Playlist
Show Playlist
Hide Playlist
Peripheral Neuropathy: Anatomical and Functional Classification
-
Slides Introduction to Neuropathy Disorders.pdf
-
Download Lecture Overview
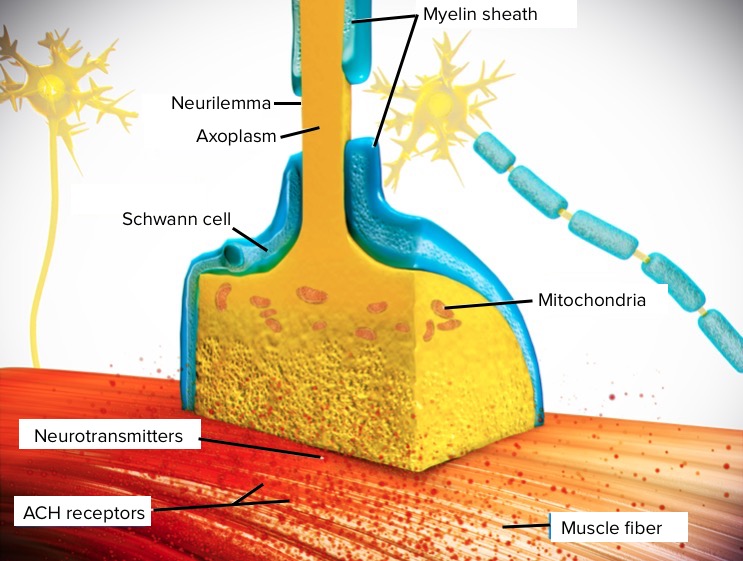
00:01 So, let's talk a little bit about peripheral nerves, peripheral neuropathies, and understand how we approach the patient in our case. 00:08 Let's begin with anatomy. 00:10 The peripheral nerve actually begins in the central nervous system, in the spinal cord. 00:15 Sensory nerves in the dorsal aspect of the cord and the motor nerves in the ventral aspect of the cord. 00:22 The sensory nerves enter in the dorsal root. 00:25 The cell bodies lie in the dorsal root ganglion, then exit out into the peripheral nerve. 00:31 In the ventral horn, we have motor nerves beginning in the ventral rootlets, and then connecting with the sensory nerves to form a peripheral nerve. 00:42 If we hone down and even more specifically to the peripheral nerve itself, we see that there's three compartments involved in the peripheral nerve. 00:50 The outside of the nerve itself is called the epineurium. 00:56 This is the outermost layer. A dense, irregular connective tissue makes up this layer, this firm connective tissue around the nerve. 01:05 As we move inward, the perineurium contains the blood nerve barrier. 01:10 There are blood vessels around each nerve fascicle and a blood nerve barrier preventing toxins or metabolites from getting into the nerve. 01:21 And then, the smallest compartment within the nerve is contained within the endoneurium. 01:25 This is the innermost layer of loose connective tissue, and it contains each nerve fascicle. 01:33 When we think about the anatomy of a neuron, sensory and motor nerves contain a cell body and an axon. 01:40 The cell bodies for the sensory nerves lie in the dorsal root ganglion, and for the motor nerves and the ventral horn of the spinal cord. 01:48 And there's important anatomic features that help the nerve to function. 01:51 One is myelin. Myelin is separated by these areas of nodes of Ranvier, and we know that that helps to propagate action potentials down a nerve or up a nerve to send signals more quickly. 02:04 That process is called saltatory conduction and it's an important function of the myelin. 02:10 Neuropathies that result in demyelination will slow down the conduction velocity along an action potential and along the axon and result in patient symptoms. 02:21 When we think about the neuroanatomy of the peripheral nervous system, there are both sensory and motor nerves. 02:26 Sensory nerves collect information from inside and outside the body. 02:30 They begin with free nerve endings, which is the terminal component of the sensory nerve. 02:36 Information is traveled down the axon, the cell bodies are contained within the dorsal root ganglion, and ultimately, they synapse in the spinal cord, relaying with interneurons in the spinal cord, and then projecting up to the thalamus and central nervous system. 02:51 The motor nerves begin in the ventral horn. 02:53 Cell bodies lie in the ventral horn, exit out those ventral rootlets into the peripheral nerve, and ultimately synapse on the neuromuscular junction to innervate muscles and result in muscle contraction. 03:05 And when we think about neuropathies, neuropathies can affect any combination of those nerves. 03:10 The vast majority of neuropathies are sensory motor polyneuropathies that affect both the sensory and the motor nerves. 03:17 But we do see neuropathies that affect only the sensory nerves, and those are termed sensory ganglionopathies, and neuropathies that affect only the motor nerves and the motor neuronopathies. 03:29 So, when we're evaluating a patient or looking at a case, we're looking to see whether they're sensory involvement, motor involvement, or a combination of those two to drive at what may be going on and narrow our differential diagnosis. 03:41 We can also look at the anatomy of the types and size of nerves that are in the peripheral nervous system. 03:49 So, let's start with the motor nerves. Motor nerves are large fiber nerves. 03:53 Information is carried in the A Alpha nerves. Those are myelinated motor nerves. 03:59 They begin in the anterior horn cells, and they innervate muscle fibers. 04:03 And you can see here, they're the largest nerves in the body, and they contain the thickest and most amount of myelin. 04:11 When we move to the sensory nerves, we also have large fiber sensory nerves. 04:15 Those are our A Alpha myelinated sensory nerves, and that carries stretch information from muscle spindles. 04:22 So, when you tap a reflex sensory nerve that feels the stretch of that muscle and ligament are these A Alpha myelinated sensory nerves, and they carry that information back to the spinal cord to generate a deep tendon reflex. 04:35 They are also large nerves and heavily myelinated. They carry information quickly. 04:40 The other large fiber sensory nerves are the A Beta myelinated sensory nerves, and they carry information from the mechanoreceptors. 04:49 Information like proprioception, vibration, and light touch, and so problems that affect a large fiber nerve can result in dysfunction of proprioception, vibration, or light touch. 05:00 Importantly, large fiber nerves carry information about vibration, proprioception, and light touch. 05:07 So, when patients present with those symptoms, we want to interrogate a large fiber neuropathy. 05:13 As we move down into smaller nerves, there are small fiber sensory nerves, and those are the A Delta partially myelinated nociceptive and touch pressure nerves. 05:24 They carry information from free nerve endings and problems with those nerves present with pain, burning, tingling, neuropathic pain. 05:33 We also have small fiber nerves that are sensory nerves that are unmyelinated. 05:39 And those are the C fiber nerves. They're unmyelinated. Primarily nociceptive nerves. 05:44 They carry pain and temperature information. 05:47 And importantly, the small fiber nerves carry information about pain, temperature, and some light touch. So, small fiber neuropathies will present with severe neuropathic pain. 05:59 In patients that present with neuropathic pain, we need to interrogate for a small fiber neuropathy. 06:06 Now, let's think about the neuroanatomy of the peripheral nervous system. 06:09 How are the sensory nerves connected to the motor nerves and how do we interrogate them with our reflex exam? Well, here, we're looking at a schematic of those connection points. 06:19 We have the alpha motor neurons in the ventral horn and the gamma motor neurons in the ventral horn. 06:25 The alpha motor neurons help volitional muscles to move, and the gamma motor neurons keep the muscle tendon-muscle spindles tight. 06:34 On the sensory side, we have group 1a afferents and Group 2a afferents, which feel stretch of the muscle spindle. 06:43 So, when we tap on a deep tendon reflex, that information is carried into the spinal cord, through the group 1 and 2 afferents. 06:50 There's a relay and synapse to both motor nerves, and this results in stretch of the extrafusal muscle fibers from the alpha motor nerves and keeping those muscle spindles taut is innervation of the intrafusal muscle fibers from the gamma motor nerves. 07:07 So, when we're evaluating deep tendon reflexes, we're really looking at that sensory motor arc. 07:12 the group 1-2 afferents and the alpha gamma motor efferents. 07:17 Reflex testing is a critical part of evaluating peripheral nervous system pathology and we can see hypo or areflexia from sensory neuropathies, motor neuropathies, and sensory motor polyneuropathies. 07:31 When we think about the motor nerves, there are both somatic and visceral motor nerves. 07:35 The alpha motor neurons arise from the ventral horn and innervate the muscles. 07:39 The gamma motor neurons innervate the muscles spindles to keep them taut and help to maintain postural tone. 07:46 And then, the motor nerves also have visceral innervation, both special and general. 07:51 And motor neuropathies can affect the somatic or visceral functions.
About the Lecture
The lecture Peripheral Neuropathy: Anatomical and Functional Classification by Roy Strowd, MD is from the course Introduction to Neuropathy Disorders.
Included Quiz Questions
Which of the following parts of the nervous system are paired correctly?
- Dorsal root ganglion - sensory nerve cell bodies
- Endoneurium - containing the blood–nerve barrier
- Motor neurons - dorsal spinal cord
- Nodes of Ranvier - helping to slow conduction signals
- Sensory neuron - synapse at the neuromuscular junction
Which of the following will slow the conduction velocity of an action potential?
- Demyelination
- Myelination
- Presence of node of Ranvier
- Increased blood flow to the nerve
Which of the following nerve fiber types is responsible for muscle control?
- A-alpha
- A-beta
- A-delta
- Type C
- B-beta
A problem with which of the following would most likely be caused by a small fiber neuropathy?
- Temperature sensation
- Proprioception
- Light touch
- Vibratory sensation
- Muscle weakness
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |