Playlist
Show Playlist
Hide Playlist
Peptic Ulcer Disease
-
Slides GIP Peptic Ulcer Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
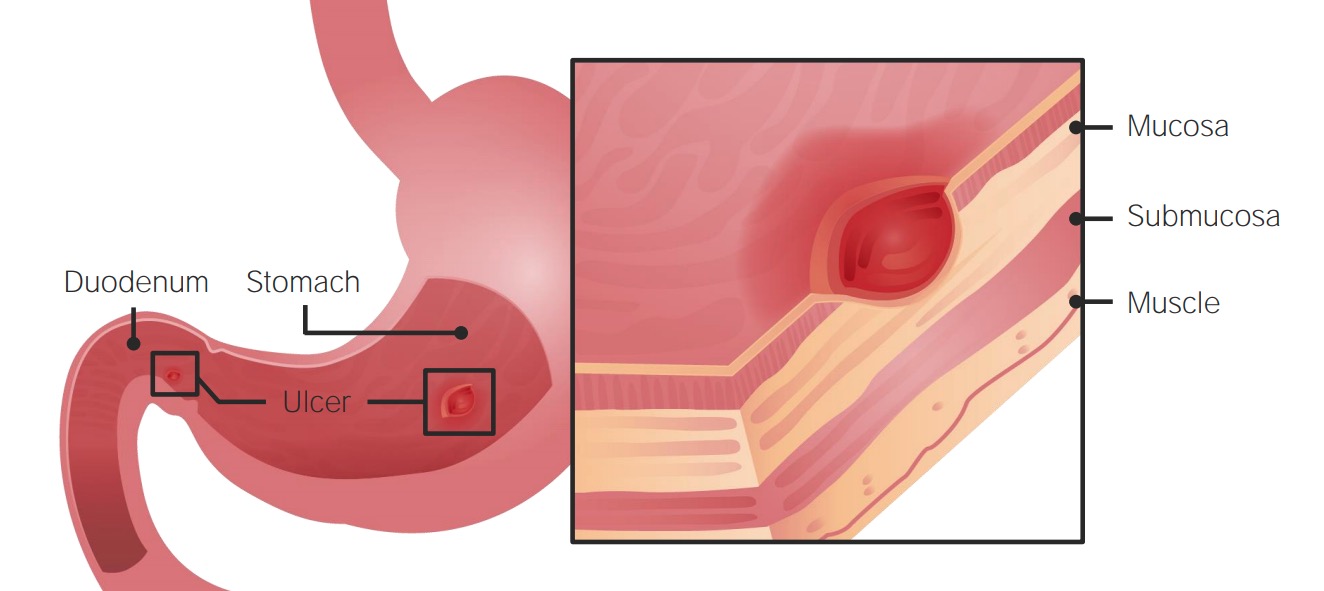
00:01 Welcome. 00:02 In this talk, we're going to cover peptic ulcer disease. 00:06 And when we talk about peptic ulcer disease. 00:08 it doesn't mean just in the stomach. 00:10 In fact, the majority of ulcers are going to occur down in the duodenum, but a certain percentage do occur in the stomach and we lump them all together. 00:20 So what is peptic ulcer disease? It's that annoying feeling you get in the pit of your stomach. 00:24 It's a mucosal defect. 00:26 In fact, that's all an ulcer is anywhere, it is the loss of the surface epithelium. 00:31 In this case, and either the stomach or the duodenum, it's a mucosal defect in the wall that leads to then bleeding, inflammation, pain. 00:43 I've already intimated that there are different locations for the typical peptic ulcer disease. 00:49 So the majority of these will tend to be in the first portion of the duodenum in the duodenal bulb. 00:56 And that's actually where you have the majority of gastric acidity, dumping on to the next unsuspecting part of the bowel. 01:03 And so that's going to be a major cause for lesions in that particular area. 01:08 The other site that we will see peptic ulcer disease are gastric ulcers, and these are typically occur in the lesser curvature of the stomach. 01:19 Epidemiology. 01:21 Men and women are equally affected in general. 01:27 Duodenal ulcers, as I've already indicated, occur much more frequently been gastric ulcers about 3:1. 01:33 And they typically occur earlier gastric ulcers, when they do occur will tend to be in older individuals. 01:41 The pathophysiology here. 01:43 So there are long laundry list of things that can cause peptic ulcer disease. 01:49 I think number one on the hit parade, number one on the list there, infection. 01:53 And Helicobacter pylori is going to be a major cause. 01:58 Drugs however, can also be a very close second, and nonsteroidal anti-inflammatory agents, such as aspirin, or any of the common nonsteroidal agents will cause effects as we will see on the microvasculature. 02:16 So you don't get good perfusion and it ends up being essentially an ischemic gastritis or an ischemic duodenitis that leads to ulceration. 02:25 Alcohol and smoking are very important causes peptic ulcer disease and hormonal stimulation. 02:33 So this isn't estrogen, this is not testosterone. 02:37 This is things like gastrin and too much gastrin will cause increased gastric acid production. 02:44 Ischemia, if we don't have good blood flow to the epithelium in the stomach or duodenum, we don't have good protective production of mucus. 02:54 And that mucus loss is going to give rise to peptic ulcer disease as the gastric acidity erodes, basically burns through the epithelium. 03:03 Chronic Disease, probably largely through ischemic mechanisms, but other forms of kind of inflammation can cause peptic ulcer disease. 03:14 And for you medical students out there, stress is a common cause probably associated with the increased production of glucocorticoids. 03:25 So I've already indicated that infections are probably your number one bad actor in terms of causing peptic ulcer disease. 03:32 And in fact, 80 to 90% of duodenal ulcers and 70 to 80% of gastric ulcers can be caused or attributed to Helicobacter pylori. 03:42 Other infections can do this as well. 03:44 So if you have watched the gastritis video previously, you also know that certain viruses like herpes simplex and Cyclo Megalo virus can also be causes for a gastritis can also be a cause of peptic ulcer disease. 03:59 Medications, remember that's number two on the list after infections. 04:03 Medications, such as nonsteroidal anti-inflammatory drugs are the most common bad actor. 04:08 So in the United States, naproxen, ibuprofen and aspirin are very common causes, and we'll get into why that is in a minute. 04:18 Bisphosphonates, typically used in the treatment of osteoporosis can also be a cause of gastritis or duodenitis or peptic ulcer disease, clopidogrel which is an anti-clotting agent. 04:37 Corticosteroids by affecting vascular supply, chemotherapies, rapamycin. 04:43 So there's a long list and this is only a partial list of drugs that could potentially cause peptic ulcer disease. 04:51 Alcohol and smoking in a minute are very important causes for inflammation, but they also cause loss of mucous production. 05:01 And alcohol specifically will cause a diminished mucus production one, but also will tend to dissolve whatever mucus is there so you lose the protective barrier and will lead to a chronic active gastritis. 05:16 In the setting of alcohol because we've also lost the mucus barrier, it's much easier for Helicobacter pylori to get a foothold. 05:25 Smoking will impact perfusion. 05:28 It will increase acid secretion, increases reactive oxygen species, and it suppresses angiogenesis. 05:36 All of those are going to lead us to a greater incidence of peptic ulcer disease. 05:42 Hormonal influences, we already talked about the fact that gastrin is going to be a very important driver of the production of gastric acidity. 05:50 And so Zollinger-Ellison syndrome where you have an actual gastrinoma, a little tumor, either in the pancreas or other locations in the body that produces too much gastrin. 06:02 You can also have antral G-cells, which are also a source of gastrin that can undergo hyperplasia and cause a gastritis. 06:12 If we are post-surgical, so if we've had gastric bypass where we are dumping contents of the stomach directly into the duodenum or small bowel, or if we've excluded the antrum, we are taking away a lot of mucus production. 06:32 In in that setting, we are dumping greater quantities of gastric acidity on mucosa that is not as well protected. 06:39 So post surgical patients will also be an increased risk for peptic ulcer disease. 06:46 Ischemia from any of a variety of causes, we have indicated here that cocaine. 06:50 Cocaine causes microvascular spasm. 06:52 So that can cause ischemia within the stomach and duodenum. 06:56 And the compensated chronic disease and there's a whole laundry list there, all of those in general will tend to cause diminished perfusion of important epithelium. 07:06 And importantly, in terms of the mucus production that gets diminished, and we lose our protection. 07:12 And finally, stress. 07:14 And stress with increased glucocorticoid production will tend to cause impact on the normal vasculature within the GI tract. 07:25 So getting back to kind of the yin and yang of gastric acidity wanting to eat into the mucosa and the mucus production by the mucosa fighting back, it's a balance. 07:39 So the defense that normally prevents the mucus from being eroded by hydrochloric acid is a mucous bicarbonate phospholipid layer, then you have an epithelial layer, and clearly everything is dependent on a good microvascular supply. 07:54 That's our defense. 07:58 If you have infection, if you have drugs that actually combat against your defense, so the Helicobacter pylori will increase gastric acid production. 08:10 It inhibits somatic statins, which also increases gastric acid production. 08:15 And you will also impact the integrity of the mucus, so you lose that barrier. 08:20 Already talked about nonsteroidal anti-inflammatory agents. 08:23 By the inhibition of the cyclooxygenase-1, we actually reduce prostaglandins which reduces the mucosal blood flow which means that the epithelium can't heal as well, and you don't produce as much mucus. 08:38 So, as we lose our barrier, as we lose our protective layer that will prevent the gastric acid from eating away at the mucosa we get now an ulcer. 08:51 The epithelium is destroyed and we have a loss not only are we losing the epithelium, but we're losing what the epithelium makes. 09:02 So we are losing mucus production, and it tends to be a bit of a reinforcing vicious cycle. 09:09 Here we have inflammatory cells as they come in, the neutrophils, the macrophages, the lymphocytes attracted to this area where we have tissue damage are also going to release cytokines inflammatory cytokines as well as reactive oxygen species which may also further exacerbate the underlying injury. 09:29 How does our patient present? I think you can probably tell me as well, as I'm going to tell you. 09:34 Interestingly, the majority of the patients, even with reasonably significant peptic ulcer disease are asymptomatic 70% or so. 09:44 They tend to be older adults. 09:46 They tend to be patients who are taking nonsteroidals. 09:48 So, that doesn't make sense. 09:50 Well, yes, it does. 09:51 Because they will not have pain sensation because of the effect of the nonsteroidal anti-inflammatory drugs. 09:58 So even though they're eroding their gastric mucosa or their duodenal mucosa, they don't sense any pain. 10:05 So nonsteroidals tends to be a very asymptomatic patient. 10:11 When we pick them up, we typically pick them up as bleeding, or tragically as a frank perforation where we have eroded all the way through all layers of the bowel, and you have a hole from the lumen into the peritoneum, and that may sometimes be your first clinical manifestation. 10:29 When patients are symptomatic, the pain is the symptom. 10:32 So you get classic pain, it's associated with eating usually 2-5 hours after that, that's when you have the most amount of gastric acidity hitting that area that is now had lost gastric or duodenal mucosa. 10:51 It is sometimes exacerbated by eating. 10:54 In classic cases, that's exactly the case but doesn't always have to be. 10:58 And it can happen just at night, when you also have a significant amount of gastric acidity but no food to dilute that, to neutralize that. 11:07 The pain is usually epigastric. 11:08 So just below the diaphragm midline, and it may radiate into both upper quadrants or either one. 11:16 Occasionally, we'll all go to the back and it tends to be described as a annoying sensation as if there's a big rat in there eating away at your stomach. 11:26 Other symptoms that may occur in patients who have peptic ulcer disease is nausea and vomiting. 11:32 Bathing the underlying submucosa may irritate nerves and cause a very thick sensation. 11:41 Patients because of inflammation may have edema. 11:44 And so there may be a compression of the lumen of the GI tract which will give a sense of early satiety. 11:53 Similarly, after you eat there may be a sense of fullness or bloating and frequently because of this partial obstruction and patients swallowing air, they will belch, or they will burp or irritation which is sounds like a nicer way to say it. 12:11 How do we diagnosis this? So, history in most cases will be the way that you make the diagnosis. 12:20 You review the common risk factors, so nonsteroidal anti-inflammatory agents. 12:24 Are you taking naproxen or ibuprofen? Are you using aspirin regularly? Well, how much alcohol do you drink? Do you smoke? Is there underlying chronic disease, chronic obstructive pulmonary disease, cirrhosis, etc? And has there been prior gastric surgery? So that you are now dumping gastric contents into other parts of the bowel directly. 12:45 Laboratory studies will look primarily for bleeding. 12:49 So you're going to be essentially looking for occult bleeding. 12:53 So you will look for blood in the stool and you will look for iron deficiency, not so much malabsorption but deficiency. 13:02 You may also, if you suspect that there is a Zollinger-Ellison type syndrome where you have too much gastrin production, you may measure gastrin levels. 13:11 And then, of course, you should do esophagogastroduodenoscopy. 13:17 Additional studies. 13:19 Of course, you should look and see if there are lesions specifically. 13:24 You can do this with esophagogastroduodenoscopy, which is probably going to be your most accurate diagnostic test, much more easily said is just an EGD. 13:34 The findings are that you'll find a gastric ulcer usually a solitary discreet mucosal lesion, usually on the lesser curvature of the stomach. 13:43 The benign lesions have a smooth, rounded edge. 13:46 If it's malignant, which can be a cause of peptic ulcer disease, it tends to be heaped up margins with a very irregular edge. 13:55 And it's typically as I said, in the lesser curvature. 13:59 As you do your EGD and get further beyond the pylorus into the duodenum, you will see small breaks in the mucosa and the duodenum. 14:07 And it's usually in the first part has the similar sort of smooth edge not heaped up and that there's a superficial erosion. 14:17 In terms of other causes, if you suspect or even if you don't, you should be assessing for the possibility that this is caused by Helicobacter pylori. 14:26 Because if that is the case, you're going to have to treat primarily to eradicate that infection. 14:31 So there are a variety of tests. 14:33 If you've looked at the gastritis talk, you already know what some of these are. 14:38 But if you're jumping in first to see peptic ulcer disease, this is what we do to look for Helicobacter pylori. 14:43 So noninvasively, we can look for antigen in the stool. 14:47 We can also do what's called a urea breath test and we basically give oral radioactive urea. 14:53 And then the urease produced by the Helicobacter pylori splits that liberate CO2 that's radio labeled and we can detect that in the breath. 15:02 And that's a very sensitive test. 15:04 Those two will tell you if you have a positive antigen test or a positive urea breath test, that means you have active infection. 15:11 You can also do Serologies. 15:13 So you can look for immunoglobulin G that indicates a past infection that will remain positive though even if you've cleared the infection. 15:22 So it's not as useful for documenting acute, ongoing Helicobacter. 15:28 Clearly, we would like to do a biopsy, make sure that there's nothing malignant in there. 15:34 And histology will also help in terms of confirming a diagnosis of Helicobacter pylori. 15:39 On histology, we can see with special stains particularly a silver stains, or a game sustain, that we have curved flagellated gram negative rods, and you can see them literally spread over the landscape. 15:53 It's pretty impressive. 15:54 We can also do bacterial culture, and sensitivity. 15:57 But in general, what we're going to do is give multiple antibiotics as we'll see in a moment. 16:03 Histology will allow us to identify if there's Helicobacter pylori, but it will also allow us to see whether or not there might be malignancy to proposed. 16:14 How are we going to manage this? Well, again, it's pretty straightforward. 16:18 We want to discontinue anything that's going to be causing the gastric ulcers so nonsteroidals, stop smoking, stop drinking, any drugs, cocaine, etc that might be causing an ischemic gastritis or ischemic duodenitis. 16:34 There's always been kind of in the literature, this notion that a bland diet will help you and stay away from the spicy food. 16:42 Control studies say that probably not necessary, but patients may feel like they're doing better on that diet. 16:50 So the psychological benefit in reducing stress may actually give you some improvement. 16:58 But, specifically, if we're thinking about Helicobacter pylori, we need to get rid of that. 17:04 And it's a combination of one proton pump inhibitors that has nothing to do with the Helicobacter but it reduces gastric acid. 17:11 But then we do a variety of antibiotics as you can see there. 17:14 And in quadruple therapy, we'll add bismuth, which is bactericidal for the Helicobacter. 17:22 It's uncommon that we have to do surgical intervention, but if you have a chronic non-healing ulcer, you may have to excise that or otherwise try to improve vascular supply to that area. 17:36 And with that, hopefully you haven't developed ulcers while listening to me talk about this. 17:42 But we've now covered everything there has to do with peptic ulcer disease.
About the Lecture
The lecture Peptic Ulcer Disease by Richard Mitchell, MD, PhD is from the course Disorders of the Stomach.
Included Quiz Questions
What is peptic ulcer disease?
- Mucosal defect in the wall of the stomach or duodenum
- Muscular defect in the wall of the stomach or duodenum
- Muscular outgrowth in the wall of the stomach or duodenum
- Mucosal outgrowth in the wall of the stomach or duodenum
- Mucosal outgrowth in the wall of the duodenum or jejunum
What is the typical location of a gastric ulcer?
- Lesser curvature of the stomach
- Greater curvature of the stomach
- Antrum
- Pylorus
- Cardia
What is the most common cause of peptic ulcer disease?
- Infection
- NSAIDs
- Alcohol
- Smoking
- Ischemia
Which of the following describes one step of the pathophysiology of alcohol-induced peptic ulcer disease?
- Reduced mucosal barrier
- Antibacterial modification
- Decreased perfusion
- Decreased acid secretion
- Decreased reactive oxygen species production
What is the most common presentation of peptic ulcer disease?
- Asymptomatic disease
- Dyspepsia
- Nausea
- Hematemesis
- Dizziness
What is the classic presentation of a duodenal ulcer?
- Pain 2–5 hours after eating and at night
- Pain 12 hours after eating fatty food
- Pain immediately after eating and in the morning
- Constant pain
- Waxing and waning pain unrelated to food intake
What is NOT a typical symptom of peptic ulcer disease?
- Dizziness
- Nausea
- Pain
- Early satiety
- Fullness
What study should be ordered if there is suspicion of Zollinger-Ellison syndrome?
- Fasting gastrin level
- CBC
- CMP
- Octreotide level
- Cortisol level
What is the most accurate diagnostic test for peptic ulcer disease?
- EGD
- CBC
- EUS
- EEG
- Gastrin level
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
16 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
16 customer reviews without text
16 user review without text