Playlist
Show Playlist
Hide Playlist
Renin-Angiotensin-Aldosterone-System
-
Slides RenalBloodFlow2 RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
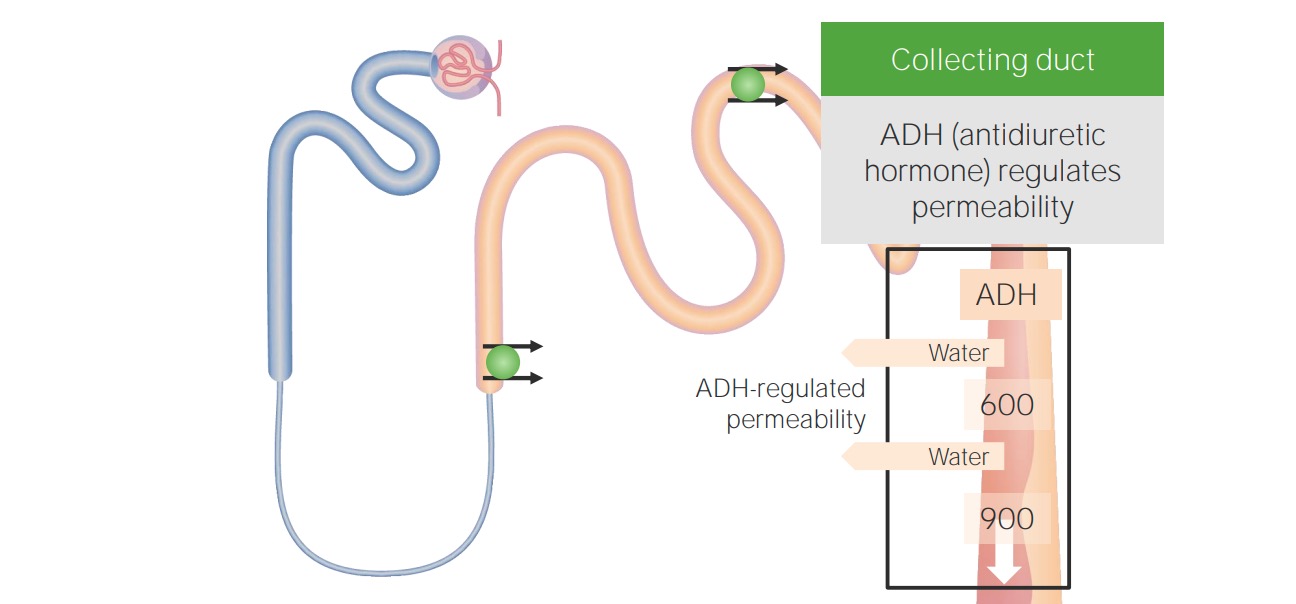
00:00 We are going to put all this together now with RAAS and make sure that you are truly familiar with the entire process of your RAAS system. Lets begin. So here we are. I want you to begin at the kidney. Please begin at the kidney and why would you want to release the renin? Decreased perfusion to the kidney.Okay good. Give me some differentials. I've walked you through renal artery stenosis adequately. What about congestive heart failure? Decreased perfusion to the kidney. In these cases, those juxtaglomerular cells are going to release renin. Hence, take a look, please. Decreased blood pressure is then going to release your renin. Here continue forward. I want you to make sure you clear by this. You are going to be an MD. You are going to be a doctor, but that MD stands for macula densa. Macula densa will decrease blood pressure. Walk me through this. Initially decrease of blood pressure, decreased perfusion, decreased GFR, where is our macula densa? Distal convoluted tubule. What is the name of that sensor? Macula densa. I showed you a picture earlier. What is that macula densa sense? It senses the sodium or chloride right. So therefore now with decreased blood pressure, what is it doing? It's not sensing as much. So all of this is going to help contribute to increasing renin. One last thing, when we have a decrease in blood pressure, can I ask you what branch of the autonomic nervous has to come out? Good. Sympathetic. What kind of receptor on your JGA? Good. Beta-1. Once again get another factor to help you stimulate renin. Here comes out and here is not ogen. Now I would like for you to take a look at this suffix. I would like for you to understand this concept ogen. What does that even mean? Trypsinogen, fibrinogen, angiotensinogen so on and so forth. So the term ogen means weak. Weak precursor right. Most of your proteins come from where? The liver. 02:12 What is the most abundant protein in our bodies? Albumin. Coming from where? Liver. Here is angiotensin, angiotensinogen coming from the liver. What does that renin do? Cleave off the ogen. There it goes. What do you have? angiotensin I. Where is the angiotensin I headed to? To the lung. What's there? ACE. So here, ACE, angiotensin converting enzyme, will take the I and turn into the infamous angiotensin II. Now lets plug in some pathologies. Are you ready? What if you had a patient that ends up having too much renin? Autonomously. There was no decrease in blood pressure as an in setting event. And imaging study you ended up finding a tumour. 02:59 Where? In the juxtaglomerular apparatus. Wow! And you ended up finding increased blood pressure. 03:05 So if you have increase in renin, increase in aldosterone, you have secondary hypertension. 03:10 Are we clear? What is this called? Reninoma. You understand the physio. You can easy put in the pathology and you see your patient. You can actually see your patient. Next, give me a pathology in which your ACE might be elevated. A pathology. May be something like What if I told you non-caseating granuloma, bilateral hilar lymphadenopathy in an African-American female. You will tell me? Good. Sarcoidosis. And sarcoidosis you could have increased production of ACE. What does this mean? Increased production of angiotensin II Now with all that said lets say that you give an ACE inhbitor. When you have an ACE inhibitor, then you knock it out and you can never form angiotensin II and never release your aldosterone. Stop there for one second. 03:56 The branch that is important for us, bradykinin. ACE, angiotensin converting enzyme is an enzyme that you must know as being the enzyme responsible for metabolism of bradykinin. Two major effects of bradykinin that you would want to know as being a side effect of what drug? ACE inhibitor. 04:18 A dry cough, And number 2, angioedema. So bradykinin, increased capillary permeability. And number 2, Might be something like dry cough. And with that dry cough, which is incredibly irritating you change the drug into ARBs. Got it? Lets move on. Angiotensin II vasoconstriction preferentially what part of the arteriole? Efferent. What would it do to your blood vessels in general? It will cause contraction, vasoconstriction. What are you are trying to do? Increased blood pressure. What was in setting event. Take a look, please. The first box, over onto your left is decreased blood pressure. You're trying to increase your blood pressure. There is my efferent arteriole. What does it do? Do not memorize this. Close your eyes. Let me ask you a question. Number one. You have efferent arteriole vasoconstriction. Tell me about renal blood flow when the plasma flow, decreased. Next efferent arteriole vasoconstriction. 05:21 Tell me about GFR, Increased. Tell me the equation for filtration fraction. GFR/renal plasma flow. 05:28 Good. You do the math. What do you get for filtration fraction? Increased. Good move on. 05:36 What else happens? While angiotensin II is going to go where, that's the organ, adrenal. 05:41 Which part? Cortex. What part of the cortex? and I am going to keep pushing you here. What part of the cortex? Glomerulosa. Angiotensin II is going to work on the glomerulosa to stimulate what's known as aldosterone synthase. Here comes an aldosterone. Close your eyes. You know this from physio already. Aldosterone turns to your collecting duct. Aldosterone works on your principal cells principally. What does it do? It works on your sodium channels everywhere. What do you mean everywhere? Well, principal cell. You picturing that? Where am I? Collecting duct okay fine and it is facing whom? Urine. It is facing the urine. So that is known as the apical membrane. That apical membrane has a sodium channel. Aldosterone could work on that ENAC. 06:32 It is called Epithelial Sodium Channel. E, epithelium; sodium channel, ENAC. Aldosterone works there to remove the sodium from the urine. You know that already. Next, on the basolateral membrane only, you have your sodium- potassium ATPase pump. So what kind of effect does aldosterone have on your pump Tell me about that pump. Sodium being kicked out. Kicked out into where? Into your blood. Aldosterone will stimulate that pump. We have addressed this. Insertion in principal cells enhances stop there. So you are going to reabsorb sodium. You are going to take out two. What do you mean take out? You are going to literally remove and secrete two substances into urine. First will be potassium, next will be hydrogen. Okay. You can see. We are going to work through a lot of pathologies here, aren’t we? Because you can have issues when you have too much aldosterone, and you can have issues in which you have two little aldosterone. Too much aldosterone. Give me two differentials.Number 1 Conn exclusive aldosterone secreting tumour. 07:45 Cushing will be both cortisole and aldosterone. Give me one aldosterone deficiency pathology, Addison. Addison's disease. So are these things that we talked about? Of course keep repeating. 08:00 So when we have aldosterone it will reabsorb sodium. It will kick out the potassium meaning to say urinated out and it gets rid of your hydrogen. So in Conn's syndrome tell me about the pH in that patient with Conn? Take your time. Close your eyes. Reabsorbing too much sodium. 08:17 Getting rid of too much hydrogen. What happens to your pH? Increases alkalosis in Conn. Confirm it. Why? Because you will find many patients with secondary hypertension and Conn syndrome. 08:28 Many, not rare. Many. 08:32 Great favourable sodium gradient and along with sodium what comes out? Fluid. Tell me what is it that contributes to the pitting edema and congestive heart failure? The aldosterone. 08:44 Why? Because of this entire mechanism, we just went through. Are we done? Not quite yet because a decrease in blood pressure, but there is another hormone that also comes into play, and angiotensin II not only will it be responsible for releasing that aldosterone from adrenal cortex, but angiotensin II also works on the posterior pituitary. Why, why, why, why? Decreased blood pressure is what the kidney is thinking? This angiotensin II is then going to walk on the posterior pituitary and so, therefore, you are going to release ADH. Tell me about ADH, antidiuretic hormone. That works on the, also collecting duct. What does it do? It works through your V2 receptors. How many kidneys do you have? I think one. 09:28 No no. Who? I think I have two. You have two kidneys. So V2 receptors is what ADH works on. Gotta have fun with this just a little bit huh. So works on V2 receptors and what does it do? It is then going to insert aquaporins. So that you do only what please, antidiuretic hormone. What is another name for ADH? Vasopressin and you are only going to reabsorb water, water, water in the hopes of doing what? In the hopes of restoring osmolarity. In the hopes of restoring some of your blood pressure. Now couple of important things about angiotensin II in addition, is that it does work. Please pay attention. That's its proximal convoluted tubule. Angiotensin II earlier through aldosterone. May I ask you questions? Worked where? Collecting duct. Angiotensin II here is working on proximal tubule. What does it do? It reabsorbs your sodium. Don't memorize this. What are we doing? There was a decrease in blood pressure as being the inciting event right. Now the angiotensin II is going to work on your proximal convoluted tubule so you can try to remove more sodium in exchange for hydrogen. So water reabsorption and then can permit what is known as contraction alkalosis and what that basically means is that you are going to have contraction and along with it you have also hydrogen leaving resulting in alkalosis. 10:58 Finally, in the hypothalamus, it has thirst. Now all of this is then going to contribute to release of ADH. So ladies and gentleman angiotensin II as you can see here from the origin of it all with that initial event of whatever it may be is causing decreased perfusion to the kidney. Once it gets into the renin realm, now renin along with angiotensin II and aldosterone my goodness gracious right up and down the body has all kinds of incredible effects, and all these pathologies that we're going to put in here including some of our issues with ADH and diabetes insipidus right. Central nephrogenic, we are going to bring all this into play, but if your foundation isn't strong it is going to make it quite difficult for me and you to work together so that we can accomplish our goals effectively.
About the Lecture
The lecture Renin-Angiotensin-Aldosterone-System by Carlo Raj, MD is from the course Renal Diagnostics.
Included Quiz Questions
Which of the following statements is true regarding the physiological changes occurring in the renin-angiotensin-aldosterone system?
- Decreased blood pressure is sensed by the juxtaglomerular cells.
- Decreased blood pressure is sensed by the macula densa cells.
- Decreased sodium sensed by the macula densa cells inhibits renin secretion.
- Increased blood pressure is sensed by the juxtaglomerular cells.
- Parasympathetic system is activated.
Which of the following receptors is found on the juxtaglomerular cells?
- Beta-1 adrenergic receptor
- Beta-2 adrenergic receptor
- Beta-3 adrenergic receptor
- Nicotinic acetylcholine receptor
- Muscarinic acetylcholine receptor
Which of the following is not an effect of angiotensin II?
- Vasodilation of the efferent arteriole.
- Acts on the AT II receptors on the vascular smooth muscle.
- Vasoconstriction of the efferent arteriole.
- Increases the glomerular filtration rate.
- Decreases the renal plasma flow.
Which of the following statements is incorrect regarding the effects of aldosterone?
- Na+/K+ pump insertion in the intercalated cell.
- Na+/K+ pump insertion in the principal cell.
- Excretion of K+ and H+ from the blood.
- Upregulation of K+ channels in the principal cell.
- Upregulation of H+ channels in the intercalated cell.
Which of the following conditions is associated with an increase in the activity of the angiotensin converting enzyme?
- Sarcoidosis
- Addison’s disease
- Conn's syndrome
- Cushing's disease
- Cushing's syndrome
Which of the following is not an effect of aldosterone?
- Increase in Kalium reabsorption
- Upregulation of ENaC
- Increase in sodium absorption
- Stimulation of Na+/K+ pump on the basolateral membrane
- Stimulation of H+ ion secretion in the collecting duct
Customer reviews
4,3 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
Love how he can make something difficult into an easy learning experience. Excellent clases, with funny quotes that make you smile.
Amazing! I really get the material, Dr. Raj! I love how you keep reinforcing the material during each lecture!
i like his fun attitude to teaching. It works for me!
It would be nice if the material was presented in a less intense manner. It feels more like he is prepping football players for a big game. It is very distracting. Perhaps, if the lecture didn't feel so choppy it would be more enjoyable.