Playlist
Show Playlist
Hide Playlist
Scleroderma
-
Slides GD Esophagus.pdf
-
Download Lecture Overview
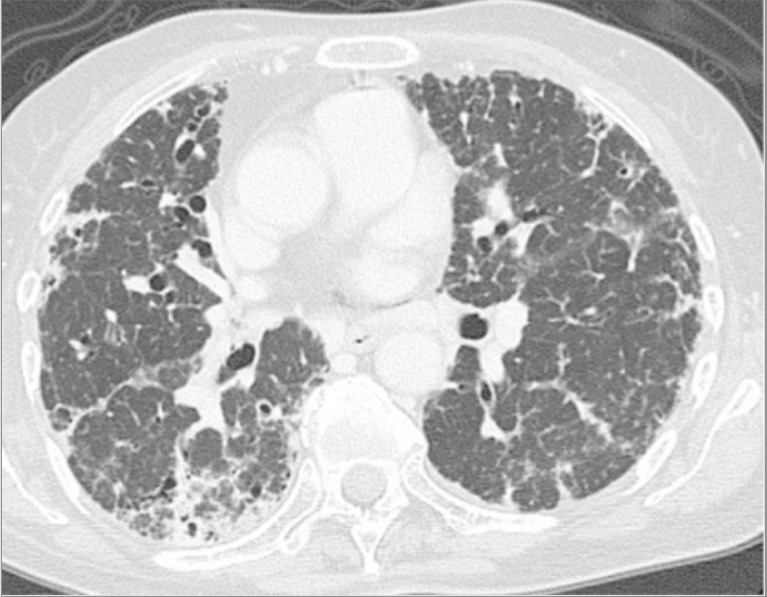
00:01 Scleroderma is the next topic. Scleroderma in general, here because you have the viscera being involved. 00:10 That we have to refer to what's known as diffuse or systemic type of scleroderma versus your limited. 00:18 The limited type would be cutaneous. The limited would be one in which you would then find skin involvement. 00:25 The limited type would be skin without any viscera involvement. The skin type of scleroderma is involved with CREST. That's a different topic with calcinosis, Raynaud's, esophageal dysmotility, sclerodactylyl, and telangiectasia. Here with scleroderma if you're thinking about viscera involvement, not only should you be thinking about the esophagus, more importantly you're thinking about the diaphragm and also the kidney. Cause here, the patient may actually die of renal failure or maybe perhaps respiratory failure. But understand here that there will be diffuse fibrosis leads to loss of lower esophageal sphincter function. There is complete absence of peristalsis, esophagel dysmotility. 01:11 The symptoms of GERD and dysphagia are very much present. It is associated with Raynaud's. 01:18 Manometry shows incompetent lower esophageal sphincter, absent peristalsis because of well, the esophagus has now become a lead pipe. That should not be the case and it is hard as a pipe. Therapy PPI, anti-reflux measure. Obviously here you're thinking about an autoimmune disease. And with scleroderma here if it's a difuse and visceral involvement, if you remember correctly, here the marker that you're going to be looking for is SCL 70. Scleroderma 70 and topoisomerase.
About the Lecture
The lecture Scleroderma by Carlo Raj, MD is from the course Esophageal Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
A 30-year-old woman comes to the physician's office complaining of heartburn and difficulty in swallowing for the past 2 weeks. She has been a smoker for the past several years and does not drink. On further questioning, she states that she has been experiencing pain in her fingers whenever she goes outside in the cold. What would manometry of the esophagus MOST likely show?
- Incompetent lower esophageal sphincter and absent peristalsis
- Increased lower esophageal sphincter pressure
- Diffuse spasm of the esophagus
- Decreased lower esophageal sphincter pressure only
- A normal resting pressure of the lower esophageal sphincter
What are the autoimmune markers used to identify diffuse scleroderma?
- Scl-70 and anti-topoisomerase
- ESR and C-reactive protein
- Antinuclear antibody
- Anti-SS-B
- CD19 and CD20
A 55-year-old man comes to the clinic with complaints of severe heartburn and difficulty swallowing for the past 6 months. He has been a regular smoker for the past 20 years and smokes 2 packs of cigarettes per day. What is the MOST appropriate treatment?
- Omeprazole and smoking cessation
- Cimetidine and omeprazole
- Nonsteroidal anti-inflammatory drugs
- Omeprazole only
- Antacids
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
A rare topic presented very well. It is very accurate to understend for any one