Playlist
Show Playlist
Hide Playlist
Tension Pneumothorax
-
Slides 09 PleuralDiseases RespiratoryAdvanced.pdf
-
Download Lecture Overview
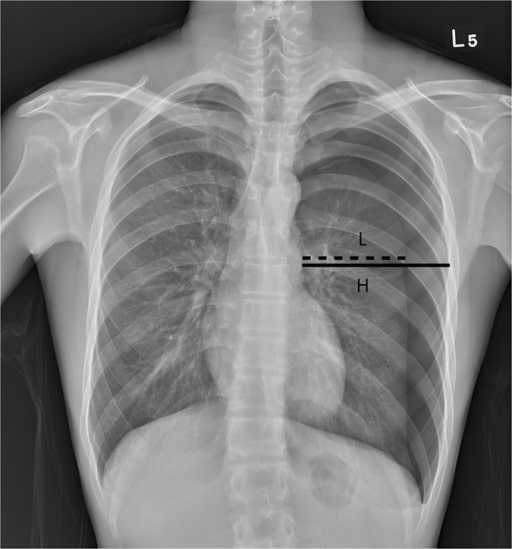
00:02 There is a form of pneumothorax which is a medical emergency, and this is called a tension pneumothorax. In this, small hole in the visceral pleura allows air out when the patient breathes in. So the pleural space expands with air. But when the patient breathes out, the hole is closed down and therefore, the air doesn’t leave the pleural space, and essentially, the patient with every inspiration is pumping out the pleural space with more and more air. 00:31 That means that the pneumothorax is under high pressure and that causes a substantial shift of the lung and the mediastinum away from the side which has been affected by the pneumothorax. And that affects cardiovascular function, because now, it becomes difficult for the venous return to the heart to supply blood to the heart because of the increased pressure in the system. That means the patient will present with hypertension, and this is an incredibly dangerous situation that requires very rapid treatment. 01:02 So, how do you recognize somebody with a tension pneumothorax? Well, first of all, they’ll be in severe respiratory distress, they’ll have low blood pressure, every time they sit up, they will be fainting potentially, and there’s marked tracheal deviation when you examine them. The chest X-ray will show an obvious pneumothorax, excessive mediastinum shift, and the diaphragm, instead of being dome shape will be flattened, and that represents the pressure that is present in the pleural space in a tension pneumothorax pushing the diaphragm down, and an extreme surface dense of the diaphragm will be inverted. 01:38 Treatment is very simple and very obvious. All you need to do is equalize the pressure in the pleural space with atmospheric pressure. And to do that, you just need to make a hole. 01:49 So a rapid treatment is insertion of a wide bore cannula in the second intercostal space in the midclavicular line. That’s chosen as a relatively safe place to put a needle the air is likely to be most marked at the top of the lung. If you put the needle in there, you’d equalize the pressure between the pleural space and atmosphere and the tension pneumothorax problem resolves. It doesn’t resolve the pneumothorax, but it resolves the problems of the pressure, and the patient will then need to have a chest drain inserted after that. So, the next section of the talk is about bacterial infection and pleural effusions. I’m not going to talk about tuberculosis then. This is all about pyrogenic bacterial infections. So I mentioned before pleural effusions often occur in patients who’ve had pneumonia. And those initially are called simple para pneumonic effusions. They occur in about 30% of people with pneumonia, and those represent areas of information overlying the area of consolidation in the lung with pneumonia with a small amount of fluid formation, but the fluid is sterile. The bacteria have not translocated across from the lung to infect that pleural space. And these small sterile effusions are not really necessarily to treat them. 03:10 However, in some patients, that small sterile effusion gets bacteria into it and then it becomes what we call a complex para pneumonic effusion. They tend to be bigger in size. 03:22 They get adhesions between the visceral and parietal pleura and there is bacteria identifiable in the pleural fluid. And these patients do need to have that pleural space drained and prolonged antibiotics to ensure they don’t develop the last step which is an empyema where they have frankly purulent pleural fluid. This is a chest X-ray which shows somebody with a loculated pleural fluid of that right lung. Previously, they just had right lower lobe pneumonia and this is the development of empyema as a consequence of a parapneumonic effusion that has become infected.
About the Lecture
The lecture Tension Pneumothorax by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Pleural Disease.
Included Quiz Questions
Which of the following conditions is NOT associated with an increased risk of pneumothorax?
- Pulmonary embolism
- Marfan syndrome
- Bullous lung disease
- Smoking
Which option is the best for immediate treatment of a tension pneumothorax?
- Rapid insertion of a cannula into the 2nd intercostal space in the midclavicular line
- Controlled oxygen with an FiO2 of 100%
- Immediate intubation and ventilation
- Treatment with cardiac inotropes
Which of the following features more reliably indicates tension pneumothorax in a patient with pneumothorax?
- Hypotension
- Tachypnea
- Tracheal deviation
- Decreased vocal fremitus
- Decreased breath sounds
Which of the following is NOT a classic X-ray finding in a patient with tension pneumothorax?
- Pleural effusion
- Pneumothorax
- Tracheal deviation
- Flattening of the diaphragm
- Mediastinal shift
Which of the following is the best location for insertion of a needle in a patient with tension pneumothorax?
- Second intercostal space in the midclavicular line
- Fourth intercostal space in the midclavicular line
- Second intercostal space in the parasternal region
- Fourth intercostal space in the parasternal region
- Subxiphoid region
Which of the following descriptions is NOT indicative of complicated parapneumonic effusion?
- Sterile
- Loculated
- Purulent
- Large
- Positive Gram stain
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |