Playlist
Show Playlist
Hide Playlist
Portal Venous Hypertension, Superior and Inferior Vena Cava Syndromes
-
06 CVP Vein and Lymphatic Pathology.pdf
-
Reference List Pathology.pdf
-
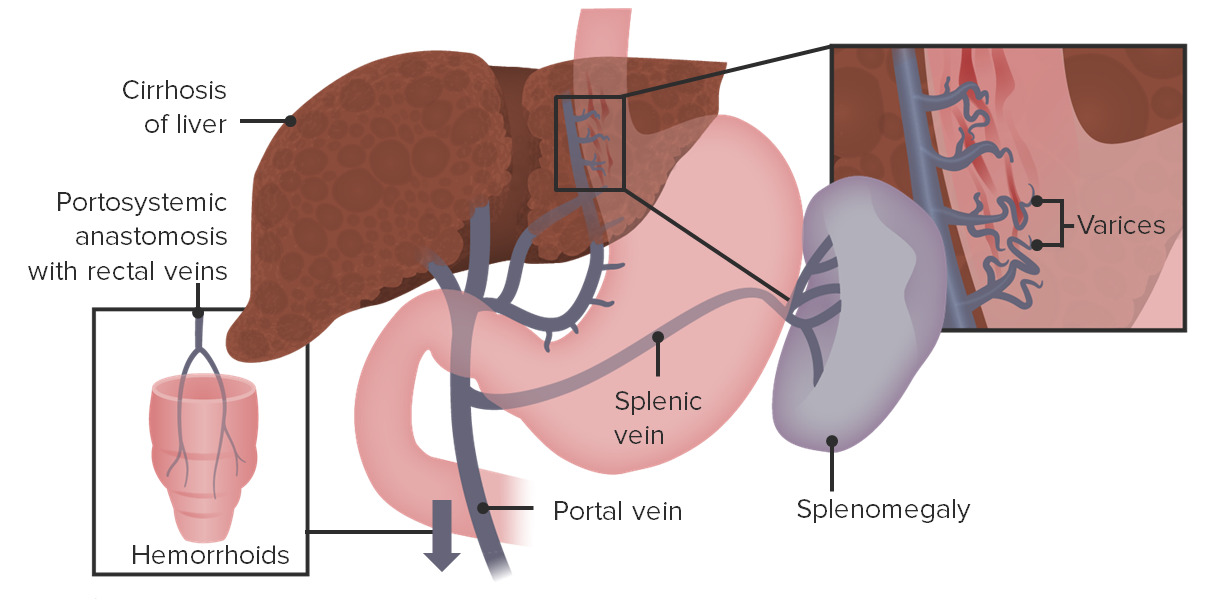
Download Lecture Overview
00:01 So, we've talked about, venus kind of extremity, occlusion, stasis and we talked about peripheral versus deep, we talked about, kind of the complications. 00:14 Let's talk about portal venous changes, in other vascular beds and specifically here, we're talking about portal venous hypertension. 00:24 This is where the blood pressure in the portal vein, going into the liver, is elevated. 00:28 The most common, far and away the most common cause, is liver cirrhosis. 00:34 With that scarring that goes on in the liver, now blood flow, through the liver is going to be compromised, there's going to be relative stasis, and increased portal pressure, trying to get through all of that scarring. 00:48 It can also happen with portal vein obstruction and there are some rare birds, that give rise to portal vein obstruction, but it can also occur with certain forms of chemotherapy, so, the outflow from the liver, becomes compromised because of the portal vein obstruction. 01:08 You can have hepatic vein thrombosis, which also occurs with certain chemotherapies and certain drug agents. 01:16 Portal hypertension, leads to now shunting, so, the blood that cannot normally get through the portal circulation into the liver, will go to other places portosystemic shunting. 01:28 There are three main areas in the body, where the shunts occur. 01:33 One is through the portal vein into the periesophageal veins, forming esophageal varices. 01:42 So, esophageal varices indicated here in the green circle, are dilations now, of the venous circulation, around the esophagus. 01:51 Why is that bad? Well in fact, those dilated veins, have very little mucosa over the surface. 01:59 They are under increased pressure and if we get mucosal erosion or injury to the esophagus, they will bleed like crazy, they can lead to massive and even fatal upper gastrointestinal hemorrhage. 02:09 So, esophageal varices are a big deal, in patients who have portal hypertension. 02:15 Another kind of portosystemic shunt, is at the rectum, so this will form hemorrhoids, and I will warn you the next picture is not pretty, but is an example of what hemorrhoids look like. 02:27 They're basically just varicose dilations, of the venous plexus, at the anal rectal junction. 02:32 And yes, you were looking at the anorectal junction in this individual, with very dilated veins. 02:38 That can be painful, it can occur not only with cirrhosis and portal hypertension, but also from prolonged pelvic vascular congestion, associated with pregnancy, or with straining to defecate, so, if you're constipated, you can also get these. 02:54 They’re a source of bleeding, they're not going to be as bad bleeders, as esophageal varices, and you're less likely to die of this, but you may feel like you want to die, they are painful. 03:07 Okay and then the third site, where you get a portosystemic shunt, is at the umbilicus. 03:13 So, this is periumbilical veins of the abdominal wall and it forms a classic, what's called a caput medusae, which is the head of the Medusa. 03:23 Those of you who are not classically trained scholars, that's what the Medusa looks like, she had instead of hair, she had snakes. 03:30 And if you gazed upon her, you would turn to stone. 03:33 Well, someone back in the archives of medicine, thought that, the dilated periumbilical plexus looked like her head. 03:44 So, there you have it the caput medusae, which is the third portosystemic shunt. 03:51 Okay, other occlusions of the venus circulation. 03:55 We have the superior/inferior vena cava syndrome. 03:58 So, again you know now, that the inferior vena cava brings blood from the lower extremities and the lower organs to the heart. 04:05 Superior vena cava brings from the upper extremities, in the head and neck to the heart. 04:11 Superior vena cava syndrome is caused by tumors, that compress or invade the superior vena cava. 04:18 Very commonly this is going to be bronchogenic carcinoma, more rarely is going to be mediastinal lymphomas. 04:24 It can also be caused by thrombosis, associated with an intravascular intervention, such as a dialysis catheter, less likely in this location. 04:33 But pacemaker wires, very commonly, can cause a superior vena cava syndrome, by irritating the vessel wall, causing the thrombosis, not allowing blood flow through. 04:42 Pulmonary vessels, can also be compressed as a result of having extrinsic compression and that can cause respiratory distress, because you're not getting blood flow through the lungs, and so, you're not getting adequate oxygenation for the rest of the body. 04:56 Inferior vena cava, so different than superior vena cava. 04:59 Inferior vena cava syndrome is caused by neoplasms that compress or invade the IVC. 05:05 Hepatocellular carcinoma and renal cell carcinomas in particular, like to grow along their venous circulation into the IVC and up towards the heart. 05:16 And so, they can be a source of occlusion and cause an IVC syndrome. 05:21 This is just showing a renal artery carcinoma, growing there out of the left renal vein, and into the inferior vena cava. 05:34 You can also have compression, causing the inferior vena cava syndrome by having a pregnancy or obesity, as we discussed previously. 05:42 So, what is this like? Basically, we're not getting blood flow coming back up from the lower extremities, we're increasing venous pressure, by virtue of having occlusion of that IVC. 05:52 So, you can get peripheral edema very easily, you can get the veins or the blood flow trying to find other ways back to the heart, so, you can get dilation, of kind of the venous plexus over the abdomen, so you can see very prominent venous stasis and because you impact renal function, by having this occlusion of the IVC, you can get extreme proteinuria, which will then exacerbate edema.
About the Lecture
The lecture Portal Venous Hypertension, Superior and Inferior Vena Cava Syndromes by Richard Mitchell, MD, PhD is from the course Vein and Lymphatic Pathology.
Included Quiz Questions
What is the most common cause of portal hypertension?
- Liver cirrhosis
- Portal vein thrombosis
- Hepatic vein thrombosis
- Congestive heart failure
- Parasite Infection
Which of the following tumors has the tendency to invade the inferior vena cava?
- Renal cell carcinoma
- Cardiac rhabdomyoma
- Meningioma
- Bronchogenic carcinoma
- Chondroma
What could be a complication of superior vena cava syndrome?
- Dyspnea
- Lower extremity edema
- Bleeding from the hemorrhoids
- Bleeding from the esophageal varices
- Formation of caput medusa
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |