Playlist
Show Playlist
Hide Playlist
Renal Corpuscle – Juxta-glomerular Apparatus
-
Slides RenalBloodFlow1 RenalPathology.pdf
-
Download Lecture Overview
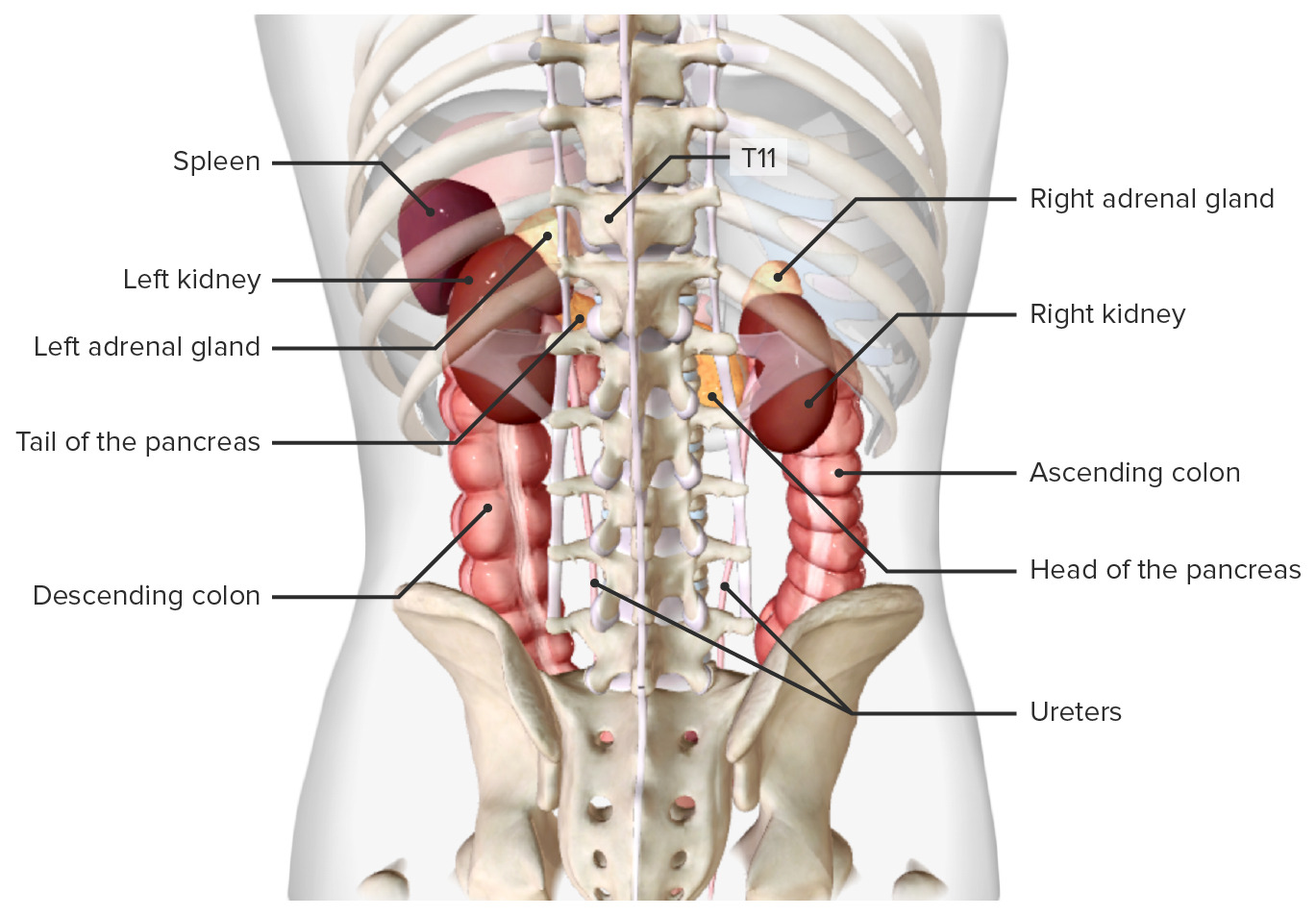
00:00 Here, let me set this up for you. 00:03 So we have the afferent arteriole, I’d like for you to begin up there, afferent arteriole. 00:07 How did you give rise to this? It was a renal artery. 00:10 And it came in, and what did it do? Interlobar. 00:12 What was next? Interlobular. What’s the name? Well, you have your arcuate. 00:15 And you had your Interlobular, what was another name for that? Cortical radiate. 00:18 And you have the afferent arteriole, and here we are. 00:22 I want you to come towards the glomerulus. 00:26 You’re going to form a tuft of capillaries, I’ve mentioned that before. 00:31 The afferent arteriole is coming in and you see all those structures there? That’s a lot of structures. 00:36 Let me set each one up. 00:38 What's inside my afferent arteriole? I’m sorry, what? I didn't hear you, one more time. 00:43 Good. 00:43 Plasma, excellent. 00:45 So your plasma coming through there, good. 00:47 Can you hear me? Loud and clear. 00:49 Afferent arteriole, plasma, filtering through. 00:52 Tell me about hydrostatic pressure from physio. 00:54 Increased. 00:55 It ensures filtration, right? ensures filtration. 00:59 Through what? Through the endothelial cells across the basement membrane, into where? Into the Bowman's space. 01:07 Okay. 01:08 So now, tell me about the cells that we see in green. 01:12 They're called juxtaglomerular cells. 01:14 What are they responsible for? They're responsible for measuring the pressure within the afferent arteriole, aren't they? Mm-hmm. 01:20 So let's say that you have decreased perfusion to the kidney, how did that occur? You tell me what the diagnosis is in older patient, male, approximately 52 years of age, blood pressure: 160 over 90, three different times on three different clinical visits. 01:37 So far, diagnosis? Hypertension. 01:39 We're not done. 01:41 Now, you go ahead and check the kidney, or excuse me, you auscultate the renal area, and you hear noise, bruit, your renal bruit. 01:56 Give me diagnosis. 01:58 What's causing the hypertension? What’s causing the bruit? A 52-year-old male, the bruit is caused by atherosclerosis. 02:07 Where? Renal artery. 02:09 Good? What caused the 160 over 90? Secondary hypertension, why? Ah, this will explain everything. 02:17 The renal artery has been cut off, take a look at the previous slide if you need to. 02:21 so that you see the positioning of the afferent versus renal artery, right? Now, you have decreased perfusion through the afferent. 02:29 This is not good. 02:31 You have decreased perfusion, that kidney must maintain GFR at all times. 02:36 Tell me what the juxtaglomerular cells are going to release here due to renal artery stenosis, secondary to atherosclerosis. 02:46 Renin. Good. 02:47 What’s the name of that receptor that those JG cells have, JG, juxtaglomerular? beta-1 What are they going to release? Renin. Good. 02:57 Continue the story. 02:58 Renin, angiotensin II, aldosterone. 03:02 What’s my blood pressure in my 52-year-old male? 160 over 90. 03:06 Was this primary or secondary hypertension? Secondary hypertension, huh? Secondary hypertension. 03:12 You got this? You better. 03:14 You have no choice, you have to know this. 03:16 Next, what's on the other side? Well, the afferent arteriole with the JG cells are going to communicate with a distal tubule. 03:25 What’s in there, what’s in the distal tubule? You wish it was me being flushed down the toilet. 03:32 It’s not, it’s urine. 03:34 That’s urine in the distal tubule, you see it? Okay, good. 03:38 So that’s urine in the distal tubule. 03:41 And what sensing the urine? It’s not the juxtaglomerular cells, it’s the macula densa, are we clear? So in physio, you did a little bit of a reflex between the macula densa and the juxtaglomerular cells. 03:54 Yeah, you did. 03:55 And that was called the tubuloglomerular feedback. 03:57 We’ll get to it in due time, not yet. 03:59 And the macula densa is sensing what? The sodium and chloride within the urine. 04:04 Are you putting all of these together? I hope so, I just gave you one example. 04:08 Now as we move, progress through here in this lecture series, we’re going to go ahead and talk about the efferent arteriole in great detail. 04:14 We’ll talk about the afferent arteriole in great detail. 04:16 We’ll bring all these structures together. 04:18 And we’re going to put in more and more and more pathologies. 04:21 It’ll be fun, trust me. 04:22 All we’re doing is laying down foundation. 04:24 Are you having a good time? Smile for me. 04:26 Okay, let's discuss this graph for a moment. 04:29 On the x-axis, we see that there's a mean arterial pressure and on the y-axis, we see that we have renal blood flow compared to percentage of normal. 04:37 This graph illustrates a phenomenon we've already mentioned occuring in the brain and that's 'autoregulation'. 04:42 In essence, this describes the organ's ability to regulate its perfusion over a range of blood pressures. 04:48 So if the chemoreceptors and baroreceptors detect hypoxia or changes in blood pressure, the system can constrict or dilate to maintain the necessary blood flow relatively constantly. 04:59 If you look at the y curve here on the graph, the green line, what do you see from point A to point B? Is there any change of blood flow to the kidney? No, and this is important because we're talking about a constant blood flow to an organ over a range of about 100 mmHg in blood pressure How did that occur? Autoregulation. 05:19 So what does that mean to? There was no communication with the brain. 05:23 There was a reflex in which it was able to handle the pressure at the level of the kidney just like that, like a reflex. 05:31 So now, this is autoregulation. 05:33 You pay attention. 05:34 As the pressure starts dropping, from 90, point C is normal Point C as in Charlie is 90. 05:41 Let’s call that normal. 05:43 As your pressure starts dropping all the way down to 40, what do you expect your blood vessels to do so that you maintain proper flow? A represents vasodilation. 05:53 Part of autoregulation so that the flow doesn’t diminish. 05:57 The pressure starts decreasing, but autoregulation causes vasodilation - that’s point A. 06:04 Whereas if you have point B, now what does that mean to you? Your pressure is increased. 06:08 Autoregulation tells your blood vessels to do what? Vasoconstrict, we have B. 06:13 We pretty much identified the perfect autoregulation points on this line for horizontal. 06:20 That is as far as I’m going to go with you on this. 06:22 I need you to at least understand autoregulation and its specifics. 06:27 At any point in time, any one of your licensed exam could ask you about curve X in which there is absent, no autoregulation. 06:35 And that dashed line represents mild autoregulation, I’ll go as far as that. 06:39 But your focus right now in pathology is going to be between A and B, that green line exhibiting perfect, perfect autoregulation. 06:47 Let’s move on.
About the Lecture
The lecture Renal Corpuscle – Juxta-glomerular Apparatus by Carlo Raj, MD is from the course Renal Diagnostics.
Included Quiz Questions
Which of the following substances is released in response to hypoperfusion by the juxtaglomerular cells?
- Renin
- Aldosterone
- Angiotensin-converting enzyme
- Angiotensinogen
- Angiotensin
Which part of the glomerulus is responsible for measuring the pressure in the afferent arteriole?
- Juxtaglomerular cells
- Macula densa
- Intraglomerular mesanglial cells
- Extraglomerular mesanglial cells
- Glomerular tuft
Which of the following structures detects the concentration of sodium chloride in the distal tubule?
- Macula densa
- Extraglomerular mesanglial cells
- Intraglomerular mesanglial cells
- Glomerular tuft
- Juxtaglomerular cells
Which of the following factors in the afferent arteriole ensures high filtration in the glomerulus?
- High hydrostatic pressure
- Low hydrostatic pressure
- High oncotic pressure
- High sodium concentration
- High plasma volume
Which of the following receptors in the juxtaglomerular apparatus is involved in the release of renin?
- Beta 1 adrenergic
- Beta 2 adrenergic
- Beta 3 adrenergic
- Alpha 1 adrenergic
- Alpha 2 adrenergic
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text