Playlist
Show Playlist
Hide Playlist
Regulation of GFR and RBF
-
Slides 02 GFR UrinarySystem.pdf
-
Download Lecture Overview
00:00 So, glomerular filtration rate and renal blood flow inherently have a link to them. They are not the same parameter though. What you can think about is that glomerular filtration rate is going to be fairly constant across most renal blood flows. The renal blood flow is only constant across an autoregulatory range. If you have too high of pressures or too low of pressures, you're not going to have the same amount of renal tubule blood flow. If pressure is high above the autoregulatory range, you're going to have an increase in renal blood flow. 00:43 If pressure is below the autoregulatory range, you're going to have a decrease in renal blood flow. Now what causes this autoregulatory range to have a fairly consistent blood flow across a wide range of mean arterial pressures? That can be seen in this graft that you see where you have mean arterial pressure on the X axis or blood flow on the Y axis. There is a range at which there is autoregulation and that means that through this zone you're going to have a fairly constant flow despite the changes in mean arterial blood pressure. What causes that? It's primarily due to a myogenic response. And what is a myogenic response? That is an inherent local reflex. "If you have too much pressure inside a vessel, it may cause it to constrict. If there's not enough pressure inside the vessel, it will cause it to dilate on its own." So those 2 local effects allow for you to maintain renal blood flow across a fairly long mean arterial pressure zone. Glomerular tubular feedback is also a very important aspect when trying to determine what renal blood flow is. It doesn't fit quite as well on this particular graft so we're going to use renal tubule feedback in more of a diagram form. So as we look for glomerular tubular feedback, let's talk through the 2 different examples that we have. 02:16 One is an increase in tubule flow. The second will be a decrease in tubule flow. So what affects tubule flow and how do you get that to change renal blood flow? The first thing to think about is what is renal tubule flow being sensed? Well at this point, you can't really stick a flow meter in your kidney and determine how fast the fluid is traveling through it. So, what the body does instead is sent the amount of sodium chloride in bulk form that's transported across the renal tubule. If there is high amount of sodium and chloride that is traveling past the macula densa, which is in the distal convoluted tubule right next to the juxtaglomerular cells. There is a little signal that is sensed that decreases the amount of renin release. 03:16 If you have a decrease in the amount of renin release, the net result is no angiotensin II and no aldosterone formed. There is a signal of adenosine that is released in response to having a high sodium chloride sensed by the macula densa. What that increase in adenosine does is cause the afferent arteriole to constrict and the efferent arteriole to dilate and the net result is a decrease in the pressure of the ultrafiltrate, a decrease in glomerular filtration rate, and that causes tubule flow to decrease. The other example is if tubule flow decreases too much, how do you get to regulate that through glomerular tubular feedback? And you're going to do the same thing, you're going to sense the bulk flow of sodium chloride by the macula densa. This case though, if you have low sodium chloride you're going to get a block of adenosine. You will, however, increase more renin and as you increase more renin from these juxtaglomerular cells what this does is increases angiotensin I, angiotensin II. 04:35 Angiotensin II in this case is an active substance and angiotensin II causes the efferent arteriole to constrict. So remember if you constrict the efferent arteriole, you're going to get a back-up of pressure in the glomerular capillary. This increases the pressure of ultrafiltration. 04:58 It increases the glomerular filtration rate. If you increase glomerular filtration rate, then that result is tubular flow will increase. So looking at glomerular tubular feedback also gives us insight into how it might change glomerular filtration rate and then even renal blood flow. 05:24 Now if we return to this kind of diagram of trying to look at glomerular filtration rate, they're on the bottom and then renal blood flow with its autoregulatory zone. What other molecules affect renal blood flow? Nitric oxide and prostaglandin especially prostaglandin E2 cause dilation of blood vessels and therefore more renal blood flow. The endotheliums and leukotrienes cause a constriction. Both the nitric oxide and prostaglandins will cause vasodilation of the various arterioles. To look at this in more detail, let's take our example of our nephron here. This is the afferent and efferent arterioles. So let's review dilation of first the afferent arteriole. If you vasodilate this arteriole, you get an increase in ultrafiltration perfusion pressure, increases in the partial pressure within the glomerular capillary, this increases GFR and increases tubular flow. The downside of this part here is there's also an increase in renal blood flow associated with the afferent arteriole. If you remember, if you dilate the efferent arteriole the opposite effects happen where you have decreases in GFR and decreases in flow, but this also increases renal blood flow. If we combine these effects dilating both the afferent arteriole and the efferent arteriole will look something like this. Now what happens to the overall glomerular filtration rate? It really doesn't change very much if it's only stimulated a little bit. If you get a little bit of vasodilation of the afferent and efferent, these can balance each other out and therefore there is no change in glomerular filtration rate but there is a large increase in renal blood flow. In terms of the endocrine substances, we've already talked about angiotensin II. We talked about angiotensin II with the glomerular tubular feedback. If you have an increase in ang II, you get a decrease in renal blood flow; atrial natriuretic peptide or ANP causes an increase in renal blood flow; epinephrine, which is also you can think of that as a sympathetic nervous system response of release from the adrenal medulla that causes a vasoconstriction which would decrease renal blood flow. And finally we have neuro factors and these neuro factors primarily utilize norepinephrine as the neurotransmitter of choice and those also have a decrease on renal blood flow. Now when you get multiple constrictors that can affect both the afferent and efferent arterioles, we need to combine the effects on glomerular filtration rate and renal blood flow. So let's review again an afferent arteriole. Vasoconstriction here decreases the partial pressure of the ultrafiltrate, decreases the pressure of the glomerular capillary hydrostatic fluid, decreasing GFR, and decreasing the renal tubule flow. This will also decrease renal blood flow. If we look at the time where you get an efferent arteriole vasoconstriction, the opposite effects happen on glomerular filtration rate and the ultrafiltration pressures. 09:10 Both of them increase. This will increase renal tubule flow. Again though, if you have an afferent arteriole vasoconstriction, you decrease renal blood flow. You add these 2 together and you get a less of a change on glomerular filtration if they occur in a minor vasoconstriction on both sides. This though, however, will still decrease renal blood flow. If, however, you get a pronounced vasoconstriction, you could start to affect GFR, decreasing it and have even larger decreases in renal blood flow.
