Playlist
Show Playlist
Hide Playlist
Obstructive Sleep Apnea – Secondary Hypertension
-
Slides Secondary Hypertension.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
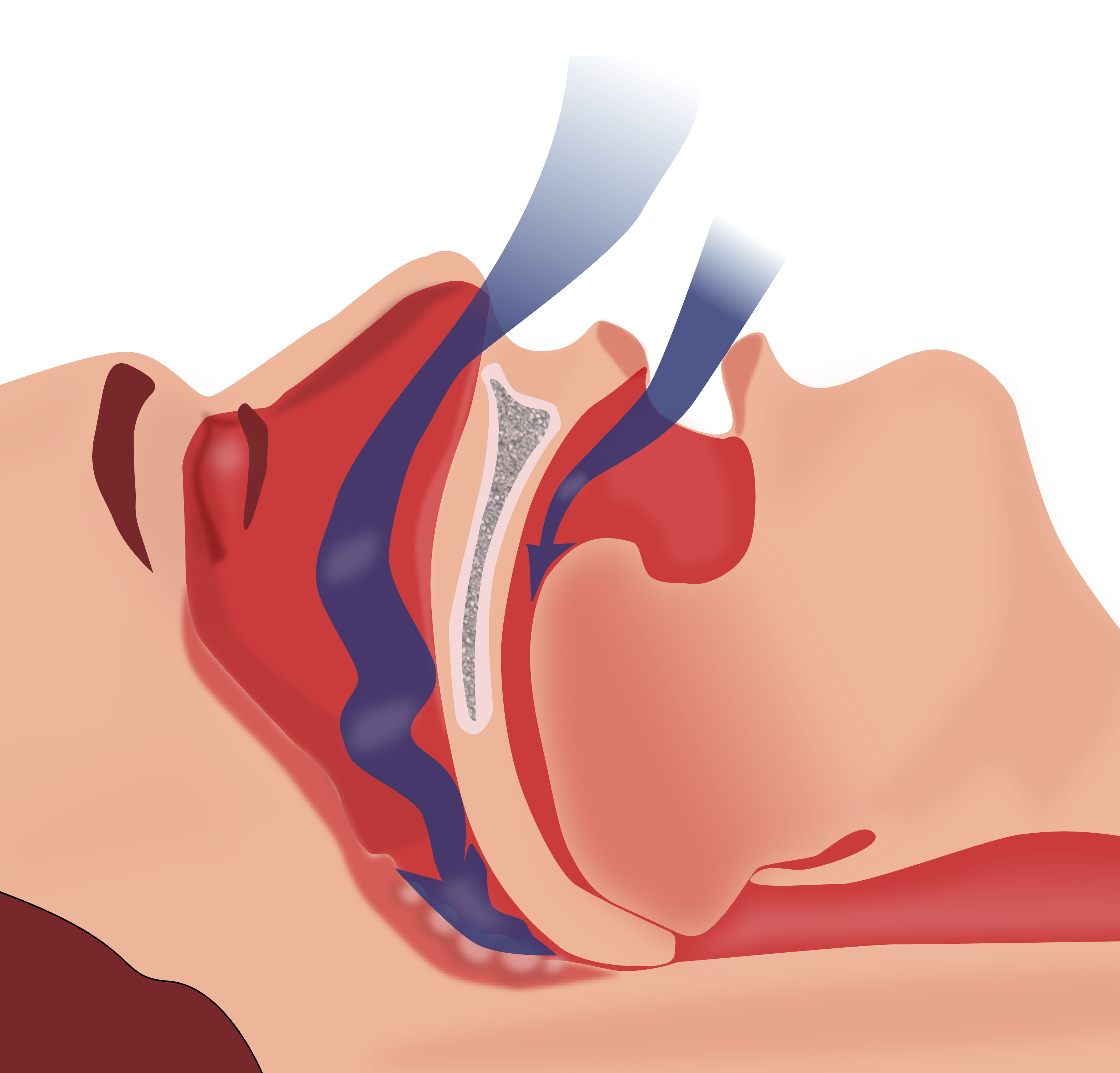
00:01 So, obstructive sleep apnea is defined by obstructive apneas, meaning that people are not breathing, hypopnea, so abnormal reduction of airflow, or respiratory effort-related arousals during sleep. 00:14 Patients will complain of daytime sleepiness, fatigue, poor concentration. 00:19 They have signs of disturbed sleeping, including snoring, restlessness, or resuscitative snorts. 00:26 The pathophysiology behind obstructive sleep apnea is interesting. 00:33 There's a well-documented association of obesity, obstructive sleep apnea, and hypertension. 00:38 The apneic syndrome itself is presumed to contribute directly to hypertension and abnormalities in the sympathetic nervous function and vascular reactivity is probably one of the culprits. 00:49 The clinical features of OSA, about 30-80% of patients with primary hypertension actually have obstructive sleep apnea and 50% of patients with OSA have hypertension. 01:03 The manifestations are what we talked about. 01:06 Daytime hypersomnolence, these people are very tired during the day, they can actually fall asleep very easily after eating a meal or even when they're driving at a stop light, which is actually quite scary for a lot of patients. 01:18 They complain of morning headache when they wake up in the morning because of restless sleep. 01:23 Snoring, witnessed apneic episodes, or poor concentration. 01:28 The diagnosis, gold standard, polysomnography, which is a sleep study. 01:33 That's able to detect apneas, hypopneas, and respiratory effort arousals. 01:38 So, once we've diagnosed our patients with obstructive sleep apnea, how do we treat them? We do a lot of lifestyle intervention. 01:46 We want those patients to really think about weight loss, avoidance of alcohol and sedating medications like benzodiazepines, antihistamines like Benadryl, those depress the central nervous system and exacerbates sleep apnea. 01:59 We can do interventions like continuous positive airway pressure or CPAP which is shown here to the right in this gentleman. 02:06 This will splint the upper airway open and prevents upper airway collapse or narrowing during sleep. 02:13 If our patients are unable to tolerate CPAP and many of them are, then you can use something like an oral appliance or mandibular advancement splint and this is designed to protrude the mandible forward and hold the tongue in a more anterior position. 02:28 Finally, there are surgical therapies available, they're definitely second-line, and they're not used as much, but something like a uvulopalatopharyngoplasty or a UPPP is really reserved for those patients who have a surgically correctable or obstructive lesion. 02:47 The degree of benefit is probably variable and a cure is rare. 02:51 So, with that, I hope that you've learned some of the important causes of secondary hypertension and I want you to remember to look for those clues because diagnosing this and treating these patients cannot only be life-saving, it also affords your patients a better quality of life. 03:07 And with that, we conclude our secondary hypertension talk.
About the Lecture
The lecture Obstructive Sleep Apnea – Secondary Hypertension by Amy Sussman, MD is from the course Secondary Hypertension.
Included Quiz Questions
Which of the following statements is true?
- Polysomnography is the gold standard test for obstructive sleep apnea.
- Obstructive sleep apnea is not an independent risk factor for hypertension.
- Obstructive sleep apnea can cause hypertension through parasympathetic stimulation.
- An early clinical manifestation of obstructive sleep apnea is daytime hypoxemia.
Which of the following is true regarding the management of obstructive sleep apnea (OSA)?
- CPAP prevents upper airway collapse during sleep.
- Surgical intervention is the first-line treatment for OSA.
- Patients with OSA should take sedating agents to help them sleep at night.
- Lifestyle modifications have not shown any improvement in the treatment of patients with OSA.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |