Playlist
Show Playlist
Hide Playlist
Rapidly Progressive Glomerulonephritis (RPGN) – Nephritic Syndrome
-
Slides Nephritic Syndrome.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
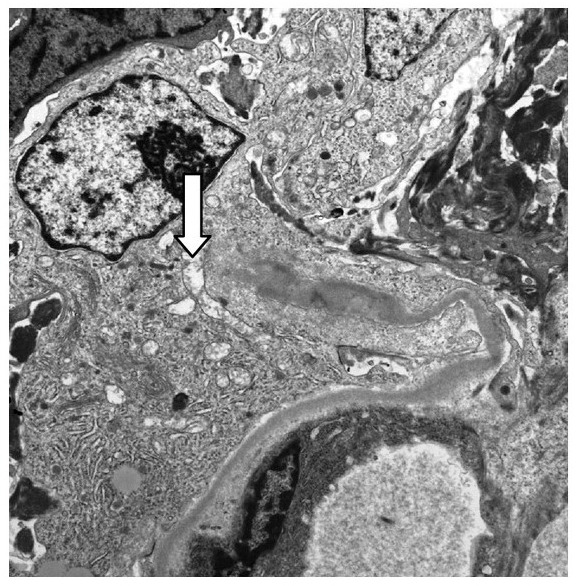
00:01 And that brings us to our rapidly progressive glomerulonephritis or RPGNs. 00:07 Remember, RPGNs are a clinical syndrome of severe acute nephritic syndrome. 00:13 These patients almost always have an active urine sediment and they have a progressive loss of renal function over days to weeks with a rapid progression to renal failure without treatment. 00:24 It can be caused by a variety of different renal diseases but what signifies this as being an RPGN is in addition to the clinical presentation of rapid progression to renal failure. 00:36 We also see morphologically on biopsy that presence of necrosis and crescents. 00:42 And that presence of necrosis and crescents are essentially a nonspecific response to severe injury to that glomerular capillary wall. 00:52 So, when we think about the categories that signify RPGN, it includes Type I anti-glomerular basement membrane disease or anti-GBM disease. 01:02 This is an acute nephritis where patients may have a pulmonary renal syndrome, meaning that both the lungs and the kidney are affected. 01:10 So, they might be presenting with hemoptysis, coughing up blood, and pulmonary hemorrhage, and when that happens in the situation both with an acute nephritis, we term that as Goodpasture's syndrome. 01:22 There's Type II RPGN which are due to immune complex-mediated diseases. 01:28 We just talked about each one of those: IgA nephropathy, post-infectious GN, lupus nephritis, and membranoproliferative GN. 01:37 All of those, if they present with a rapid deterioration in renal function and morphologically, when we biopsy those patients, if we see necrosis and crescents, they now become an RPGN. 01:48 And then Type III which is pauci-immune type, we refer to those as ANCA-associated glomerulonephritis. 01:57 These are small vessel vasculitis that target the glomerular capillaries. 02:02 So, let's talk about Type I or anti-GBM disease. 02:07 This is due to the formation of autoantibodies against Type VI collagen, the NC1 domain of the alpha-3 chain. 02:14 When we have both pulmonary and renal manifestations, we refer to that as Goodpasture's syndrome. 02:20 So, those antibodies target the GBM in both the kidney but as well -- but also the basement membrane of the pulmonary alveoli. 02:29 It can occur in all ages but our younger patients, again, less than the age of 30, are more likely to present with the full Goodpasture's syndrome. 02:38 Our older patients over the age of 50 are more likely to present with an isolated glomerulonephritis. 02:46 So, in our Type II, which are our immune complex-mediated RPGNs, it's due to the formation of those immune complexes and activation of complement as described in the disease processes that we talked about before. 02:58 But again, what happens is those patients clinically will present with a rapid deterioration of renal function and morphologically, when we biopsy them, they have necrosis and crescents, and that's why they're grouped as an RPGN. 03:11 And finally, Type III, which is our pauci-immune type, this includes our ANCA-associated antibodies. 03:20 These are also referred to as antineutrophil cytoplasmic antibodies. 03:24 The pathogenesis of ANCA-associated vasculitis or GN is complex. 03:29 It's multifactorial and involves several different etiologies that's not yet been fully elucidated. 03:35 There's no or minimal immune deposits, hence the word pauci-immune. 03:39 It may be associated with systemic disease or it could just be renal limited. 03:46 There's two types of ANCA that we need to think about. 03:49 There's c-ANCA which refers to cytoplasmic staining. 03:54 That's why I want you to notice on the immunofluorescence the cytoplasm of the neutrophilic stain which is why we call it c-ANCA. 04:01 Now, the actual target antigen that we're concerned about is called proteinase 3. 04:04 When patients have c-ANCA, it may be renal limited or associated with Wegener's granulomatosis which we now refer to as granulomatous polyangiitis or GPA and that's a crescentic glomerulonephritis, sinusitis with upper airway involvement, people will complain of otalgia as well, as well as pulmonary hemorrhage. 04:26 We also have p-ANCA referred to as perinuclear because if you look at the immunofluorescence of the neutrophil, the perinuclear area is stained. 04:35 Now, the actual target antigen that we really care about is the myeloperoxidase or anti-MPO antibody. 04:42 That is our target antigen. 04:44 It may be renal limited or again, it can be associated with microscopic polyangiitis and that's a crescented glomerulonephritis along with pulmonary hemorrhage because those alveolar cells are affected as well. 04:56 When it comes to diagnosing patients who have RPGNs, their clinical presentation is key and remember, that's going to be characterized by acute nephritis, active sediment, and rapid loss of renal function. 05:09 We can also look for positive serological tests. 05:12 So, blood test, things like anti-GBM antibodies if we're concerned about anti-GBM disease. 05:18 We also wanna look at c-ANCA and p-ANCA, and remember their target antigens. 05:23 So, we wanna look at PR3 and MPO. Up to 5-15% of people, however, who have pauci-immune GN can be ANCA negative. 05:34 So, we have to keep that in mind. 05:35 We can't clinch the diagnosis or hang our hat on a having a c-ANCA or p-ANCA. 05:41 Now, I also want to mention a special association in this patient population. 05:46 So, people who come in with ANCA-associated vasculitis, it will be critical to really take a good social history and ask them potentially about cocaine use. 05:56 So, within the last decade, there -- people have been made aware that cocaine has been adulterated with something called levamisole. 06:04 Levamisole is an old antihelminthic agent but it is that environmental trigger that can really turn on this process for ANCA-associated vasculitis. 06:14 When people have levamisole-associated ANCA vasculitis, they tend to come in not only with that syndrome of microscopic polyangiitis or granulomatosis with polyangiitis, they also will have some cutaneous lesions. 06:30 So, we can typically see them on the helix of the ear and we can also see them on the Achilles tendon as well. 06:35 So, pay attention to a good skin exam and please take a good social history. 06:40 This is critical in order to be able to catch this. 06:44 As always, with any of our glomerular disease, we wanna do a biopsy that's going to be definitive. 06:50 So, this is a biopsy of a patient who has pauci-immune glomerulonephritis and this is the light microscopy that is really highlighted with a Jones' silver stain. 07:00 So, we're looking at basement membranes and what our arrow is really pointing to is an area of necrosis. 07:06 So, you could basically see that this destructive process in the segmental portion of the glomeruli is so destructive that it basically broke through that basement membrane. 07:15 So, that's what we refer to as necrosis. 07:18 Our image on the right here is another silver Jones' silver stain for Jones' on light microscopy that actually shows a crescent. 07:27 So, if you can see those little black areas in the middle, those are the normal capillary loops. 07:32 They're being completely squished down by this process of a crescent and we call it a crescent because it almost looks like a crescent moon, but this particular crescent is taking but that entire glomerulus and it's made up of things like parietal epithelial cells, visceral epithelial cells, and macrophages, and it's essentially squishing a glomerulus. 07:52 So, in immunofluorescence for pauci-immune GN, it's exactly as we stated. 07:56 It's pauci-immune. So, we don't really see anything other than some fibrinogen. 08:01 We're not gonna see any immune complex deposition or if we do see it, it'll be very little, hence the name pauci-immune. 08:07 But for anti-GBM disease, remember where those antibodies are directed at, at that Type IV collagen. 08:13 So, we will see some of the most beautiful immunofluorescence that's out there. 08:17 You see this beautiful ribbon-like GBM IgG that's directed towards that in a linear fashion, towards that glomerular basement membrane and that's pathognomonic for anti-GBM disease. 08:29 So, in terms of treatment, one thing that I cannot underscore enough, this is a renal emergency. 08:35 This is when you have to call your nephrologist, we will come in at any time. 08:38 These are the patients that we want to diagnose and institute therapy immediately. 08:43 It is a renal emergency because the chance of recovery is going to depend on the rapid institution of therapy in this particular patient population. 08:51 We give our patients high-dose steroids. 08:53 So, IV pulse methylprednisolone typically over a 3-day period of time and we can use doses anywhere from 250-750 mg/day. 09:04 We then follow that by oral prednisone typically dosed at 1 mg/kg and then tapered over a 6-month period of time. 09:11 We can use an alkylating agent like cyclophosphamide either oral or IV, that patients will have an induction of anywhere from 3-6 months to induce a remission. 09:22 For ANCA-associated vasculitis, we now have rituximab which is non-inferior in most cases to cyclophosphamide depending on their clinical presentation. 09:32 Remember, that's that monoclonal antibody to CD 20. 09:36 Once our patients induce a remission, then we can use azathioprine which is an antimetabolite agent for maintenance therapy. 09:44 We can also maintain our patients with rituximab as well if they have that as an induction therapy. 09:50 And for anti-GBM disease, we have plasmapheresis. 09:52 Remember, these patients are making anti-GBM antibodies. 09:57 So, we can actually take those out with plasmapheresis and give them either fresh frozen plasma or albumin back. 10:04 We also, in those patients, want to be able to give them an alkylating agent like cyclophosphamide or potentially something like rituximab as well. 10:12 Now, interestingly, patients who are dialysis-dependent and they have ANCA-associated GN, those patients can also potentially benefit from plasmapheresis. 10:23 However, studies have shown that over the long term, the mortality is unchanged. 10:29 I also wanna mention that for people who have extrarenal manifestations of disease, if they have pulmonary hemorrhage in the setting of ANCA-associated vasculitis, then plasmapheresis would be indicated as well. 10:41 So, I really want to underscore, again, how important it is to make a swift diagnosis and institute treatment in this particular population because the morbidity and mortality from these disease processes are so high. 10:56 If we can expedite the diagnosis and start treatment expeditiously, we will not only be able to spare the patient from potentially needing dialysis but we can ultimately potentially save that patient's life. 11:09 And with that, we've concluded the nephritic syndrome lecture.
About the Lecture
The lecture Rapidly Progressive Glomerulonephritis (RPGN) – Nephritic Syndrome by Amy Sussman, MD is from the course Nephritic Syndrome.
Included Quiz Questions
Which of the following is true regarding anti-GBM syndrome?
- It is caused by antibodies directed against type IV collagen in the glomerular basement membrane.
- Younger patients are more likely to present with isolated glomerulonephritis.
- The clinical presentation of Goodpasture's syndrome involves the upper respiratory tract, lungs, and kidneys.
- Biopsy of the kidney typically reveals pauci-immune glomerulonephritis.
Which of the following is true regarding granulomatosis with polyangiitis?
- It is associated with autoantibodies against proteinase 3.
- It is a large-vessel vasculitis and has a preference for the aortic arch and its branches.
- It is associated with autoantibodies against p-ANCA.
- Immunofluorescence microscopy demonstrates linear deposition of IgG along the glomerular basement membrane.
- It is a common cause of immune complex-mediated RPGN.
Which of the following is categorized as a type II, rapidly progressive glomerulonephritis?
- Postinfectious glomerulonephritis
- Dense deposit disorder
- Microscopic polyangiitis
- Anti-GBM syndrome
- Minimal change disease
Which of the following is used in the maintenance phase of the management of RPGN?
- Azathioprine
- Plasmapheresis
- High-dose IV methylprednisolone
- Antibiotics
- Proteosome inhibitors
Which of the following pairings is correct?
- Microscopic polyangiitis - Anti-myeloperoxidase antibodies
- Lupus nephritis - C3 nephritic factor
- Membranoproliferative glomerulonephritis - Anti-phospholipase 2 receptor antibodies
- Membranous nephropathy - Anti–proteinase 3 antibodies
- IgA nephropathy - Anti–double-stranded DNA antibodies
Which of the following statements is true regarding rapidly progressive glomerulonephritis?
- It is characterized morphologically by necrosis and crescent formation on biopsy.
- It can be managed conservatively through a low-salt diet, loop diuretics, and ACE inhibitors/ARBs.
- It is a type of severe acute nephrotic syndrome.
- The findings on biopsy develop over a prolonged period of time.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I was struggling between Pauci and Anti Basement(Goodpasture) now my concept is very clear.
I was confused a lot of the 3 types of RPGN. Credits to Dr. Sussman the it is all now clear and very understandable.