About the Lecture
The lecture Regulation of GFR and RBF by Thad Wilson, PhD is from the course Urinary Tract Physiology.
Included Quiz Questions
Which of the following substances increases renal blood flow?
- Atrial natriuretic peptide
- Epinephrine
- Norepinephrine
- Angiotensin II
How will glomerular filtration rate be affected if the efferent arteriole undergoes vasodilation?
- It will decrease.
- It will increase.
- It will stay the same.
- It will increase and later decrease.
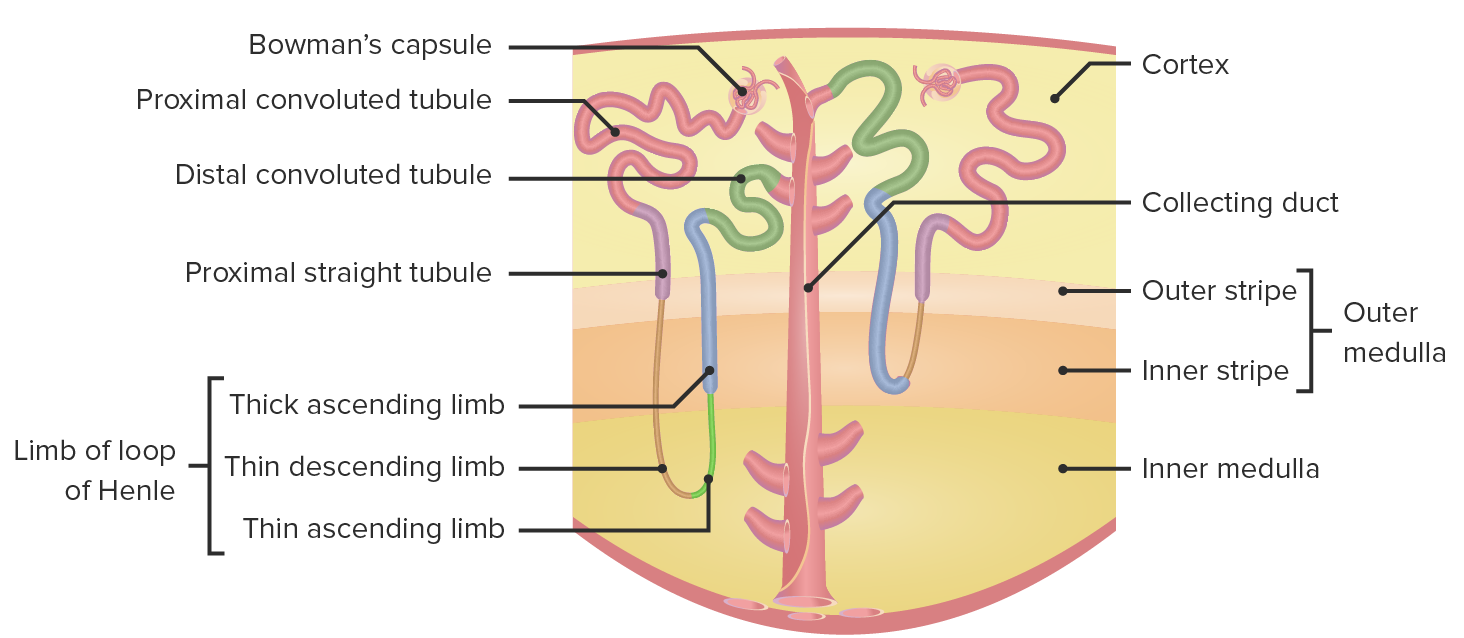
Which of the following best describes the location of the macula densa?
- Distal convoluted tubule, next to the juxtaglomerular cells
- Proximal convoluted tubule, next to the juxtaglomerular cells
- Thin descending limb
- Collecting ducts, next to the juxtamedullary cells
- Thin ascending limb
Which of the following best describes the relationship between flow rate and mean arterial blood pressure within the autoregulatory zone?
- Constant flow, regardless of changes in mean arterial blood pressure
- Decreased flow, when mean arterial blood pressure decreases
- Decreased flow, when mean arterial blood pressure increases
- Increased flow, when mean arterial blood pressure increases
- Increased flow, when mean arterial blood pressure decreases
Which of the following will be released after a high concentration of NaCl is sensed by the macula densa?
- Adenosine
- Angiotensin I
- Angiotensin II
- Renin
- Aldosterone
Customer reviews
1,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
2 |
| 2 Stars |
|
0 |
| 1 Star |
|
14 |
very good explanations helped me to understand easily. Recommend watching it.
Clear and concise, concepts were explained in enough detail and slowly enough to follow.
16 customer reviews without text
16 user review without text