Playlist
Show Playlist
Hide Playlist
Neurofibromatosis Type 2: Diagnosing Criteria
-
Strowd CNS Tumors Inherited Tumor Syndromes.pdf
-
Download Lecture Overview
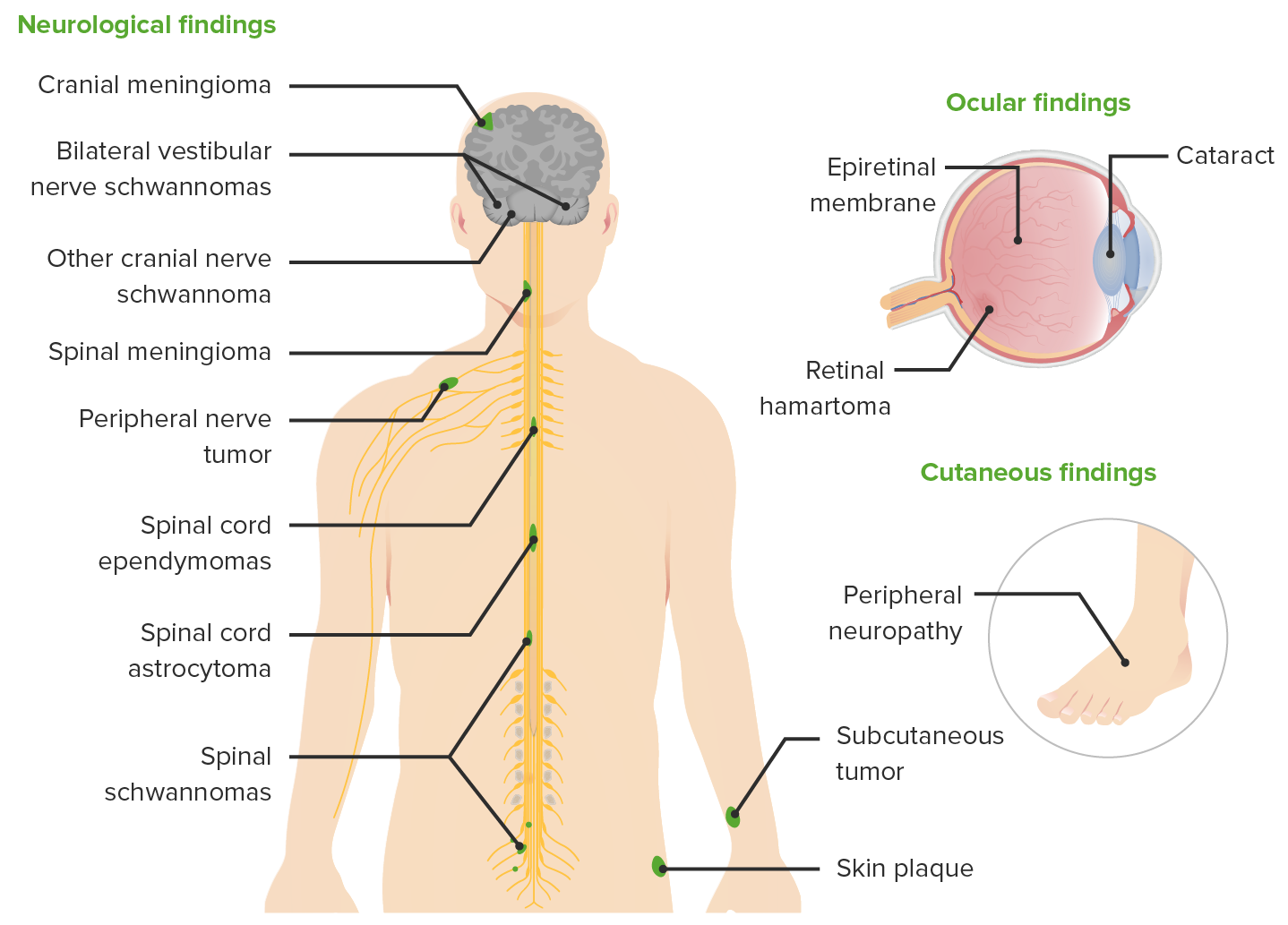
00:00 How do we diagnose NF2? Well, it is a genetic condition. 00:04 But like NF1, we often don't do genetic testing. 00:08 It can be helpful and it's done in certain circumstances, but the vast majority of patients with NF2 are diagnosed clinically, based on these criteria. 00:17 The most common clinical criteria to establish a diagnosis of NF2 is the presence of bilateral vestibular schwannomas, just like in our case. 00:26 That should be present by the age of 30. 00:29 And typically, patients with NF2 will have their tumors by 30, and you should see them at that time. 00:35 So a patient who does not have bilateral vestibular schwannomas on MRI imaging by the age of 30, likely does not have or will develop NF2. 00:45 There are other clinical criteria that can be met to establish this diagnosis. 00:49 The presence of a family history of NF2, and a unilateral vestibular schwannoma is sufficient to make the diagnosis. 00:55 The presence of a family history and two other characteristics of NF2, two other characteristic tumors like meningiomas, ependymomas, peripheral nerve schwannomas, gliomas, or this juvenile posterior subcapsular cataract are also consistent with a diagnosis of NF2. 01:14 And then there are some other ways to make this diagnosis a unilateral vestibular schwannoma and two other characteristic tumors, which you can see there, and multiple meningiomas, as well as two other characteristic tumors. 01:25 The point is, it's not just one tumor, because meningiomas and vestibular schwannomas are amongst the four most common benign tumors, brain tumors, that we see. 01:35 These patients have multiple tumors. 01:37 And that raises the suspicion that they're not sporadically acquired, but inherently gained. 01:46 What are some other features that we see in these patients? Well, it's not just tumors. We can see cutaneous lesions. 01:52 And 70% of patients with cutaneous lesions may be a bit high, but if you look, you may find them. 01:58 Neurofibromas can occur but are much less common than in patients with NF1. 02:03 And typically the tumors that we see are schwannomas. 02:06 Neuropathy is common in these patients, and we see both a generalized polyneuropathy that's usually pretty mild and only present on exam, not subjectively reported by patients, as well as manoneuropathies. 02:18 Things like Bell's Palsy or other single nerve dysfunction syndromes. 02:23 Seizures can occur but are rare. 02:25 Intracranial hypertension, too much intracranial pressure is also rare, but can occur particularly in patients with multiple meningiomas. 02:34 And then we can see cranial neuropathies from compression of a tumor or other causes. 02:38 And that can contribute to hearing loss, facial nerve dysfunction like a Bell's Palsy, dysphasia, balance dysfunction, or vagal nerve dysfunction. 02:47 Again, a lot of neurologic symptoms that can be seen in these patients. 02:51 Many of those which are of central nervous system origin.
About the Lecture
The lecture Neurofibromatosis Type 2: Diagnosing Criteria by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Which of the following is sufficient to make a diagnosis of neurofibromatosis type 2?
- 1st-degree relative with NF2 + ependymoma + glioma
- Bilateral vestibular schwannoma by age 40 on imaging
- 1st-degree relative with NF2 + spinal schwannoma
- Unilateral vestibular schwannomas + meningioma
- Juvenile posterior subscapular cataract + peripheral schwannoma
Which of the following is an additional finding that might be seen in neurofibromatosis type 2?
- Neuropathy
- Raised intraocular pressure
- Anterograde amnesia
- Hallucinations
- Impaired executive function
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |