Playlist
Show Playlist
Hide Playlist
Tachycardia: For The Boards
-
Slides Tachyarrhythmia MultifocalAtrialTachycardia CardiovascularPathology.pdf
-
Download Lecture Overview
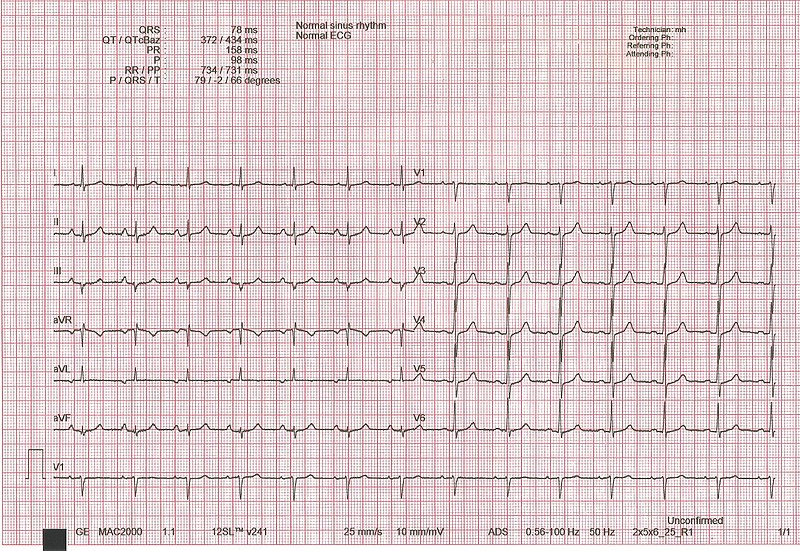
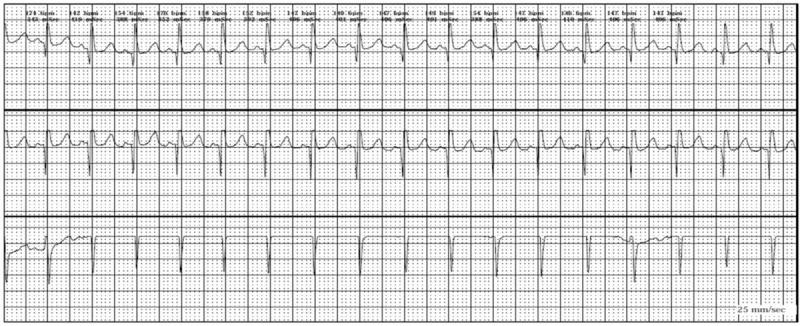
00:00 Now, overall, these were things becoming important. The important points of what you want to know about ECG are the following. What is the rate that you are looking for? How do you find the rate? You are going to take a look at the space or the span between the R waves. Think about the R wave, first major positive deflection and what is my phone number? 300-150-100, 75-60-50 keep saying it over and over again, practice them here, practice with me so that you get those firmly etched in your head. For every line, that is seperating the R wave, you are going from 300 beats per minute all the way down to six lines seperating R wave resulting in brady and 50 beats per minute. That is your rate. Is it regular or irregular? Mean to say, let me give you prime example. An atrial fibrillation was it irregular or regular type of rhythm that you saw on that lead? Atrial fibrillation, you had a P wave, which was fibrillating and wavy and it was irregular. 01:08 The QRS complex showed up randomly. Whereas an atrial flutter, I will show you at a 2:1 type of ratio. That type of pattern was two P waves to every QRS complex and that was irregular rhythm. You see that now. Crystal clear. Now, what about the QRS complex. Is it narrowed or is it perhaps widened? So far what we have seen is a widening of a QRS complex. 01:35 Prime example, WPW. Wolf-Parkinson-White. What caused that widening of that QRS complex? QRS complex, the delta wave. What happened to PR interval in WPW? It got shortened. Are you able to do with that quickly? Yes, you are. You will get it. 01:50 Clinical picture. What about your patient hemodynamically? Is your patient hemodynamically stable? If they are, just maybe you have enough time and you have the luxury of using medical cardioversion. In other words drugs. Or if your patient is hemodynamically unstable, what does that mean to you? There is syncope. There is dizziness, decreased cardic output. There is dyspnea. Things are backing up into the lungs. Hemodynamically unstable. Hypotension and now are you thinking about what kind of issue or what kind of cardioversion? Electrical. 02:26 Blood pressure, consciousness, distress that to you should indicate in the setting of an arrhythmia as to whether or not your patient is hemodynamically stable or unstable. Know this forever more not only you are going to save the lives of your patients, but really you are going to build confidence in yourself to make sure you can approach any scenario and you can walk away knowing that you have done a good job. 02:51 Now, what else do you want to know? Clinically unstable, shock is which you are worried about. The heart is failing. Cardiogenic shock. How is the patient going to feel with this type of shock where the heart is not pumping properly? You tell me. 03:07 Decreased cardiac output so therefore what happens to blood pressure? Decreased. Tell me about your baroreceptor reflex. Decreased firing, increased sympathetic activity. With that increased sympathetic activty, how is the skin going to feel? Cold and clammy and there is going to be diaphoresis. Are we clear? Why? Because increased sympathetic activity. 03:31 Shock, hemodynamically unstable. Narrow complex, regular tachy and clinically stable. What about this patient? Vagal maneuvers. 03:41 Let me give you big one physiologically, right here. Carotid massage. A carotid massage has a particular component in the carotid in this components called the sinus and this sinus houses what exactly? The carotid sinus houses baroreceptors. Chemoreceptors are in your bodies, aren't they? So, here, let us focus on the carotid sinus that contains baroreceptors and your patient has regular tachy, narrow complex of your QRS complex. Clinically stable there is no major hypotension. Distress not so much and the syncope and dizziness not there. We are okay. Shock, no. Obviously not. Stable. You want to slow down the heart rate. Are you seeing it now? You massage the carotids. 04:35 When you have increased blood pressure and you are stretching your blood vessel, you are stimulating the baroreceptor, outcomes to parasympethetic. 04:45 You by performing carotid massage are mimicking high blood pressure, increased blood flow. 04:53 So hemodynamically stable, be careful when you do carotid massage, you would expect the heart weight to decrease. Valsalva, what does that mean? The same thing in which we talked about the early with valsalva when we did phase II and such and doing a maneuver where I decreased preload. Valsalva could also result in maneuvering in vagal response. 05:15 Adenosine IV unless which one please? WPW. We are also going to avoid WPW one more time. 05:21 You tell me about dig, dig is the big one. Technically calcium-channel blockers as well. May terminate your reentry tachycardias. You pay attention to RT right now. That is good enough. Reentry tachycardia. We will make flutter waves more clear. Adenosine because you are slowing down conduction. May not terminate atrial tachy, but will slow AV conduction so that abnormal P waves focus is what you are paying attention to. Is that clear? So you are really slowing down the AV conduction, but may not necessarily terminate the atrial tachy. We will transiently slow atrial fibrillation and as we move on to clinical medicine and those of you that are already cardiologists, those of you that have done your cardiology rotation, you know exactly what I am referring to. Many times you use adenosine to do what? Diagnose your patient, right? You use adenosine to see as to whether or not by giving it, have you slowed down the heart rate just a little bit? And if you have done so, well maybe you have diagnosed your patient with an SVT of some type. Keep that in mind. Transiently, will slow down atrial fibrillation.
About the Lecture
The lecture Tachycardia: For The Boards by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
What is the heart rate with an R–R interval that spans 3 large boxes on an ECG?
- 100 bpm
- 150 bpm
- 75 bpm
- 60 bpm
- 300 bpm
What is the most appropriate step in the management of a patient presenting with a narrow complex tachycardia who progresses into severe hypotension with symptoms of dizziness and dyspnea?
- Cardioversion
- Propranolol
- Procainamide
- Adenosine
- Carotid massage
What is the first step in the management of a clinically stable patient with narrow complex tachycardia?
- Carotid massage
- Adenosine
- Digoxin
- Beta blockers
- Electrical cardioversion
Adenosine is contraindicated in which of the following conditions?
- Wolff-Parkinson-White syndrome
- Atrial tachycardia
- Atrial flutter
- Atrial fibrillation
- Ventricular tachycardia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |