Playlist
Show Playlist
Hide Playlist
Telomerase and MicroRNAs
-
Slides CP Neoplasia Genetic alterations in malignancy.pdf
-
Reference List Pathology.pdf
-
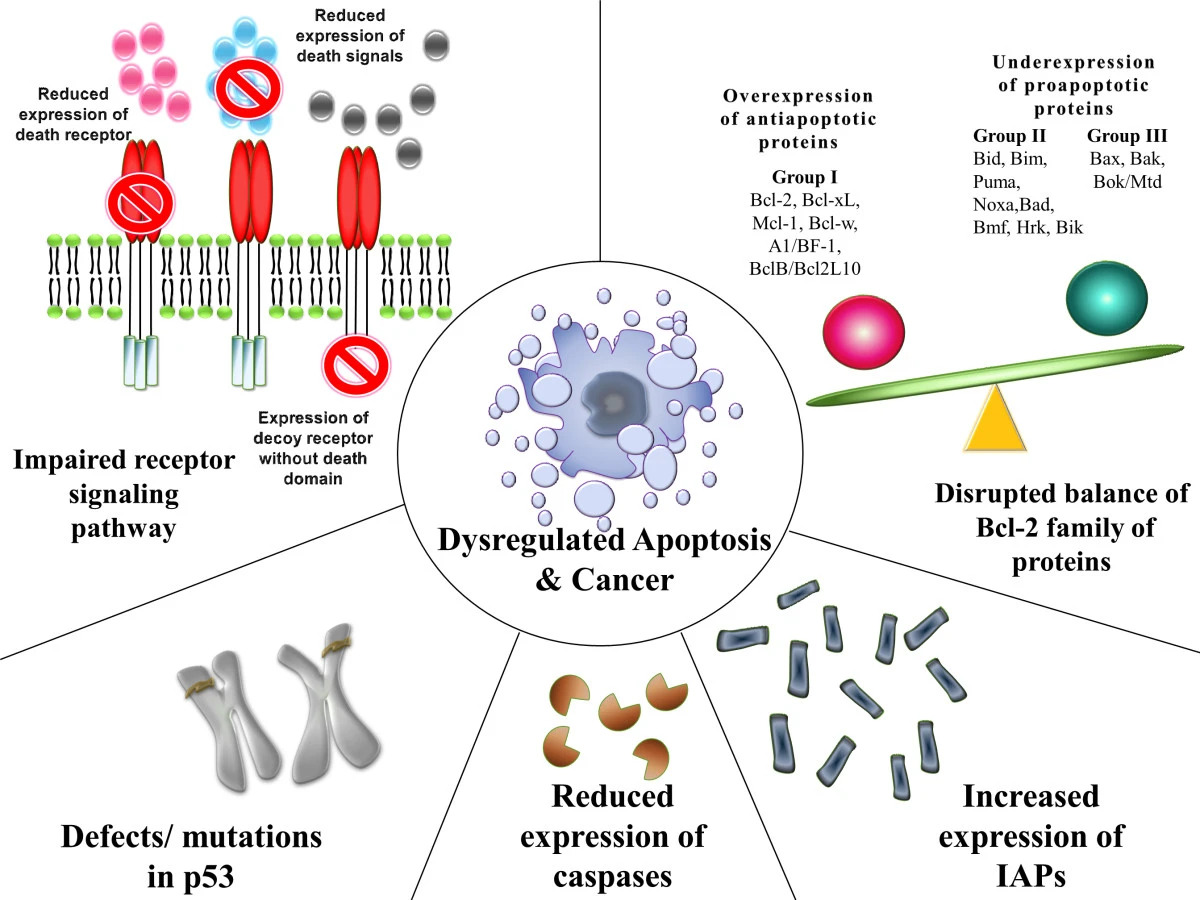
Download Lecture Overview
00:00 Telomeres. So telomeres are like the little plastic things at the end of your shoelaces, that's how they're described and they are at the end of the chromosomes. They are repeated subunits of nucleotides. And because of the way that we replicate chromosomal material, each replication leads to a little bit of shortening of the telomere. So the telomere just protects the chromosome through multiple cell cycles, but at some point it will become so short that now we can no longer have the cell go through replication successfully. 00:36 So, in cells we want to have infinite capacity to turn over such as germ cells and stem cells. 00:42 Those cells have their telomeres constantly renewed by a telomerase. So we have an enzyme that will be able to add more DNA back every time that we have a replication so these cells are essentially immortalized. However, in every other somatic cell, normally the telomeres will get shorter, and shorter, and shorter. After about 50 to 70 replications, they have shortened enough and the p53 pathways are activated by the sensors ATM in red and all those other things will sense that we have now telomerase insufficiency. We will activate the p53 pathway and the cells will go through a proliferative arrest or they may even die. And that's part of normal cellular senescence. We just are losing telomeres that aren't being replaced. So, as I said before, normal germ and stem cells have the enzyme telomerase and can go through infinite essentially cell cycles. So, in order for cancer cells to continue to proliferate ad nauseam would be immortalize, they need to reactivate the telomerase and they can do that, that can be one of the mutations that occurs, that telomerase gets reactivated. It maintains the telomere length and therefore giving the cells increased replicative potential. Okay, so let's think about how this works just briefly. So, normal cell senescence occurs this way. We have cells that will replicate. You can see the chromosomes. They are kind of a simplified version. And they replicate and after about 50 to 70 replications, the telomeres at the very end becomes so shortened that we go through replicative senescence. Basically p53 pathways are activated and it turns off cell cycle. We don't want to have more proliferation of these chromosomes because each time we proliferate them now or replicate them now, they are going to in fact be losing genes, actual genes at the end because the telomeres are not there to protect it. So, that's the normal pathway with cellular senescence. If you don't have p53, however, and a cell has been replicating all along, then you can no longer have the repair turn off that would make the cells stop in a senescent cell cycle. And you can, as the cell tries to salvage these genes, the ends become rather sticky and you end up with dicentric chromosomes. That is either 2 cm and we've joined the ends where they're out the telomerase anymore to each other. 03:30 So we have made some very aberrant chromosomes. Now, all the genes are still there being expressed at this point, but they are now in a position as we go through the cell cycle as we replicate everything through metaphase, through anaphase, and then as we separate those we can get some very abnormal breaks. We can pull them apart in abnormal ways. 03:54 Now, at this point, that's a really screwed up genome. And if we don't have any telomerase, then we'll have a mitotic catastrophe. On the other hand, if we do have telomerase, we can put telomeres on the ends and now we can happily replicate those chromosomes even though they're aberrant and with many abnormal translocations. So that's how telomerase from tumor cells can drive cells away from that mitotic catastrophe in cell senescence and make them immortal. And finally, let's finish up with micro RNAs because micro RNAs can do all of the above. So micro RNAs are small, non-coding RNA oligonucleotides about 22 nucleotides in length. There are well over a hundred now that have been identified. 04:52 Previously we thought this was all just junk RNA and in fact it's not, it's regulatory RNA. 04:58 And they regulate gene expression by either translational repression or by causing the destruction of normal messenger RNA. So how do they do this? So if you have the normal genome, you can form through transcription some primary miRNA. So that's primary PRI micro mi, RNAs. Those get further processed to form through the Drosha and Dicer and you don't need to memorize those, they're just fun names to say. They get processed to a micro RNA, a mature micro RNA in the cytoplasm that can bind to homologous sequences in the cytoplasm and either silence the RNA by cleaving it or more upstream can actually stop the translation of the new mRNAs. Okay, so let's look at this in a little bit more detail. 05:59 So, here we have a potential oncogene and the normal micro RNA might be able to be formed into the pre-micro RNA, go out into the cytoplasm, and then interact with that oncogene if it's being overexpressed and cause its repression. That would be the normal thing. But if I have a mutation in that micro RNA or if I have a mutation in the target sequence on the oncogene that I won't get as much destruction as should normally happen I will get some but I won't get as much as I expressed. So, in this case, I have reduced translational repression from either mutated or inadequate micro RNAs. And that will functionally look like oncogene overexpression because I'm not controlling it, I'm not eliminating it, and that will drive all of the variety of increased proliferation, decreased apoptosis, etc. etc. etc. Because we have now more activity at that oncogene not be inhibited by the micro RNA. So that's what happens with an oncogene and micro RNA. 07:11 What about tumor suppressor? So, normally you might have minor amounts of the micro RNA that are regulating tumor suppressor gene expression. But if I make a lot more of it or I don't appropriately get rid of it, then I will have too much suppression of the tumor suppressor genes. I'll give too much binding, I will break all of that down and now we won't have enough of the tumor suppressor genes. That inadequacy of the tumor suppressor genes can also drive then all of the changes we talked about and promote oncogenesis. 07:51 So, it's kind of an overview. Genetic defects and malignancy. You can have defects in the growth factor receptor where it's constantly turned on even if there's no ligand bound to it. You can have inhibitors of signal transduction that are lost or are abrogated, and we talked about the RAS oncogene. You can have inhibitory receptors, lose their normal inhibitory capacity. Additional way is that you can have genetic defects and malignancy if there is an abnormal association with the extracellular matrix or proteins that regulate that interaction. And normally by virtue of molecules like cadherins that bind to beta-cathenin and then in turn to APC, we can have mutations in that complex that lead to proliferation. 08:46 APC is the adenomatous polyposis coli protein and when it is mutated it is no longer inactivated as is the normal pathway which will lead to proliferation. You can also have loss of apoptosis genes. You can have increased expression of your CDK and cyclins or diminished expression of the inhibitor proteins for the cell cycle regulation. Your DNA repair may be abnormal with the BRCA1 and 2 mutations. Cell cycle regulators, cyclin D, CDK4, all of those may be aberrantly expressed and/or not turned off appropriately. You can also have loss of the cell cycle inhibitor retinoblastosis, RB. You can also have cell cycle and apoptosis repair inhibition through mutations in p53. So there are variety of ways that a cell can go bad and notably in most cancers it's multiple of these pathways that have occurred because of genetic instability. And with that, we completed a fairly complex set of concepts relating to malignancy and I encourage you to review this again so that hopefully each time through you go "Oh yeah, okay I've heard that, that makes sense." See you next time.
About the Lecture
The lecture Telomerase and MicroRNAs by Richard Mitchell, MD, PhD is from the course Neoplasia.
Included Quiz Questions
In cells with short telomeres, what protein is activated and stops the cells from proliferating?
- p53
- p21
- MYC
- RAS
- p17
What is the approximate length of microRNAs?
- 22 nucleotides
- 200 nucleotides
- 22 genes
- 200 genes
- 100 nucleotides
Which of the following is the mechanism through which microRNA regulates gene expression?
- Translational repression
- Translational promotion
- Transcription repression
- Transcription promotion
- DNA repair
What protein inhibits signal transduction?
- NF-1
- RAS
- TGF-B
- Cadherins
- APC
Which of the following proteins is involved in signal transduction?
- RAS
- TGF-B
- APC
- p53
- BRCA1
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Amazing explanation, illustrations and pictures. Really love Lecturio. Thank you!
In the explanation of miRNA, on the most important part of it, he sort of gets tangled explaining. I couldnt understand the only part i want interest of in the video. Please refilm this video, it is unclear.