Playlist
Show Playlist
Hide Playlist
Sialoadenitis
-
Slides GIP Sialoadenitis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
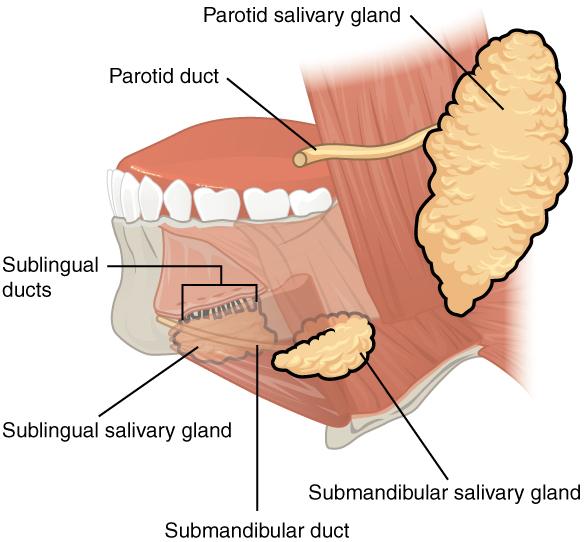
00:01 This leads us into Sialoadenitis. 00:04 So sialo, salivary gland, adenitis means inflammation of that salivary gland. 00:10 It's going to be often associated with stones but not always. 00:13 So Sialoadenitis is inflammation or infection of a salivary gland. 00:18 What's the epidemiology of this? Well, it's hard to know because the exact incidence is unknown. 00:26 In many cases, it kind of, you have a little bit of pain, discomfort, and then, it goes away. 00:32 So we don't really have a true knowledge about what the incidence is. 00:38 There doesn't appear however to be any particular predilection for ethnicity or gender. 00:43 I will say that it tends to occur in older, chronically ill, and debilitated or dehydrated patients. 00:51 The risk factors that we do recognize, so geriatric individuals, people who are older than 50 years, so, me. 00:57 They may not have normal salivary gland or saliva production, so called xerostomia. 01:05 They may be dehydrated, so they're not producing more saliva because they are dry. 01:12 That will go along clearly with anorexia or bulimia. 01:16 Sjogren Syndrome because it is associated with inflammation of the salivary gland. 01:23 And/or duct is a common precursor risk factor for developing Sialoadenitis. 01:29 And clearly, last but not least, if you have a stone that sits within the draining duct, Sialolithiasis that puts you at risk for developing inflammation more upstream in the salivary gland. 01:42 The pathophysiology of this is not that hard to think about. 01:46 So you can have primary inflammation due to an infection. 01:49 So viruses such as mumps or Epstein Barr virus or parainfluenza, frequently cause inflammation of the salivary glands. 01:58 You can have an autoimmune Sialoadenitis. 02:02 And it will typically be one of the manifestations of Sjogren's disease. 02:06 Other infections include staphylococcus aureus and strep viridans, oral flora, and radiation treatment, clearly, by causing inflammation and/or stenosis of the salivary ducts. 02:19 We're looking here at our three main salivary glands, the parotid, the sublingual, the submandibular for reasons that I don't completely understand, the vast majority of the Sialoadenitis is actually going to occur in the parotid gland up here at the angle of the jaw. 02:38 And we're showing here a stone that's in the primary duct that causes then obstruction. 02:45 And there may be bacteria behind that because, again, there's bacteria throughout the salivary gland and/or salivary duct. 02:53 And if you are not moving fluid through that, they may grow and then, a combination of the obstruction And the infection leads to an inflamed parotid gland in this case. 03:06 The clinical presentation, it's usually unilateral with salivary gland swelling on that side. 03:13 So you see this poor kid who has a really severe parotid gland Sialoadenitis. 03:19 The pain and swelling typically is worse with meals. 03:22 Again, when you eat or drink and you are trying to make saliva and it can't get out of the salivary gland, that's going to increase the pain and swelling. 03:33 Usually, it's very red, firm, and diffusely tender, all the cardinal features of inflammation. 03:39 If there is necrosis or a lot of bacterial infection, we will get purulent exudate will actually form an abscess. 03:48 And with systemic manifestations of a bacterial - a secondary bacterial infection, you'll get fevers and chills or rigors. 03:56 How do we diagnose this? Well, it's mainly clinical. 03:59 You have swelling, you've got pain, and it's unilateral and it seems to be involving a gland. 04:04 That's not that hard to make that diagnosis. 04:07 But we do want to specifically identify what are the bugs that are in there. 04:11 So you want to do a gram staining culture of any exudate that's coming from the gland if that's possible. 04:16 You may also want to evaluate for mumps or other viral causes of this. 04:23 So you can do PCR serology. Mumps is going to be the most common but there are others that will be associated with it. 04:30 When it is important to kind of sort this out from, say, a tumor of the salivary gland, then you may need to do some imaging. CT, ultrasonography, magnetic residence imaging. 04:43 You'll want to visualize whether or not there are stones in the duct because you can treat a Sialoadenitis but if you don't get rid of the obstruction, it's going to come back. 04:51 And if there's an abscess, we're going to have to identify that and drain it. 04:55 Okay. So what are we going to do about this? Most of this is going to be treating the symptoms. 05:01 But we can do some more definitive things to make sure it doesn't come back. 05:05 So we'll use compresses and heat. 05:08 Basically, applying heat will cause dilation of the salivary duct and improved flow. 05:14 And if there's an obstruction, you may resolve that. 05:17 If there's secondary infection, possibility of infection, antibiotics are due - usually indicated. 05:23 We'll want to treat the pain obviously, but we want to give anti-inflammatories to reduce swelling. 05:28 And that will also open up the duct. 05:31 And then, we can also use Sialogogues, things that will increase salivation. 05:36 So if you're a dog, we'll ring a bell. No, we won't do that. 05:39 But we can get things like peppermint oil which will increase salivation, to Sialogogues. 05:44 And with that, we have concluded our discussion of Sialolithiasis and Sialoadenitis.
About the Lecture
The lecture Sialoadenitis by Richard Mitchell, MD, PhD is from the course Disorders of the Oral Cavity and Salivary Glands.
Included Quiz Questions
What is NOT a common cause of salivary gland inflammation?
- Orthopedic surgery
- Viral infection
- Autoimmune condition
- Bacterial infection
- Radiation treatment
Why is heat a recommended treatment for sialadenitis?
- Dilation and improved flow within the duct
- Increased mucus production
- Decreased thickness of secretions
- Decreased pain
- Increased ability to eat meals to meet nutritional requirements
Which of the following is a sialagogue?
- Peppermint oil
- Garlic
- Cumin
- St John's wort
- Vitamin C
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |