Playlist
Show Playlist
Hide Playlist
Primary Hyperaldosteronism – Secondary Hypertension
-
Slides Secondary Hypertension.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
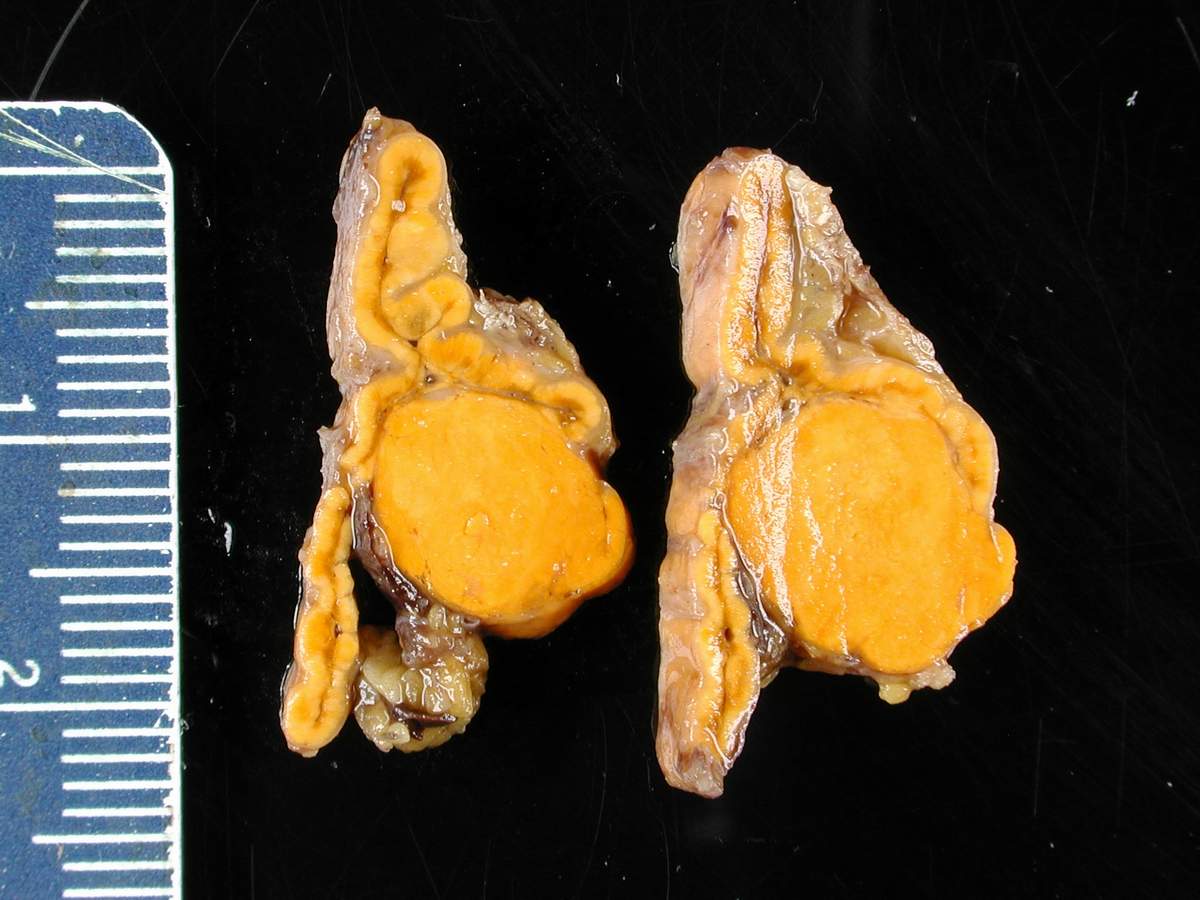
00:01 So, primary hyperaldosteronism is really autonomous production of aldosterone leading to mineralocorticoid excess. 00:08 The prevalence really depends on where you're at. 00:12 It's about 0.5-2% in most populations but if you're in a tertiary care referral center, it's gonna be a little bit higher because you are seeing more complex patients so it's more in the order of 5-12%. 00:24 Now, I want you to keep in mind, this is the most common cause of hypertension due to an endocrinopathy or endocrine-related cause. 00:32 The etiology that causes this could be due to a functional adrenal adenoma, bilateral adrenal hyperplasia, or rarely, adrenal corticocarcinoma. 00:44 The way our patients typically present when they have primary hyperaldosteronism is that they have mineralocorticoid excess. 00:53 So, they typically will have a triad of hypertension, unexplained hypokalemia, and metabolic alkalosis. 01:01 I do want you to keep in mind, not every patient is gonna follow that rule. 01:05 There may be a number of patients who come in with normal potassium levels. 01:09 So, once we suspect this, we wanna see if we can clinch a biochemical diagnosis in our patient. 01:17 So, the first thing that we wanna do is wanna obtain a plasma aldosterone concentration to plasma renin activity ratio. 01:24 This is typically taken as a morning ambulatory blood sample. 01:28 A ratio of greater to 35-50 with a plasma aldosterone concentration of greater than or equal to 15 ng/dL is suggestive of primary hyperaldosteronism. 01:40 So, for example, if I have a patient who has a plasma renin activity of 0.6 ng/mL/h and a plasma aldosterone concentration of 30 ng/dL, his ratio is 50. 01:54 So, he would meet criteria for primary hyperaldosteronism. 02:00 Now, couple of things to keep in mind if you're doing this test in your patients. 02:03 You do not want these patients to be taking aldosterone antagonists. 02:07 Things like spironolactone or eplerenone. 02:11 They have to be discontinued for at least 6 weeks prior to testing. 02:14 They have a very long half-life and if you think about these medications, these are competitive antagonist for the mineralocorticoid receptor. 02:21 So, if that happens, of course, then patients are going to falsely have a high aldosterone. 02:27 So, do keep that in mind and make sure your patients are not taking those medications when you're doing this test. 02:32 The remainder of antihypertensives should not pose a problem. 02:35 You should be aware that ACE inhibitors and ARBs can increase renin levels but typically, it's not significant in the setting of primary hyperaldosteronism. 02:45 So, once we have that aldosterone to renin ratio, we still have to do confirmatory testing because we wanna make sure that aldosterone wasn't activated just because that patient perhaps was volume-depleted. 02:59 So, what we're gonna do is we're actually gonna sodium load our patient. 03:03 I know it seems counterintuitive because we feel like our patient is already volume overloaded but this is really important in order to really clinch that biochemical diagnosis. 03:11 So, we have a couple of different options of doing this. 03:14 The first option which, I think, is more fun for patients is you can put them on a very high sodium diet. 03:19 That means that they have to eat at least 5 g of salt per day which is somewhere around 90 mEq/day. 03:26 We then do that over a 3-day period of time. 03:31 At the end of that time period, we do a 24-hour urine collection for aldosterone. 03:36 We also wanna check urinary sodium and creatinine levels to ensure that we have an accurate collection, number one, and to ensure, number two, that they've taken enough sodium. 03:46 We then look at our urinary aldosterone concentration and if it's greater than 14 micrograms, this is will confirm that that patient does, in fact, have primary hyperaldosteronism. 03:57 Another way that probably is a little bit easier is to actually administer isotonic saline. 04:03 So, we bring our patient into our office, we do an infusion of isotonic normal saline. 04:08 Remember, that has about 9 grams of sodium chloride per liter so that's a fair amount of salt if you think about that. 04:14 They're in the recumbent position, we administer it over 4-hour period time. 04:19 We then want to measure plasma aldosterone levels and they should fall to less than 5 ng/dL in normal subjects. 04:27 So, if your patient has a value that's greater than 10 ng/dL, that's a positive result and that patient has biochemical evidence of primary hyperaldosteronism. 04:37 So, your job is not yet over though. You have to figure out where is that coming from. 04:44 So, we have to go on further in our imaging or in our diagnostic tree to figure out where this is coming from. 04:51 We have to distinguish whether this patient has a unilateral adenoma, rarely corticocarcinoma, from bilateral adrenal hyperplasia once we have biochemical confirmation. 05:02 So, our next step in our diagnostic tree is to obtain imagining with the CT of the abdomen. 05:08 This has, however, a sensitivity and specificity that are only moderate so we see a lot of false positives and can see some false negatives. 05:17 Why do we get false positives? Because these images can actually detect a nonfunctioning adenoma, what we can an incidentaloma when the patient actually has bilateral adrenal hyperplasia. 05:29 If you look at my image on the right, this is an axial CT scan which shows an adenoma at that adrenal gland on the right. 05:39 So, what can we do in order to confirm that that adenoma that we saw on that last picture is actually functioning? Because I want you to think about if I actually have an endocrine surgeon go in there and perform a surgical invasive procedure on my patient, take that adenoma out and that patient still has primary hyperaldosteronism. 06:01 I've really done a disservice to that patient. 06:03 So, I have to prove that that adenoma is functional, that it is secreting aldosterone. 06:08 And the way I do that is with adrenal vein sampling. 06:11 This is predictive for a successful unilateral adrenalectomy. 06:16 So, what we do is we have our interventional radiology colleagues, our vascular colleagues, or interventional nephrology colleagues go in, sample the actual adrenal vein. 06:26 It's quite difficult to do but when they do this, they are looking for a five-fold increase in plasma aldosterone concentration on the side with the adenoma compared with the contralateral side. 06:39 That actually will confirm that that adenoma that you see is functional and can be removed. 06:46 Now, one of the problems with adrenal vein sampling is it's very technically difficult to do so there's probably only very few centers who do this well. 06:56 Okay, so, once we have a biochemical confirmation, once we've got imaging confirmation, and adrenal vein sampling, and we see that yes, in fact, that adenoma that we saw on that CT scan is functional, it needs to be removed. 07:10 Then, we call in our endocrine surgery colleagues and they come in, and they do a laparoscopic surgical removal for us. 07:17 Now, something that I want you to keep in mind, those patients, remember, are extraordinarily hypertensive so it's important to pre-treat them for about 3-4 weeks with an aldosterone antagonist like spironolactone or eplerenone so that they are medically suitable to undergo a surgical operation. 07:34 How about our patients who have bilateral adrenal hyperplasia? So, in those particular patients, they actually just are treated with spironolactone or eplerenone, which are aldosterone antagonists, indefinitely. 07:46 They can do quite well but I do want you to keep in mind, those doses can be quite high. 07:50 So, for example, in a patient who has primary hyperaldosteronism due to a bilateral adrenal hyperplasia, it's not uncommon to see a dose like 200 mg, three times a day of spironolactone.
About the Lecture
The lecture Primary Hyperaldosteronism – Secondary Hypertension by Amy Sussman, MD is from the course Secondary Hypertension.
Included Quiz Questions
Which of the following is true regarding the diagnosis of primary hyperaldosteronism?
- A ratio of plasma aldosterone concentration to plasma renin activity of >35 is suggestive of primary hyperaldosteronism.
- A ratio of plasma aldosterone concentration to plasma renin activity of >35 confirms primary hyperaldosteronism.
- Aldosterone antagonists should be stopped for at least 6 weeks before testing because they may give false-negative results.
- Patients with primary hyperaldosteronism usually present with hypertension, unexplained hypokalemia, and metabolic acidosis.
Which of the following is correct regarding the management of primary hyperaldosteronism?
- Laparoscopic adrenalectomy is the preferred treatment for patients with unilateral adenoma.
- Patients with bilateral adrenal hyperplasia should be treated with aldosterone antagonists for 3 to 4 weeks before laparoscopic adrenalectomy.
- Patients with unilateral adrenal adenoma should be on aldosterone antagonists indefinitely.
- ACE inhibitors/ARBs are the first-line treatment for primary hyperaldosteronism.
What is the limitation of using CT in the workup of primary hyperaldosteronism?
- It may detect incidentaloma instead of bilateral adrenal hyperplasia.
- It is invasive.
- Only a few centers have this imaging modality.
- It is time-consuming and operator-dependent.
What is the reason for measuring urine sodium and creatinine in the sodium loading test?
- To ensure accurate urine collection and sodium intake
- To distinguish adrenal adenoma from bilateral hyperplasia
- A urinary sodium level of >14 μg/day is diagnostic for primary hyperaldosteronism.
- To distinguish primary hyperaldosteronism from secondary hyperaldosteronism
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |