Playlist
Show Playlist
Hide Playlist
Neuropathic Pain: Locating a Lesion in the PNS
-
Slides Neuropathic Pain Syndromes.pdf
-
Download Lecture Overview
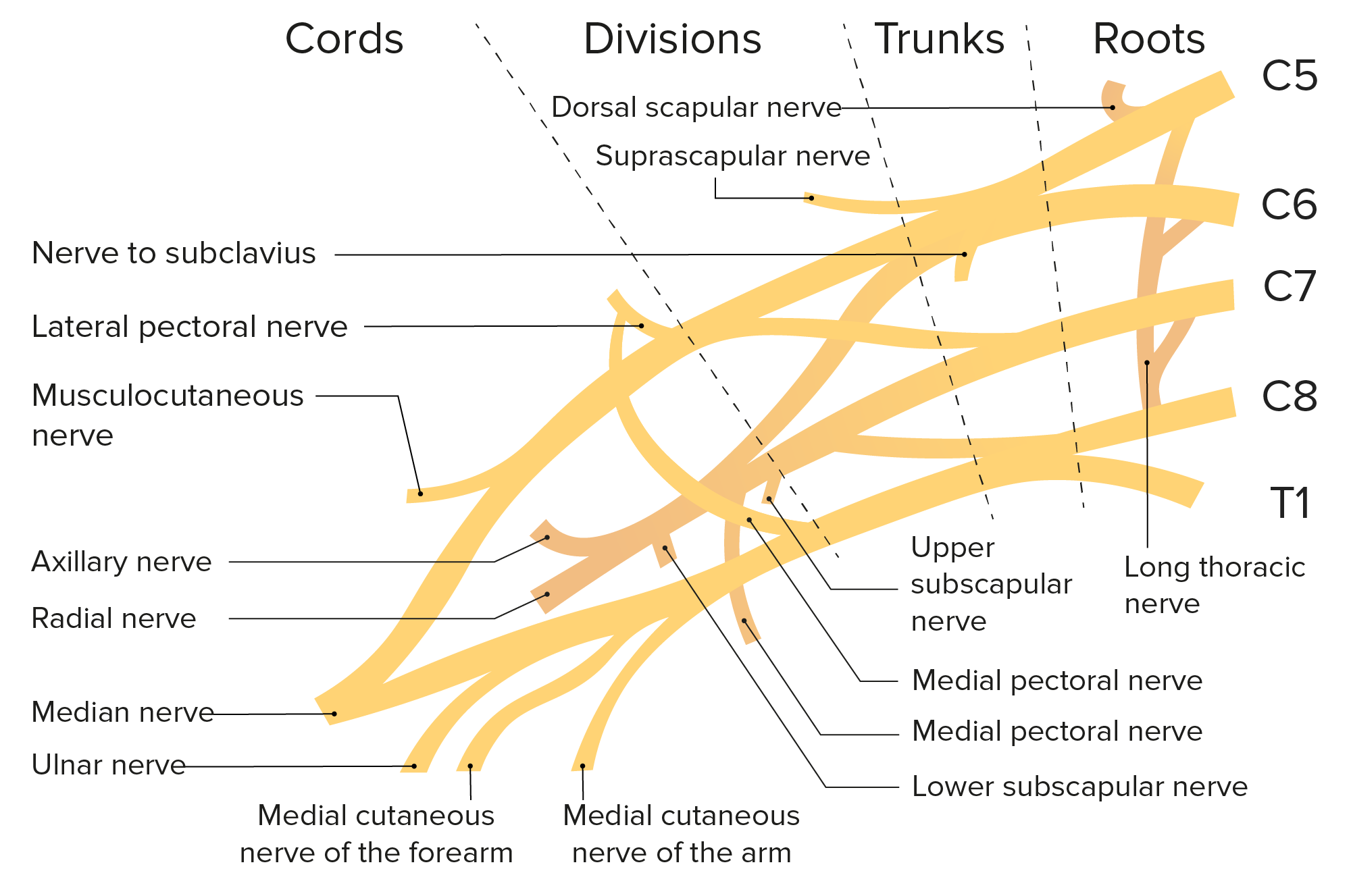
00:01 Now let's talk about Step 2. 00:03 If the problems in the peripheral nervous system, where is it? And first let's go back to our anatomy of the peripheral nervous system. 00:12 The peripheral nerve starts in the central nervous system next to the spinal cord, exits through dorsal and ventral roots to form the peripheral nerves. 00:21 The cell bodies of those sensory nerves lie in the dorsal root ganglion. 00:25 And we have pre-ganglionic portions of the sensory nerves and post-ganglionic portions of the sensory nerve. 00:32 Here pathology at the nerve root at the nerve Plexus or out in the terminal nerve branches can contribute to neuropathic pain. 00:40 Radiculopathy and nerve root problem can present with neuropathic pain and diabetic polyneuropathy problems originating in the terminal nerve branches can present with prominent neuropathic pain. 00:52 When we think about the peripheral nervous system, we want to start by thinking about the type of nerve that's involved, the size of the fiber that may have dysfunction, and the clinical description. 01:03 There are number of different types of neuropathies we can see. 01:05 We can see motor neuropathies, problems with those large myelinated A alpha nerves and patients will describe weakness. 01:14 We can also see sensory neuropathies where neuropathic pain is a very common symptom. 01:19 Sensory neuropathies may affect a large myelinated sensory nerves and present with symptoms of decreased touch, reduced vibration or problems with proprioception. 01:29 We may also see small fiber neuropathies. 01:31 And pain, neuropathic pain is the most common in a scene in small fiber neuropathies. 01:37 Small fiber neuropathies caused problems with those unmyelinated or thinly myelinated sensory nerves and we see symptoms of problems with pain or temperature or light touch. 01:48 And then autonomic neuropathies can also present variably with neuropathic pain. 01:53 Autonomic fibres include both the thinly myelinated and unmyelinated C fibers and may present with various autonomic dysfunction, problems with heat or cold, orthostatic hypotension from abnormal blood pressure or constipation from autonomic control of gut function. 02:12 When we localize to the peripheral nerve, we can localize using the type of nerve that's involved. 02:16 We can localize to sensory neuropathies or motor neuropathies or autonomic neuropathies and understand whether the neuropathic pain is in the setting of a certain type of neuropathy. 02:26 We can localize to the fiber type. 02:29 There are large fiber neuropathies where neuropathic pain may be seen and present with numbness and small fiber neuropathies where pain and neuropathic pain and paraesthesias are more common. 02:39 And then we can localize to the section of the nerve that's involved. 02:42 There is axonal neuropathies and demyelinating neuropathies and neuropathic pain can be seen with both.
About the Lecture
The lecture Neuropathic Pain: Locating a Lesion in the PNS by Roy Strowd, MD is from the course Neuropathic Pain Syndromes.
Included Quiz Questions
Pathology at what location(s) can contribute to neuropathic pain?
- Terminal nerve branches
- Preganglionic portions of sensory nerves
- Spinal cord
- Ventral nerve roots
- Thalamus
How might a small fiber neuropathy present clinically?
- Neuropathic pain
- Decreased vibration and proprioception sense
- Motor weakness
- Orthostatic hypotension
- Sweating and diarrhea
How might an autonomic neuropathy present?
- Constipation
- Foot pain
- Crampy abdominal pain
- Confusion
- Sweating and diarrhea
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |