DHT gene
- The PKD-1 gene
Which of the following best describes the difference between the Sertoli and the Leydig cells?
- Sertoli cells will associate with and help the spermatozoa mature whereas Leydig cells will produce testosterone.
- Sertoli cells, but not Leydig cells, are stimulated from TDF.
- Leydig cells will associate with and help the spermatozoa mature whereas Sertoli cells will produce testosterone.
- Leydig cells, but not Sertoli cells, are stimulated from TDF.
- Both the Sertoli cell and Leydig cell are first activated by testosterone.
Which of the following is False regarding testosterone production in the developing male?
- Testosterone is produced by Sertoli cells.
- Testosterone is converted to a more potent form of DHT by the 5-alpha-reductase enzyme.
- Testosterone induces further development of the mesonephric ducts.
- Testosterone is produced by Leydig cells.
- Testosterone is instrumental in the differentiation and development of secondary sex characteristics.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |