Playlist
Show Playlist
Hide Playlist
Nonalcoholic Fatty Liver Disease
-
Slides GIP Nonalcoholic Fatty Liver Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
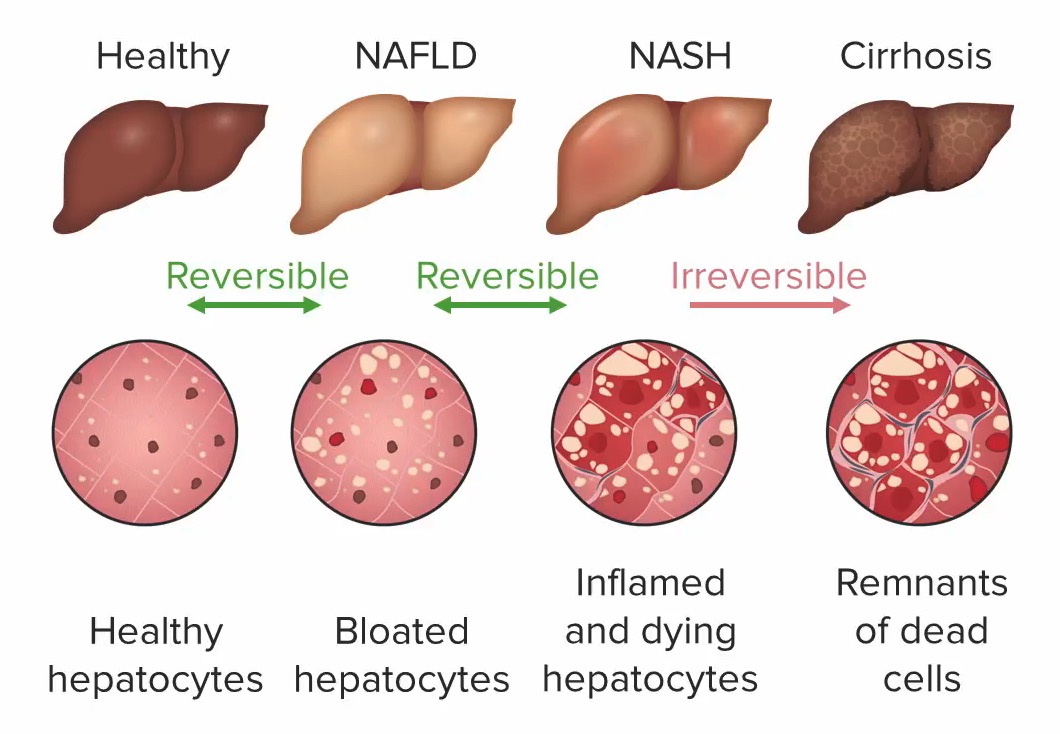
00:02 Welcome! In this talk, we're going to be covering Nonalcoholic Fatty Liver Disease. 00:07 What is this? So NAFLD or Nonalcoholic Fatty Liver Disease is chronic liver pathology that's associated specifically with obesity and also with hepatic steatosis. 00:18 And it may or may not have associated inflammation and fibrosis. 00:22 It's essentially got many of the same mechanisms and much of the same appearance as alcohol associated liver disease, just without the alcohol. 00:33 The types of non alcoholic fatty liver disease. 00:35 So you can have just non alcoholic fatty liver, this is just hepatic steatosis and there's no inflammation. 00:42 You can also have non alcoholic steatohepatitis, easier to abbreviate that as NASH, which is steatosis. 00:50 But there's lobular inflammation, degenerating hepatocytes and lots of accumulated, a both acute and chronic inflammatory cells. 01:00 The epidemiology. 01:03 This is now in the United States the most common cause of chronic liver disease, it exceeds alcohol, and it exceeds hepatitis due to viral injury. 01:14 It affects up to 25% of adults and it's increasing as the obesity epidemic kind of expands, no pun intended, to the adult population in many industrialized nations. 01:28 Patients are usually affected in their 40s and 50s. 01:30 So this is after a period of time with obesity. 01:33 It doesn't happen instantaneously in their 20s and 30s when they become fat. 01:38 But later on, after a couple of decades of persistent accumulation of extra cholesterol and lipids. 01:48 It can also lead to cirrhosis. 01:50 So in the same way that alcoholic liver disease can progress through alcoholic steatohepatitis and then eventually to cirrhosis so too can occur in non alcoholic fatty liver disease and the incidence of fat of liver cancer is up to 3% when cirrhosis does develop. 02:10 Risk factors for this overall. 02:12 So metabolic syndrome and you may recall the metabolic syndrome involves insulin resistance, central obesity with a large abdominal girth, hypercholesterolemia, and hypertension. 02:27 Other associated risk factors even if the patient doesn't have insulin resistance, etc, just central obesity puts them at increased risk for non alcoholic fatty liver disease. 02:37 Type 2 diabetes, probably as a marker for obesity and insulin resistance is also a risk factor as is hypertension and hypertriglyceridemia. 02:46 Other risk factors, so rapid weight gain, okay, that kind of makes sense. 02:51 You're just pouring on the calories and you have increased fat content, but also rapid weight loss by mobilizing fat and proteins from the periphery and mobilizing and sending them to the liver may also give rise to non alcoholic fatty liver disease. 03:09 Hypothyroidism by changing metabolic rates may be a risk factor. 03:14 Certainly polycystic ovarian syndrome is also associated with, although the mechanisms overlapping between obesity and polycystic ovarian syndrome. 03:25 And then some of the endocrine derangements that lead to PCOD, Polycystic Ovarian disease are a little bit complex. 03:34 Some of the other endocrinopathies. 03:36 So Cushing syndrome with an elevated ACTH leading to elevated glucocorticoids and then medications. 03:43 Amiodarone is known to cause non alcoholic fatty liver disease, glucocorticoids, doxycycline and there are a host of others. 03:52 The pathophysiology here. 03:54 Again, this is very similar to what is happening overall associated with alcohol and the metabolism of alcohol except in this case, it is increased oxidative stress due to the increased chronic metabolism of free fatty acids. 04:11 In metabolizing free fatty acids, in the setting of obesity and type two diabetes and other things, we are creating increased amounts of reactive oxygen species, and those in particular drive an oxidative stress that will in turn, induce lymphocyte and kupffer cells, macrophages within the liver, to increase their production inflammatory mediators that increased triglyceride metabolism also leads to lipid toxicity. 04:40 So as we're metabolizing a whole bunch of triglycerides, we may not efficiently get down to two carbon acetate subunits, but in fact, we may have intermediates that are also potentially lipotoxic. 04:54 When that occurs, the poor hepatocytes respond by not metabolizing lipid appropriately. 05:01 And they accumulate it. 05:02 So that's recognized the steatosis are non alcoholic fatty liver, and with recurrent injury, or recurrent bouts of this or just chronic obesity and chronic steatosis. 05:15 You may eventually get such degree of lipotoxicity and activation of kupffer cells and lymphocytes that you now get NASH, steatohepatitis, and with prolonged NASH that can then lead into cirrhosis. 05:31 And as we've already seen, cirrhosis over time may develop into hepatocellular carcinoma. 05:36 So that's kind of the pathway. 05:38 So the progression from a healthy liver to a liver, the past cirrhosis or even hepatocellular carcinoma is as indicated here. 05:48 With the lipotoxicity, the reactive oxygen species, the accumulation of fat, we can get steatosis, that's completely reversible. 05:55 And if we lose weight, if we reduce the oxygen toxicity associated with reactive oxygen species, we're good to go. 06:04 With persistence steatosis, we may activate lymphocytes and macrophages. 06:10 So we did get a degree of inflammation or steatohepatitis. 06:15 That's also incredibly reversible and we can get back to even a healthy liver. 06:21 However, once we progress to fibrosis, through the activity, through the activation of stellate cells, who are driven by inflammatory mediators, once we have that cirrhosis, then that's in stage and we can't ever revert. 06:38 And in that setting, as we've already talked about, there is an increased risk for the development of hepatocellular carcinoma. 06:46 How does the patient present? So with early steatosis, the patient is often quite asymptomatic, there may be subtle levels of fatigue and malaise. 06:56 There may be a little bit of right upper quadrant discomfort, that's because as the liver expands with fat, it will stretch glistens capsule and that will lead to some sensation of discomfort. 07:08 There will be hepatomegaly, you can formally feel the liver edge below the right costal margin, indicating that the liver is enlarged. 07:16 And with more progressive disease, we may see elements or symptoms related to cirrhosis. 07:25 I would refer you back to other talks within this Lecturio series to see what cirrhosis presents with. 07:33 How are we going to make the diagnosis? Liver biopsy is probably the gold standard but is not usually performed. 07:41 If the diagnosis is unclear, if there might be other etiologies for fatty liver disease or for hepatitis or even cirrhosis, we may do that. 07:52 The biopsy will help us to distinguish whether we just have fatty liver disease with accumulation of fat, or whether we've progressed on to hepatosis with NASH. 08:02 An ultrasound will often give us some of that same information and is non invasive, and a very echogenic liver indicates that there's lots and lots of fat that is reflecting the ultrasound waves. 08:13 And on the image that you're seeing here, the normal renal parenchyma is indicated on the right hand side. 08:20 That darker color should be what the liver looks like. 08:23 And here's a liver is looking much wider, indicating greater fat content. 08:28 Laboratory tests can be somewhat confirmatory, they're not going to be absolutely diagnostic. 08:34 So you may see elevated Aspartate Aminotransferase, AST, or elevated Alanine Aminotransferase or ALT, but they may also be normal, particularly if there is no steatohepatitis. 08:48 There will certainly be elevated triglycerides and cholesterol but this is actually part and parcel of the primary process. 08:54 These patients are obese. 08:56 So their serum triglycerides and cholesterol are usually elevated just on that basis, whether they have liver disease or not. 09:04 We do want to rule out other causes of chronic hepatitis. 09:08 So we want to make sure that this isn't due to alcoholism. 09:11 And we do that with history and some of the biomarkers and I would refer you to the talk in this series about alcoholic liver disease. 09:20 We want to make sure it's not viral hepatitis because we have some therapies for that, particularly viral hepatitis C. 09:26 Wilson's disease or hemochromatosis due to either copper or iron overload respectively, on autoimmune hepatitis, so we want to rule those out. 09:35 This is just an example of what things would look like histologically on biopsy. 09:39 On the left hand side is mostly steatosis. 09:43 We have enlarged hepatocytes with nuclei out to the periphery and a massive expansion with intracellular triglycerides. 09:52 It's basically a big bubble of fat that is reversible. 09:56 On the right hand side, we are seeing hepatocytes with triglyceride accumulation, but now we see a lot of little blue cells in between. 10:06 That's the hepatitis. 10:07 So we have steatohepatitis. 10:10 And stage we will get cirrhosis. 10:12 And again, I refer you to those talks on cirrhosis in this series. 10:18 How are we going to manage it? So easier said than done, tell your patient to lose weight, help them with that, be supportive. 10:26 But it can be very difficult. 10:28 You want to control a lot of the comorbidities. 10:31 So if diabetes is associated with their metabolic syndrome, that's leading to this, we want to control that with insulin, or other agents that are going to help them control and give them good glucose blood control. 10:45 We want to avoid other toxicities, we don't want to exacerbate what is already going on due to the lipotoxicity and the reactive oxygen species. 10:53 So avoid alcohol, avoid smoking, avoid other things that can injure the liver. 11:01 We want to make sure that they're immunized and up to date so that they don't get hepatitis. 11:05 And if they do have hepatitis, such as hepatitis C, we want to be sure that we treat that quickly and effectively. 11:12 For non alcoholic fatty liver disease, so just steatosis and this steatohepatitis, there is no specific pharmacologic therapy, we just do the things that are at the top part of this slide. 11:26 And for end stage disease, where the patient has developed cirrhosis, but is driven to lose weight and otherwise maintain good glycemic control, etc. 11:39 Then liver transplantation can be considered. 11:42 With that, non alcoholic fatty liver disease
About the Lecture
The lecture Nonalcoholic Fatty Liver Disease by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What is the most accurate definition of NAFLD?
- Chronic liver disease associated with obesity and hepatic steatosis with or without inflammation and fibrosis
- Acute liver disease associated with obesity and hepatic steatosis with or without inflammation and fibrosis
- Chronic liver disease associated with anemia and hepatic steatosis with or without inflammation and fibrosis
- Chronic liver disease associated with obesity and hepatic steatosis without inflammation
- Chronic liver disease associated with obesity and hepatic steatosis without fibrosis
What is the prevalence of nonalcoholic fatty liver disease?
- 25% of adults
- 50% of adults
- 25% of children
- 50% of children
- 50% of the entire population
What are the risk factors for nonalcoholic fatty liver disease? Select all that apply.
- Metabolic syndrome
- Central obesity
- Type II diabetes
- Hypotriglyceridemia
- Type 1 diabetes
Which of the following explains the pathophysiology of nonalcoholic fatty liver disease?
- Increased free fatty acids
- Decreased reactive oxidative species
- Decreased triglycerides
- Hypertrophy
- Reed-Sternberg cells
What test best distinguishes NAFLD from NASH?
- Liver biopsy
- Ultrasound
- CT abdomen
- AST
- Bilirubin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |