Playlist
Show Playlist
Hide Playlist
Plaque: Structure and Rupture
-
Slides Plaque Morphology and Complications.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
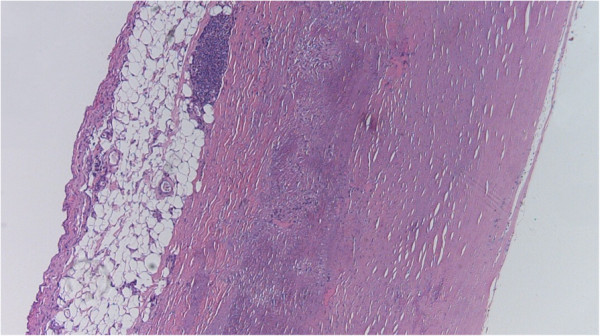
00:00 Let's talk about the risk of plaque rupture. 00:03 This slide should scare the daylights out of you, scares the daylights out of me. 00:09 This was a study that was done back in the 60s, maybe 70s, by Dr. Peter Davies. 00:14 And what he demonstrated was that majority of atherosclerotic plaque ruptures on less than critical stenosis. 00:24 Let me say that, again, the majority of acute events happen when you have atherosclerotic stenosis less than what you would have had to get symptoms. 00:36 So you can be completely angina free. 00:39 Up to 60%, chronic stenosis, and not ever know you have atherosclerosis and then suddenly, all heck can break loose, that plaque ruptures and you get a thrombus. 00:51 So what's been demonstrated on the image on the left hand side is an atherosclerotic plaque. 00:57 And the green arrows indicate areas of plaque rupture. 01:00 Now with an acute thrombus superimposed on it, you were looking at what caused the death of this unfortunate individual. 01:08 The atherosclerotic plaque is there. 01:10 And that would have been about a 60% chronic stenosis. 01:14 And yet, no symptoms. 01:16 And yet, it ruptured, and we have the patient die as a result of that. 01:21 See the red line on the right, so if you, the number of cases that had a plaque rupture, fatal cases of myocardial infarction, and Dr. Davies looked at how many, what degree of stenosis was in each of those vessels. 01:34 In about 13% of cases, there was less than 30% stenosis, another 13% of cases had 40%, stenosis, 16%, 50%, and 20% of cases had 60%, stenosis. 01:47 All of those up to 60%, totally asymptomatic, and yet they correspond to 70% of the events, leading to an acute demise due to plaque rupture and myocardial infarct. 02:02 So that's why it scares the daylights out of me, because I'm walking around with no chest pain, no critical stenosis, and yet, I know that I probably have atherosclerotic plaque in some of my vessels, that is at risk of rupturing. 02:14 So can we predict that? Answer is kind of yes and no. 02:19 So how can we stratify? And this is where we get into the notion of vulnerable plaque versus stable plaque. 02:28 A vulnerable plaque has a much larger lipid core, as you can see there on the left. 02:34 It's also got a relatively thin fibrous cap. 02:38 And it's got relatively more amounts of inflammation. 02:42 And inflammation is important not only because it's a driver of atherosclerosis, but also because those inflammatory cells are making matrix proteases that can break down that thin fibrous cap. 02:56 So the greater the lipid core, the more deformable is the plaque. 03:00 The thinner the cap, the more likely it can rupture and the more inflammatory cells, the more likely that we will break down matrix and we'll get rupture. 03:07 That's one that's likely to blow. 03:10 As compared to the stable plaque on the right. 03:15 Here we have a relatively smaller lipid course. 03:18 So this plaque is not as deformable with flow in the lumen. 03:23 The fibrous cap is much thicker, so it's going to be more stable and much less likely to rupture, and there's less inflammation so there are fewer proteases less amount of degradation of the extracellular matrix. 03:36 So vulnerable and stable. 03:38 Just to give you a sense of what that looks like, this is a relatively stable plaque on the left. 03:43 It's got a relatively high amount of extracellular matrix and their atheromatous plaque that is sitting near the bottom of the vessel. 03:52 And we can also see that there's relatively minimal amounts of clearing, which would represent the fatty core the atheromatous core. 04:01 As compared to this one, where there is a much greater atheromatous core, all that clearing on the left hand side is a big fatty cholesterol and necrotic debris laden core and the cap over the surface much thinner. 04:15 So, this one is going to be much more prone to rupture. 04:21 Whether a plaque will rupture or not, is a given take, a push and pull between matrix synthesis driven by macrophages that are going to be making TGF beta that are going to be acting to make more matrix. 04:35 So more collagen and elastin versus matrix degradation. 04:40 So, T-cells and the factors that they elaborate, can act on macrophages to drive more matrix metalloproteinase production, which will degrade the matrix. 04:53 So it's a push and pull whether or not a plaque will acutely rupture. 04:59 And this is driven by different macrophage populations. 05:02 I think we have talked about this. 05:04 In fact I know we have talked about this previously when we talked about wound healing. 05:08 The monocytes have two different flavours, when they become macrophages, on the left hand side is the classically activated macrophage which is very pro inflammatory and more prone to matrix degradation. 05:21 On the right hand side is the alternatively activated M2 macrophage, which is anti inflammatory and makes more matrix. 05:29 What is going on in atherosclerotic plaque will determine whether we have more M1 or more M2 macrophages. 05:38 And that will ultimately also drive whether or not we get an acute plaque rupture. 05:45 So, we can see on the left hand side we can see our atherosclerotic plaque with macrophages and T-cells interacting with each other, but they can be driven by inflammation, microbes and other factors to release proteases that will drive plaque rupture. 06:03 And that's what's being shown on the right hand side, once again. 06:07 A plaque rupture can also be triggered by a number of other events. 06:11 So we're looking at a longitudinal view of a, of an atherosclerotic packet within a vessel. 06:18 And we're going to have a plaque rupture right there. 06:22 Now with flow going from left to right, we are going to induce thrombus overlying that area. 06:29 But how we got the plaque rupture in the first place is actually what the slide is about. 06:37 So physical exertion, as you increase blood flow, pulsatility, and other things like that will drive pulsatile flow over the surface and if we have a deformable plaque is more likely to rupture. 06:52 Mechanical or emotional stress by causing vasospasm. 06:57 We can actually change plaque conformation and make it more prone to rupture. 07:02 And elevated heart rate just by increasing the local pulsatility will also increased risk, elevated blood pressure, vasospasm, inflammation, all these can drive plaque rupture, and then we get a thrombus and then we're having a myocardial infarct. 07:20 The important point about plaque rupture. 07:23 And this gets back to Peter Davies observations about the degree of stenosis in the setting of where we do eventually have plaque rupture. 07:31 It's a completely unpredictable event. 07:33 Right now, we lacked the tools to reliably identify vulnerable plaque For starters, but also plaques that are at the risk or right on that kind of tipping point to rupturing. 07:47 And we just don't have that capacity to identify those yet. 07:51 And that's where you come in. 07:53 So keep up the good work. 07:54 So again, to recapitulate, vulnerable plaques, thin cap, large liquid pool, many inflammatory cells, relatively fewer smooth muscle cells, versus stable plaque, which has got a much thicker cap, small lipid pool, few inflammatory cells, many smooth muscle cells. 08:14 Important point so we also are constantly seeking to improve the risk, diminish risk, improve risk for our patients. 08:25 And to do that we frequently give patients statins. 08:28 Well, statins we're designed originally is HMG, Hydroxy-methyl-glutaryl CoA reductase inhibitors that would block the synthesis of cholesterol. 08:39 So statins in addition to that, also stabilize plaque there, we can convert a vulnerable plaque to a more stable plaque by the administration of statins and so by increasing HDL, decreasing LDL, those are the actions that we know about, but they also are anti inflammatory. 08:59 So statins have an anti inflammatory effect need to decrease macrophage activation, they decrease the production of tissue factor, they increase collagen, and although the lumen may not regress, the risk of plaque rupture goes down dramatically. 09:15 So yet another reason to put all of our patients on statins.
About the Lecture
The lecture Plaque: Structure and Rupture by Richard Mitchell, MD, PhD is from the course Atherosclerosis.
Included Quiz Questions
Up to what percent of stenosis remains an individual with atherosclerotic plaque usually asymptomatic?
- 60-70%
- 10-20%
- 0-30%
- 40-50%
- 90%
What is a feature of a vulnerable plaque?
- Large lipid core
- Minimal inflammation
- Thick fibrous cap
- Large lumen
- Rigid fibrous cap
What is the mechanism of TNF-alpha in causing plaque rupture?
- Causes matrix degradation
- Promotes matrix synthesis
- Produces collagen
- Produces elastin
- Promotes stable plaque
What type of macrophage is responsible for acute plaque rupture?
- Classically activated macrophage
- Alternatively activated macrophage
- Anti-inflammatory macrophage
- Matrix-synthesizing macrophage
- Stable macrophage
Which of these may trigger acute plaque rupture?
- Stress
- Hypotension
- Bradycardia
- Vasodilation
- Laminar flow
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |