Playlist
Show Playlist
Hide Playlist
Peripheral Vascular Disease (PVD): Examination & Diagnosis
-
Slides Peripheral vascular disease Special Surgery.pdf
-
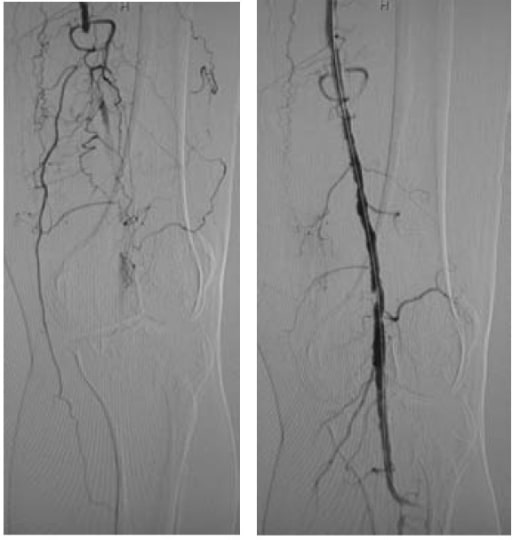
Download Lecture Overview
00:01 Now, whenever I'm faced with a patient who complains of malperfusion in the lower extremities, sometimes call claudication or rest pain, I ask myself some very important questions. 00:13 Number one, how far can the patient walk? Two, is there pain when the patient wakes up? And three, are there any ulcers or signs of malperfusion. 00:25 With the answers to these three common and important questions, one can have a very good idea of the level of the vessel stenosis and whether anastomosis is even present. 00:39 Let's take a look at some physical findings? And very importantly, differentiate claudication versus rest pain. 00:46 In claudication, pain is usually induced with exercise, but resolves with rest. 00:51 And this occurs over approximately two to five minutes as opposed to rest pain. 00:56 Rest pain usually is in the forefoot and toes and the pain can be worsened if the leg is raised or in a recumbent position. 01:03 This make sense. 01:04 In a recumbent and/or raised position, there's even further decreased flow. 01:10 And sometimes, the pain is relieved by dangling the foot or the feet over the bed. 01:15 We alluded to this ankle brachial index, also called an ABI. 01:20 As you examine the pulses, very importantly, check every pulse from the abdominal aorta down to the femoral system, popliteal, dorsalis pedis and posterior tibial system. 01:33 How can you objectively identify whether or not there is a pressure drop gradient from your brachial to your ankle? Well, it’s by the angle brachial index. 01:43 An ABI, or the ratio between systolic blood pressure in your ankle and the systolic blood pressure in your arm, less than 0.4 is highly suggestive of rest pain. 01:55 Remember, ankle brachial index is extremely sensitive and specific. 01:59 And additional studies are usually not necessary to simply diagnose peripheral occlusive arterial disease. 02:05 But remember, imaging may be useful for surgical planning. 02:12 Unfortunately, routine laboratory studies are unlikely to be helpful unless there's some infection going on. 02:18 Whether it's an non-healing toe or a gangrene, you may see an infection and an elevated white blood cell count as a result. 02:29 Let's move on to some helpful imaging diagnosis. 02:33 Using a duplex, again, it’s operator dependent. 02:36 It's an ultrasound technology that introduces no radiation to the patient. 02:41 The duplex has the additional advantage of giving velocities. 02:44 Recall, velocities are higher in stenotic regions. 02:49 And with a Doppler or ultrasound, we can also get some anatomic idea. 02:54 Next, this image shows a fairly classic CT angiography. 02:59 Arteriograms is the gold standard0 for diagnosis of vascular disease. 03:04 As a multidetector slice CAT scan’s cross-sectional imaging improves, CTs are slowly replacing invasive arteriograms. 03:14 Here, highlighted by the circle as well as the arrow, this arteriogram shows narrowing and occlusion in the tibial system. 03:20 If you look further down the extremity, you notice that there are some wisps of contrast filling. 03:26 That's called reconstitution and runoff. 03:30 Increasingly, magnetic resonance imaging is being used for arterial disease. 03:36 Here, you see a nice depiction of an MRA. 03:39 There appears to be some occlusive disease in the right lower extremity. 03:44 And lastly, given all the cross-sectional imaging, modern technology allows us to do 3-D reconstructions. 03:51 Here, you see a nice example of aneurysms just above the knee. 03:55 They’re marked in red.
About the Lecture
The lecture Peripheral Vascular Disease (PVD): Examination & Diagnosis by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
An extremely sensitive and specific test for peripheral vascular disease is the ABI. Which of the following values is the threshold for an abnormal ABI?
- < 0.9
- < 0.1
- < 0.2
- < 0.6
- < 0.4
Which of the following tests is the gold standard for the diagnosis of peripheral vascular disease?
- Arteriogram
- Treadmill test
- Magnetic resonance Imaging
- Doppler ultrasonography
- Blood tests
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |