Playlist
Show Playlist
Hide Playlist
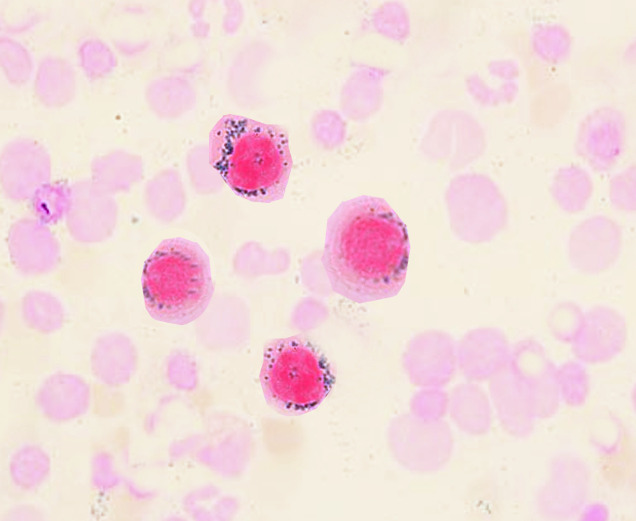
Sideroblastic Anemia: Nucleated Red Blood Cells in Bone Marrow
-
Slides Sideroblastic Anemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:01 Students always confuse the amount of iron in microcytic anemia. 00:06 What does that even mean? You shall see in sideroblastic. 00:10 There is absolutely no issue with iron deficiency, yet it’s microcytic. 00:15 Let’s begin with MCV being less than 80 and we also began here with a pretty prolonged and elaborate conversation and discussion of things that you need from biochemistry so that the pathology makes sense. 00:30 Not to worry, I’m going to walk you through every step of this. 00:33 So that by the time you go from start to finish, you have a complete picture of what sideroblastic anemia means and along the way, you are then – I am then going to point out to you a couple of other interesting points of what’s known as you porphyria pathway and porphyria diseases from biochem. 00:55 Okay. 00:56 First and foremost, please know where we are. 00:59 We’re in the bone marrow and the fact that you even have a nucleus in an RBC is -- Well, what kind of RBC would this be? Tell me about your RBC that’s in circulation. 01:10 It is naked. 01:11 What does that mean? It has no nucleus and it has no mitochondria. 01:16 The only method by which iron can then derive its energy from would be anaerobic glycolysis and it would then protect itself by utilizing what’s known as your G6PD pathway and your hexose monophosphate. 01:30 Are we clear about what a normal RBC should look like? And I showed you a picture earlier in iron deficiency with the normal, where it looks pretty transparent. 01:38 The only thing that it truly contains is hemoglobin. 01:41 Okay. 01:42 Enough discussion about normal RBC. 01:44 So this is a nucleated RBC and if you were to find this in your circulation, that definitely would mean pathology. 01:51 But here, let’s go with normal though. 01:53 You have a nucleated RBC and this would be located where? Good, in your bone marrow. 01:58 Remember that RBC goes through the production and the progression into maturity which means that you have your erythroblast and normoblasts, reticulocyte, and then you have your – everything has been plucked out, meaning that the nucleus has been plucked out and the mitochondria is not there anymore. 02:16 And so what this is is – The gray shaded area that you see is going to be inside the mitochondria. 02:24 And then, we have the cytosol, which you see outside here at the bottom. 02:28 You see that, okay? Identify where you are. 02:31 At first, we’re in our bone marrow and we’re trying to produce what? We’re trying to produce hemoglobin, okay? So in the nucleus, and so that we can properly, properly, equip the RBC with the hemoglobin that it requires for oxygen transport basically. 02:46 That’s what an RBC does. 02:48 It’s the truck, right? The transporter of oxygen to your tissue. 02:52 Let's begin at the top. 02:53 Now, so here’s my transferrin and it’s a delivering. 02:55 I’ve told you this a few times now. 02:57 The transferrin is going to then deliver the iron to the bone marrow, doesn’t it? In the meantime though, in your RBC, you can have bone marrow macrophages and we’ll go ahead and call that ferritin or iron containing substances. 03:11 Keep that in mind please. 03:13 Because that’s important. 03:14 Bone marrow macrophages, which is then responsible for holding on to some of that iron. 03:19 That becomes important. 03:20 Okay, next, as you bring in the iron, we’ll begin the process biochemically by having succinyl-CoA and glycin. 03:28 If you want to remember those, that will be fantastic. 03:31 Now, what you truly want to remember here are going to be these. 03:34 You definitely want to know from pathology, vitamin B6 and you want to know ALA synthase, which is rate-limiting enzyme. 03:42 When you do biochemistry, please make sure that you begin every single pathway that you need to know, the glycolytic pathway, gluconeogenic pathway, the HMP shunt pathway, whatever it may be. 03:51 And you know that rate-limiting step or rate-limiting enzyme because that becomes important for what? It’s called feedback mechanism. 03:59 So whenever you get questions about feedback mechanism, if your producing enough of your product and you produce too much of that product, what kind of effect do you have on your rate-limiting enzyme? Good. 04:08 Negative feedback. 04:09 You decrease. 04:10 Why do you want more when you already have so much product? Clear? But if you don’t have enough product, then what do you want to do? Then, obviously, you want to stimulate the rate-limiting enzyme. 04:19 Are we clear? So it’s important that you know that type of relationship for sure. 04:25 Okay, so then you have the rate-limiting enzyme, ALA synthase, and we have vitamin B6. 04:30 What I’m going to do first is lay down the normal foundation and then we’re going to quickly put in the pathologies and you see as to how this works. 04:37 With the synthase, you end up forming aminolevulinic acid. 04:40 Say that three times fast. 04:42 I can’t. 04:42 I’ll do it once. 04:43 Aminolevulinic acid. 04:45 Next, you come out into the cytosol. 04:49 And you have an important enzyme here. 04:50 This is not the rate limiting enzyme. 04:53 I do wish to point out to you, this will make your life a little bit easier, Pb in your periodic table is lead. 05:01 Why in the world did I say lead like that? Because lead, D, that it ends in is the enzyme ALA dehydrotase. 05:11 Students often get dehydrotase confused with synthase. 05:15 No longer. 05:16 So whenever you have lead, it is going to inhibit ALA dehydrase. 05:20 Do not choose ALA synthase, is that clear? So we’ll talk about synthase more when the time is right. 05:26 You’re going to end up forming porphobilinogen. 05:30 Okay. 05:31 So why did I pronounce this -- Why did break it up that way? -Ogen means to you what? Weak, weak, weak, weak, weak. 05:38 What do you mean? Trypsinogen, pepsinogen, wherever else, or fibrinogen, right? So you need to cleave off that –ogen so that you can form your proper porphyrins. 05:50 So there’s many steps here. 05:51 Hence, you find the dash lines. 05:53 And you tell me which is the most common type of porphyria disease. 06:01 Good. 06:01 Porphyria cutanea tarda, isn’t it? So your porphyrias, the one that you definitely want to know. 06:07 Well, there’s two that you definitely want to know, but the most common will be porphyria cutanea tarda. 06:13 In your porphyria cutanea tarda, what component of that did you want to remember from biochemistry? The cutanea, why? How is the patient going to present? "Doc, I have a rash." Tell me about this rash "Well, when I go out and sunbathe, oh my goodness, this blister develops and it hurts." It hurts. 06:35 So painful blister upon exposure to UV, ultraviolet, is the history that that patient is going to give you for porphyria cutanea tarda, and with this, you are then going to then look for maybe the enzyme deficiency called UROD. 06:49 And what you are then going to find in the urine. 06:52 The second type will be known as acute intermittent porphyria. 06:56 Another one that you want to know, well, luckily with acute intermittent porphyria, you’ll be paying attention to letter P, what does that mean? Pink urine. 07:04 A little reddish. 07:05 You’ll have abdominal pain. 07:07 Ouch! Maybe a little crazy. 07:10 What’s that? Psychosis. 07:11 Remember psychosis begins with the letter P. 07:13 All right, so many of these issues that you have with AIP, acute intermittent porphyria, will begin with the letter P. 07:20 So those are discussions that you’ve had in biochemistry, at least know two of these. 07:24 Porphyria cutanea tarda and number two, acute intermittent porphyria. 07:29 Know the enzymes that are deficient in those conditions and you’ll be in fantastic shape. 07:35 Let’s continue forward. 07:36 What are you trying to form here? Oh, I do believe we’re trying to form hemoglobin. 07:40 Where am I? Bone marrow. 07:42 What kind of cell is this? A nucleated RBC. 07:46 Let’s go back into the mitochondria and whatever, you have protoporphyrin IX, so be it. 07:53 But then you have this enzyme called ferrochelatase. 07:55 That you’ll want to memorize for sure. 07:58 We’ll talk more about that later as you can see here. 08:00 Lead is also going to interfere with that, and then what have you formed finally? Heme. 08:06 Are you done? No. 08:08 Remember that transferrin that was bringing the iron? That iron has to be incorporated into the heme so that you can form the heme component only of hemoglobin. 08:18 Are we clear? So all we’ve done thus far is form heme. 08:20 What’s left? The globin. 08:23 Tell me about the globin. 08:25 The globin is the gene. 08:26 Where are you going to get those genes? G, globin. 08:31 G, gene. 08:33 Obviously inherited. 08:35 Alpha, beta, delta, gamma. 08:36 See that in parenthesis. 08:37 Alpha, beta, delta, gamma. 08:40 Greek letters. 08:41 So you have to know Greek, you have to know Latin, you have to know medicine. 08:44 I mean really – It’s endless, isn’t it? It’s rather interesting. 08:47 So now, you have alpha, beta, delta, gamma, is that important? Oh, are you kidding me? Have I told you anything that’s not important? Exactly. 08:55 So here, when you have hemoglobin A, you have the heme formed by the porphyria pathway and the globin in which the genes have then been given to you. 09:06 In a fetus, what kind of hemoglobin do you have? Fetus. 09:10 Hemoglobin F. 09:12 What’s my Greek salad there? My Greek salad as a fetus is alpha and gamma, right? As we’re born and delivered and such, approximately, oh, maybe about two to three maybe maximum of four months, you convert all of your hemoglobin F into hemoglobin A. 09:35 What’s your Greek salad for hemoglobin A? Alpha and beta. 09:39 Alpha and beta, are we clear? So as long as all of this is occurring properly with the biochemical pathway in genetics, boom, they came together and they form hemoglobin. 09:50 So far, all of the microcytic anemias that we’ve done have been heme diseases. 09:56 These include, number one, iron deficiency, anemia of chronic disease, sure, but it’s dealing with iron but also chronic diseases. 10:04 And then here, ladies and gentlemen, welcome to sideroblastic anemia. 10:10 So in sideroblastic anemia, what’s my problem? Let’s go back to the beginning. 10:14 So start is on your left. 10:17 The finish of this interesting porphyria monopoly game is going to be the hemoglobin. 10:23 Start to finish. 10:24 Left to right. 10:26 So in the beginning, let’s say that you had a patient who had night sweats, fever, weight loss. 10:31 On your chest x-ray, you ended up finding these interesting nodules or maybe CT that’s showing you nodules. 10:38 With that type of history and the fact that imaging study of CT, more likely to have maybe something like TB, right? So obviously, you confirm this and you find acid-fast positive organisms. 10:51 So here’s mycobacteria TB and the patient now begins on a RIPE regimen. 10:56 What’s RIPE? R- rifampin. 10:58 I- INH, a.k.a., isoniazid. 11:03 P- pyrazinamide. 11:04 E- ethambutol. 11:07 Why do have INH here? Because INH along with the drug, you have to give pyridoxine. 11:15 What’s another name for pyridoxine? Oh, yeah, that’s vitamin B6. 11:20 Know both names please. 11:22 Now, point is this, say that you have a scenario in which the individual has not been ordered or instructed, whatever, to take the B6 with INH. 11:31 What happens? You become B6 deficient. 11:33 If you become B6 deficient, then what happens? My rate limiting enzyme isn’t working properly. 11:39 Wow! So if that isn’t working properly, you’re stuck. 11:43 You can’t even move past your step of Succinyl-CoA and glycine. 11:47 Can you form heme? Nope. 11:50 If you can’t form any heme, what happens to my state of iron? Too much. 11:56 So what do you think this iron is going to do? What is this that we’re seeing here? A nucleated RBC. 12:01 So what is this iron going to do? It is going to then wrap itself around your nucleus, isn’t it? What is that called? Ring sideroblasts. 12:11 Holy cow! Everything’s now coming together. 12:14 It’s making sense. 12:16 So therefore is there any iron deficiency here? No. 12:20 It’s the fact that no heme was formed. 12:24 So the iron comes in and it’s lost. 12:26 I don’t know where to go. 12:27 I don’t know where to go because there’s no heme. 12:30 Are we clear? So what does it do? It forms a siderocyte. 12:34 What’s a siderocyte? It’s just an RBC, which has too much iron in it. 12:38 A sideroblast, a ringed one, is one in which around the nucleus, it forms a beautiful ring. 12:44 And if you do a Prussian blue, obviously, you’ll find that to be lit up. 12:47 I’ll show you a picture. 12:48 You see that? So a sideroblastic anemia isn’t specific. 12:52 Is it only one disease? Is it only one disease? Sideroblastic is an umbrella of diseases. 12:57 I’ve only given you one, INH. 13:00 Who’s my second one? Well, my second scenario, let’s say that there’s a baby. 13:04 And what’s this baby doing? Well, in the lower socioeconomic type of environment, unfortunately, or even like old homes, huh? Even old homes actually northeast if you go to the New England area, Boston and such, the actual communities in which children are not allowed to live. 13:24 Not because of discrimination or not because like, “Oh, I don’t like children, so no children in my community.” No, no, not because of that. 13:31 It’s the fact that the children are not allowed in these old homes because if the paint starts chipping, what are they going to do? They put everything in their mouth. 13:39 “Look at that, there’s a –“ Well, they can’t talk to you, right? They’re going to crawl over to the paint chip. 13:43 See me crawling? And you’re going to put a paint chip in my mouth. 13:46 Uh-oh. 13:47 What happens? Not good. 13:50 This child is going to grow not too tall. 13:53 The child’s going to go to school, not do too well. 13:57 The child gets older and what happens? Maybe limp wrist. 14:02 What does that mean? Something like wrist drop, maybe foot drop. 14:06 See what I’m getting at? Maybe that’s neuropathy. 14:08 Uh-oh. 14:09 Later on, adult life, also there might be issues with increased creatinine. 14:14 What’s that called? Lead nephropathy. 14:17 That’s what I’m getting at. 14:18 This is all lead poisoning, isn’t it? So look for – Even to this day, ladies and gentlemen, where you find children that unfortunately might just put anything in their mouth including lead chips or paint chips. 14:30 And so therefore, sometimes if with that type of history, with maybe lower socioeconomic type of environment, where they’re eating old paint, all they have to do is show up with abdominal pain, with that type of history, no doubt, your patient has lead poisoning. 14:46 What kind of anemia is this? Good. 14:48 Sideroblastic anemia. 14:50 Most likely here, the MCV is going to be less than 80, it doesn’t have to be at all times. 14:55 But just to make your life a little bit easier though, that’s the full history of your patient. 14:59 They’re not going to go crazy on the categorization so much because it could actually micro or even normal. 15:06 But the history is going to tell you everything that you need. 15:08 And what about that INH? Well, that INH, the synthase wasn’t working properly because there’s no B6. 15:14 So two down. 15:15 Two what? Two causes of sideroblastic. 15:18 What kind were these? Acquired, right? INH, therapy for tuberculosis. 15:24 Number two, lead poisoning. 15:26 Let’s go to the most common type actually. 15:28 The most common type is one in which alcohol is involved. 15:31 Just keep it simple, alcohol is a mitochondrial poison. 15:35 It will damage the mitochondria. 15:37 So therefore, if your mitochondria isn’t functioning properly, you’re not able to form heme, are you? Nope. 15:44 So what do you have? You have sideroblastic anemia. 15:46 Acquired type. 15:47 “But Dr. Raj, I thought alcohol could cause non-megaloblastic anemia, macrocytic?” It does. 15:53 “I thought, Dr. Raj, alcohol could consume folate, may result in megaloblastic macrocytic anemia?” Yeah, it does. 15:59 And alcohol may cause mitochondrial poisoning and result in sideroblastic anemia. 16:04 So you want to be very, very careful with alcohol because it could be any number of anemias. 16:10 It all depends as to what your questions and this situation is going for. 16:15 Three down, these were acquired. 16:18 Then, could you then be genetically deficient of the rate-limiting enzymes? Sure. 16:23 So you’re genetically deficient of the rate-limiting enzyme, which one is this? ALA synthase. 16:29 Wow! So there is a genetic one that you want to know? Yeah. 16:33 You want to know the most common genetic deficiency causing sideroblastic anemia and that would be ALA synthase deficiency. 16:40 And there’s one other that we’ll talk about a lot more when we get into WBC pathology. 16:45 And that is going to be something called myelodysplastic syndrome. 16:49 Your myelodysplastic syndrome, there’s a type of refractory anemia of ring sideroblast. 16:55 Rare, but actually we’re finding more and more about this. 16:59 Hence, it is absolutely important for you to know. 17:01 So I’ll mention it as we go through here. 17:03 The last little point that I wish to bring to your attention, ladies and gentlemen, if you go all the way to the right and to the top and take a look at the globin chains. 17:12 If you’re missing alpha and beta, at a later discussion, we’ll take a look at our fourth and final type of microcytic anemia, which is then going to be dealing with your thalassemias. 17:20 A beautiful picture, ladies and gentlemen, of really wonderful integration of biochemistry, your physiology, your bone marrow issues, obviously a lot of pathologies here. 17:30 All dealing with what kind of anemia? Microcytic. 17:33 Which one are we referring to here specifically? The sideroblastic anemia’s an umbrella of etiologies. 17:40 And then just to make sure we’re clear, take a look at globin in the thalassemias.
About the Lecture
The lecture Sideroblastic Anemia: Nucleated Red Blood Cells in Bone Marrow by Carlo Raj, MD is from the course Microcytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following is the main rate-limiting enzyme in the heme synthesis pathway?
- Aminolevulinate synthase
- Delta-aminolevulinic acid dehydratase
- Ferrochelatase
- Uroporphyrinogen decarboxylase
- Porphobilinogen deaminase
Which of the following vitamins is a co-factor in the formation of δ-amino levulinic acid, a rate-limiting step in heme biosynthesis?
- Pyridoxine
- Riboflavin
- Thiamine
- Niacin
- Cobalamine
Which of the following is one mechanism by which isoniazid causes sideroblastic anemia?
- Functional pyridoxine deficiency
- Directly inhibiting ferrochelatase
- Depleting uroporphyrinogen decarboxylase
- Inhibition of aminolevulinic dehydratase
- Depleting cofactor for porphobilinogen deaminase
What is the most common genetic deficiency resulting in sideroblastic anemia?
- Germline mutation in aminolevulinic acid synthase gene
- Germline mutation in ferrochelatase gene
- Germline mutation in uroporphyrinogen decarboxylase gene
- Germline mutation in porphobilinogen deaminase gene
- Germline mutation in aminolevulinic acid dehydratase gene
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Huge thank you, dr. Raj! You managed to explain everything very clearly and with a bit of humour that allowed me to go through this 18 minutes lesson very very easy!!!
Wonderfull lesson from humourous and extremely intelligent doc . Pleased to learn from him
Nice lecture . Saves time for sleepless nights. Highly recommended for med students
Dr Raj you crack me up, you make medicine fun.