Playlist
Show Playlist
Hide Playlist
Pericarditis
-
Slides Endocarditis Myocarditis and Pericarditis Cardiomyopathy.pdf
-
Reference List Pediatric Nursing.pdf
-
Download Lecture Overview
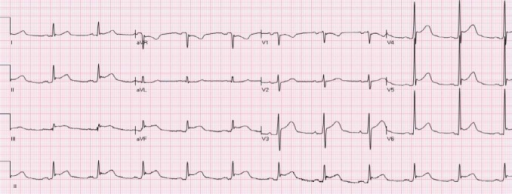
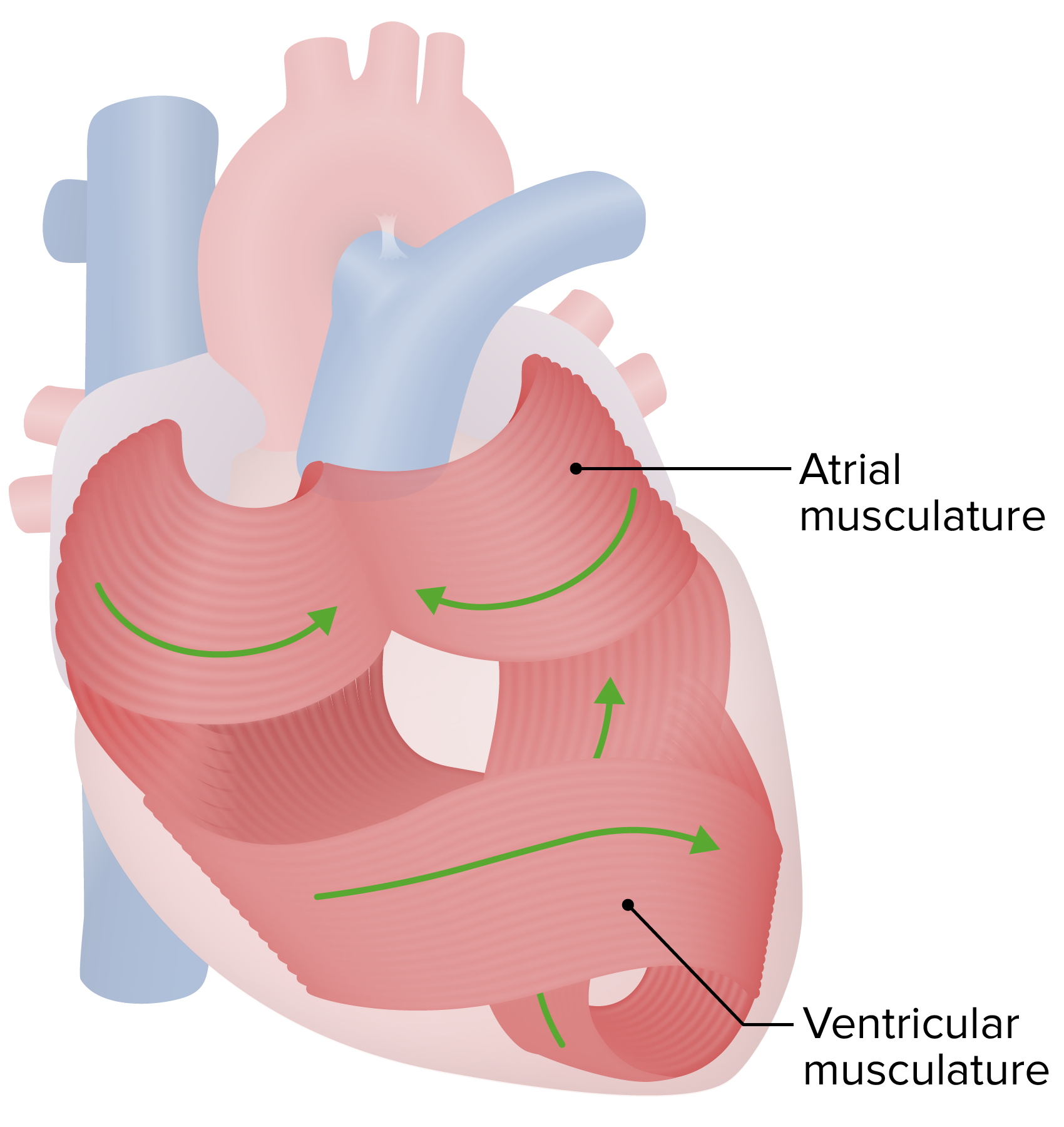
00:02 Let's shift gears a little bit and talk about pericarditis. 00:05 Remember, the pericardium is the sac around the heart. 00:08 This can get inflamed and can cause problems. 00:12 Most common causes are infections, and once again the cause is most likely Coxsackie virus, although may viruses can cause an acute pericarditis or inflammation in the sac around the heart. 00:26 Bacterial pericarditis is also possible, and that can be staph aureus. 00:32 Staph aureus pericarditis is usually a very aggressive, rapidly presenting inflammation of the pericardium. 00:41 Tuberculosis can cause pericarditis as usually a later finding. 00:46 These patients are more indolent in their presentation. 00:51 They come in a little bit later with prolonged fevers, you notice a friction rub and you start to figure out what's going on. 00:59 Drugs can cause pericarditis. 01:01 We don't see this as commonly in children, but hydralazine can cause it. 01:07 Procainamide can cause it. 01:08 Isoniazid, ironically, a treatment for tuberculosis, and also patients who've had radiation therapy. 01:15 Children who had a mediastinal mass and received radiation therapy may present years later with a pericarditis. 01:25 Also, the immune system can frequently present with pericarditis as an autoimmune presentation. 01:32 Classic diseases that cause this are rheumatic fever which can affect any part of the heart but certainly can cause a pericarditis. 01:39 In Kawasaki disease, we can often see a pericarditis in addition to the classic finding of coronary artery aneurysms. 01:48 And then of course pericarditis is possible in several connective tissue diseases. 01:53 We see it in children most commonly in lupus or SLE, and in juvenile idiopathic arthritis, or JIA. 02:02 So, a patient with pericarditis typically will present with a history of chest pain or shortness of breath that worsens when they're lying flat and improves when they're leaning forward. 02:15 Patients will typically present leaning forward and they won't want to lie back. 02:21 When you examine them, you'll notice a friction rub. 02:25 This is key, high yield on exam is the friction rub. 02:30 You want to place your stethoscope on their chest while they're leaning forward and listen. 02:35 It's a hard noise to describe. It's a low pitched friction-y, rubby sound that goes with the beating of the heart. 02:44 It's so unlike any other noise that you'll hear that the first time you hear it, you'll probably correctly make the diagnosis. 02:53 Pulsus paradoxus is often on exams but is actually not fairly common when you examine a patient. 03:01 It's on your test but it's not in the patient so commonly, but you can notice a pulsus paradoxus. 03:07 Remember, a pulsus paradoxus is when you only hear the first Korotkoff sound while the patient is exhaling. 03:15 As you lower the blood pressure you then hear it both in inhalation and exhalation. 03:22 A chest x-ray in pericarditis is gonna reveal cardiomegaly. 03:27 It's hard to distinguish that from myocarditis. 03:30 You'll get to see a large heart. 03:31 If you get an EKG, you're gonna see low voltage on those QRS. 03:36 They're low perhaps because the electrical interference of the inflamed pericardium. 03:44 You may see PR depression or ST elevation in about 80 percent of patients. 03:48 And again you'll see this electrical alternans where the direction of the QRS is migrating about during the course of that EKG. 03:58 The echo will show a poorly functioning myocardium if they're having myocardial involvement and again the viral serology and other blood testing is indicated if you suspect viral disease. 04:12 So, key points that you might see out of this lecture. 04:17 Remember Osler nodes, Janeway lesions, and Roth spots. 04:21 Remember to get that large volume blood culture for endocarditis. 04:25 Remember Coxsackie B virus is the viral cause of myocarditis or pericarditis. 04:32 Recall that myocarditis and pericarditis both show with low-voltage QRS, and you can distinguish between these two on echo. 04:41 And then remember for pericarditis, that patient is leaning forward and has a friction rub on auscultation.
About the Lecture
The lecture Pericarditis by Brian Alverson, MD is from the course Pediatric Cardiology.
Included Quiz Questions
What is the typical auscultatory finding in a patient with pericarditis?
- Friction rub
- Systolic ejection murmur
- Diastolic rumble
- Mitral valve click
- Washing machine murmur
Which of the following positions typically worsens the chest pain in pericarditis?
- Lying supine
- Sitting up and leaning forward
- Lying in the left lateral position
- Standing
- Squatting
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture as usual. I would have liked an explanation on why the pain is relieved when the patient is leaning forward in pericarditis. I liked the emphasis on the overlap between myocarditis and pericarditis. Thank you!
Straight to the point and high yield info. Dr Alverson does a great job throughout the lectures.