Playlist
Show Playlist
Hide Playlist
Peptic Ulcer Disease
-
Slides Stomach and Duodenum.pdf
-
Download Lecture Overview
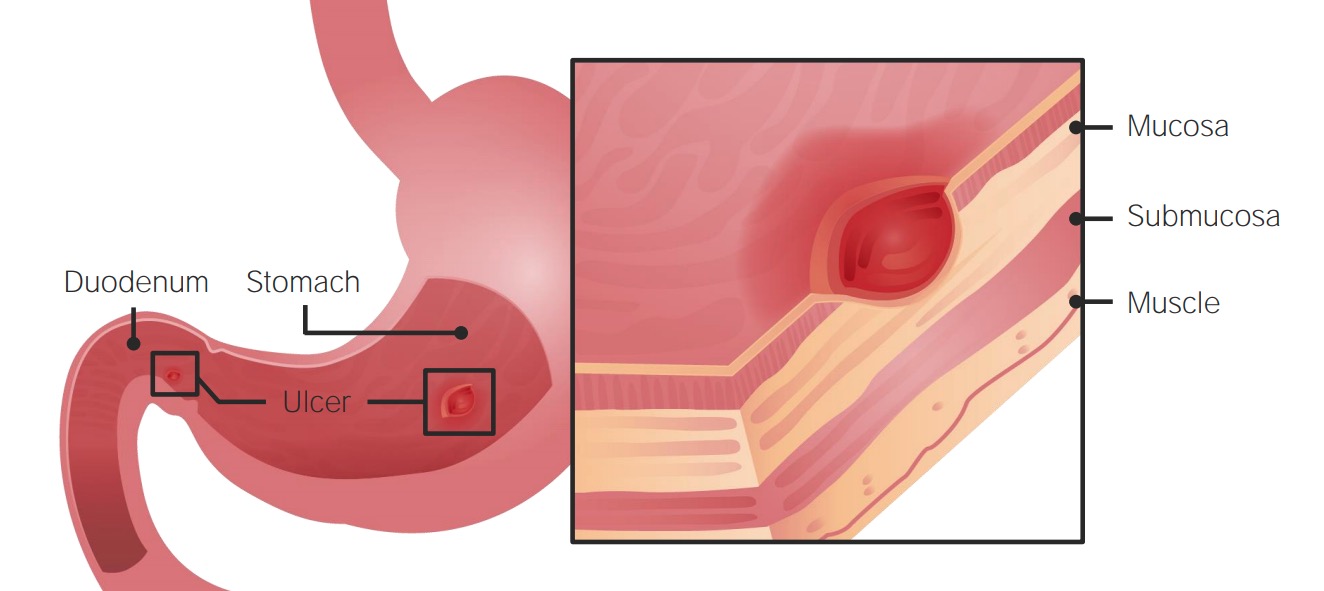
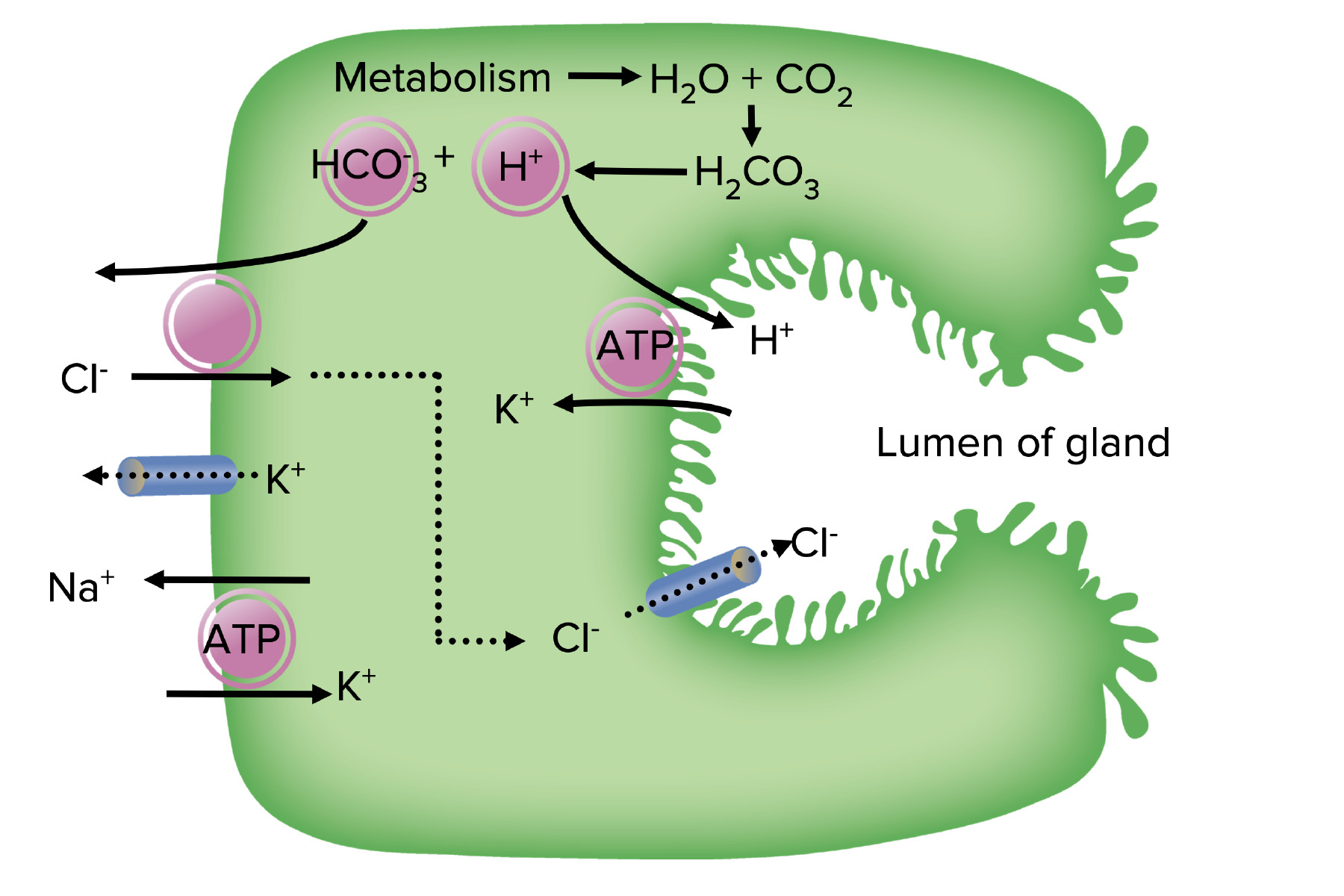
00:01 Our topic now brings us into, “Peptic ulcer disease.” A peptic ulcer disease you divide this into that disease, or erosion that's taking place in the stomach, versus that type of erosion that might be taking place in duodenum. 00:15 By far in the US, the most type of most common type of peptic ulcer disease, would be the type that's taking place in the duodenum, however, for learning purposes, we need to make sure that we cover both sets of peptic ulcer disease, and then, importantly, we will go through the symptoms of your patient, so that you're able to distinguish one from the other. 00:36 Mechanism of injury: If there's direct mucosal damage due to toxins (ethanol), NSAIDS, bile, H. pylori. 00:46 Now, for the most part, you can think of peptic ulcer disease taking place in the stomach, as really not due to increased acid production, remember that, the stomach is extremely effective, with protecting the lining of the stomach from the acid. 01:00 And due to all that bicarbonate, prostaglandins and such, so therefore, protecting the stomach from all that acid. 01:08 However, if the lining of the stomach has been compromised, where it could take place due to, let's say, NSAIDS, which is then inhibiting your COX pathway, then you might then inhibit the formation of the prostaglandin necessary to properly protect, or contribute to the protection of the stomach, or if there's actual chemical damage taking place to the lining of the stomach, due to bile, that might then regurgitate back into the stomach, remember bile, is being released or secreted from your gallbladder, into the second part of the duodenum, so therefore, there must be some kind of method, by which the bile is, retrograde flow back in the stomach causing damage. 01:56 H. pylori in the stomach would be residing where? In the antrum of the stomach and from henceforth, whenever you deal with H. pylori, you should be thinking either the distal end of the stomach, or the first part of the duodenum, as being its place of residence. 02:15 In the stomach the H. pylori if you remember from micro, then has an enzyme called urease. 02:20 Therefore, it'll take the urea and it will create a force field for itself, that force field that H. pylori then creates in the antrum of the stomach, is then made up of ammonia, amazing isn't it. 02:33 At some point in time, it could then burrow into the lining of the stomach, and so therefore weakening the lining, resulting in peptic ulcer disease. 02:41 H. pylori, bile, NSAIDS, alcohol. 02:46 Prostaglandin inhibition, like we just said with NSAIDS or steroids, even with pathologies such as, Cushing, in which you would have excess cortisol, hypercortisolism, is then knocking out your phospholipase A2, you don't have the necessary prostaglandin, to protect the lining of the stomach as such, against the acid. 03:07 Increased acid production could be a cause, but more importantly the most important pathogenesis for peptic ulcer disease of the stomach, would be damaged to the lining. 03:19 Whereas if it is pathogenesis peptic ulcer disease of the duodenum, then in fact it would be increased acid. 03:26 For example, if you do Zollinger-Ellison syndrome, and with the gastrinoma, with all that acid which is then coming out like a huge wave, out of the stomach and into the duodenum, there is no way that the duodenum can properly protect itself against the all that acid. 03:44 Mucosal ischemia, is always a possibility, whenever there is a infarction that's taking place, then at some point in time, you might then be hurting or injuring lining of the stomach. 03:57 Peptic ulcer disease, if it is in the stomach, the patient here, is going to be complaining of epigastric pain, however, this time around, the peptic ulcer disease in the stomach, you would not find, and the patient would not be complaining a pain, that's radiating to the back, is that clear? On your step, and on your wards, if the pain is radiating to the back, then this gives you the high suspicion and differential of pancreatic damage, however, if it's not, then you're thinking about peptic ulcer disease. 04:29 Also, with this erosion that's taking place, remember, you have not perforated, ulceration means ulceration, it's a clean punched up lesion in the stomach, and the clean punched out lesion here, with bleeding taking place, may result in hematemesis. 04:49 With all this blood that's now being released, either from the stomach or maybe perhaps the duodenum, you can only imagine that, as I told you earlier, that the stool has an opportunity to completely saturate itself with blood. 05:02 So, therefore by the time it's evacuated, here the stool, in fact is going to look black and tarry. 05:09 Hematemesis, hematochezia, iron deficiency anemia, all these, well, all part of bleeding. 05:17 Next, if there's perforation that's taking place, especially of the duodenum type of peptic ulcer disease, it will then perforate and then it will then affect different organs or blood vessels. 05:31 If it is peptic ulcer disease of the stomach, which is usually found in the lesser antrum of the stomach, and if it is the perforate, then you are then going to, or the perforation is going to affect the left gastric artery. 05:45 Whereas if the perforation takes place down in the duodenum, and then the perforation, then causes damage to the gastroduodenal artery. 05:55 Gastric obstruction due to peri-pyloric scar formation, is an important complication. 06:01 At some point in time, when there is enough damage that's taking place, any type of damage at some point, the body wishes to respond with the repair process. 06:09 This repair process that you're looking for, at some point with fibrosis taking place, may actually then cause, gastric outlet problems, because of the more or less think of it as being a stricture formation, or scar formation, and therefore, decreasing the emptying of the stomach. 06:29 Gastric ulcers may be malignant, while duodenum ulcers are basically never. 06:35 Once again, peptic ulcer disease, keep in mind that if it's the stomach, you should be monitoring or should be thinking, “The possibility of a primary gastric cancer developing” in duodenal, almost never. 06:52 On the left, peptic ulcer disease is in the duodenum, you'll notice that you have a clean punched out lesion, whereas a gastric ulcer, you also have a clean punched out lesion. 07:02 Endoscopy esophagogastroduodenoscopy, would be your guest best measure or best method of diagnosis. 07:11 With this ulceration, at some point remember, keep your ulceration and perforation completely separate. 07:21 Management of peptic ulcer disease. 07:23 Antacids. 07:25 Because of the burning sensation that's taking place, magnesium and aluminum cause long-term toxicity, be careful with antacids. 07:32 Magnesium and aluminium. 07:34 Milk alkali syndrome due to prolonged use of calcium, is something that you want to keep in mind with antacids. 07:40 Once again, milk alkali syndrome due to prolonged use of calcium. 07:46 PPIs are first line treatment for a PUD, and they're also used in combination with antibiotics to treat H. pylori. 07:54 Sucralfate. 07:55 It stimulates endogenous prostaglandin production so that it helps to then, protect the lining of the stomach. 08:03 Avoiding renal insufficiency, so, and that's a big deal. 08:07 So, the drugs that I've given here for management, I've given you as to what it does objectively, and then things that you want to keep in mind, as side effects, because these patients will be on these drugs for quite a bit of time. 08:24 Peptic ulcer disease. 08:25 We have two types, the duration of therapy if it's duodenal ulcer, being the most common type of presentation in the US, 4-6 six weeks of duration. 08:35 If it's a gastric ulcer, then at 6-8 weeks with repeated, esophagogastroduodenoscopy to document the healing. 08:42 The management remember H. pylori highly associated with, both of these issues, so therefore, the importance of eradicating H. pylori, cannot be understated, responsible for developing lymphomas perhaps, and maybe even our intestinal type of gastric primary adenocarcinoma. 09:03 Now, we have two types of treatments, so, you want to either think quadruple bismuth, and the quadruple therapy would include bismuth metronidazole, tetracycline and proton pump inhibitor, or you could have clarithromycin based triple therapy, which would then consist of, amoxicillin, clarithromycin and your PPI.
About the Lecture
The lecture Peptic Ulcer Disease by Carlo Raj, MD is from the course Stomach and Duodenum Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
A 75-year-old woman comes to the clinic complaining of constipation, vomiting, and a loss of appetite for the past 4 weeks. She has had a history of peptic ulcer disease for the past 10 years, for which she has been on medication intermittently. Which of the following is the MOST likely cause of her presentation?
- Gastric outlet obstruction
- Perforation of the ulcer
- Ulcer penetration
- Bleeding ulcer
- GERD
Which of the following pathophysiological mechanisms is NOT responsible for injury in peptic ulcer disease?
- Reflux of acid into the esophageal mucosa
- Mucosal damage due to Helicobacter pylori and NSAIDs
- Loss of blood supply to the mucosa
- Increased acid production
- Inhibition of prostaglandins
A 35-year-old man who is an alcoholic presents to the emergency department with severe epigastric pain, nausea, and vomiting. His blood pressure is 90/70 mm Hg. He begins receiving intravenous fluids and supportive treatment. After his condition is stabilized, he states that he was diagnosed with peptic ulcer disease 6 months ago. An endoscopy reveals a bleeding ulcer in the posterior wall of the proximal duodenum. Which of the following is the MOST likely cause of his symptoms?
- Rupture of the gastroduodenal artery
- Peri-pyloric scar formation
- Malignancy
- Rupture of the splenic artery
- Pancreatic bleeding
A 55-year-old man with a history of myocardial infarction and atrial fibrillation presents to the clinic for a refill of cimetidine for his peptic ulcer disease. He is compliant with his medications even though he complains of intermittent epigastric pain, which subsides after meals. A week later, he is seen in the emergency department for a nosebleed as well as bleeding in his stools. What is the MOST likely cause?
- Warfarin toxicity due to inhibition of cytochrome P450 by cimetidine
- Toxicity of the antacids
- Mucosal ischemia due to previous MI
- Interaction with proton pump inhibitors
- Interaction with sucralfate
A 45-year-old woman presents with a loss of appetite and fatigue. She has lost a significant amount of weight in the past 4–to 6 months. Her blood workup shows iron-deficiency anemia. She has a prolonged history of peptic ulcer disease. What is the MOST likely diagnosis for this patient?
- Malignancy due to gastric ulcer disease
- Perforated duodenal ulcer
- Gastroesophageal reflux disease
- Inflammation of the colon
- Esophagitis
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
great tutor, very informative and direct to the point helped a lot
1 customer review without text
1 user review without text