Playlist
Show Playlist
Hide Playlist
Neurofibromatosis Type 2: Clinical Presentation
-
Strowd CNS Tumors Inherited Tumor Syndromes.pdf
-
Download Lecture Overview
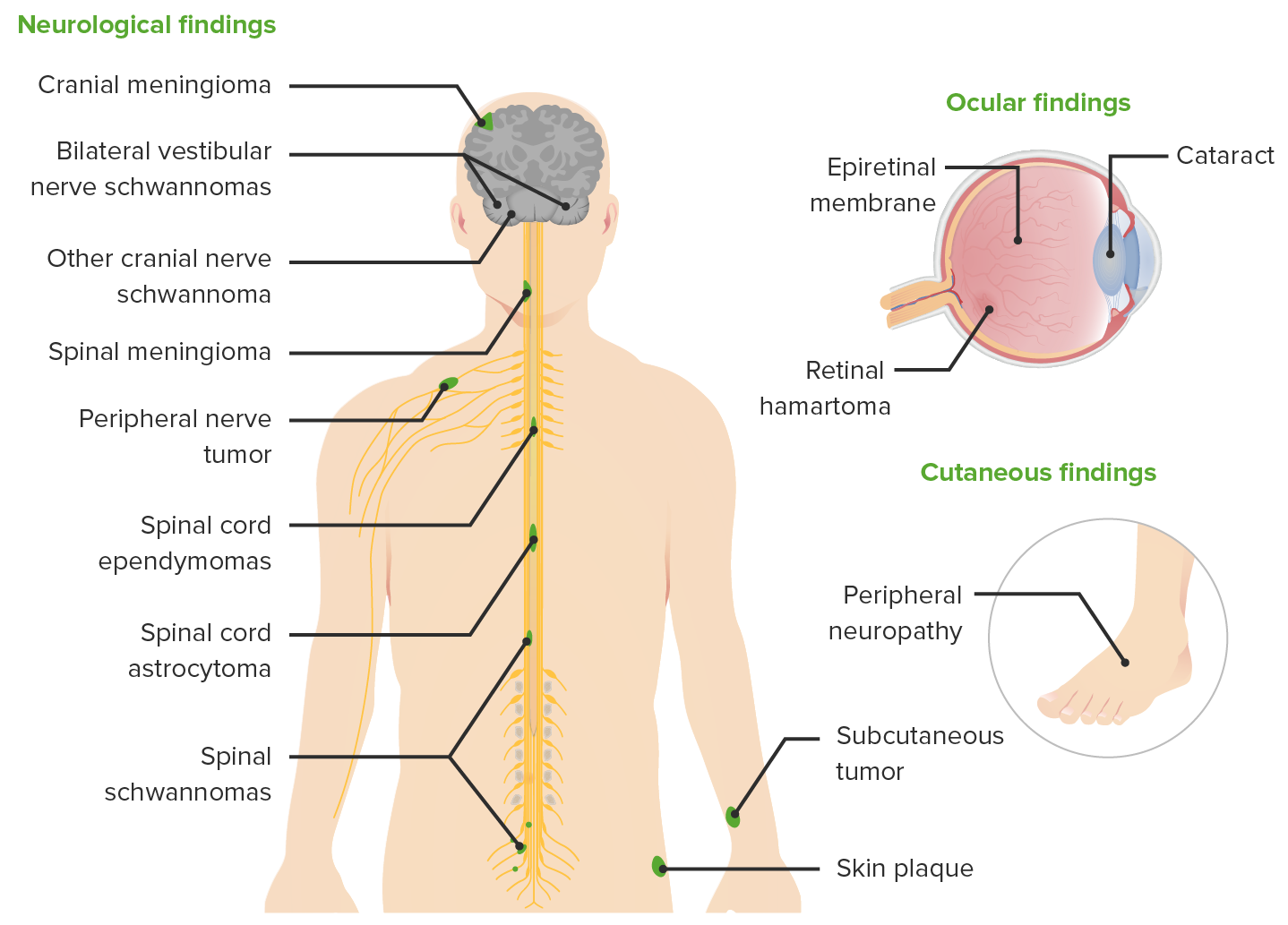
00:01 So let's talk a little bit more about the key manifestations of NF2. 00:04 And the things I want you to know about are vestibular schwannomas, intracranial meningiomas, and spinal ependymomas. 00:12 You need to know that those are associated with NF2. 00:15 And when you see a patient or a vignette, with those three tumor types, the first thing you should think of is NF2. 00:21 We'll also think about spinal schwannomas, which can occur including in the bulbar fibers and cranial nerves, as well as this juvenile posterior subcapsular cataract, which is uncommon to see sporadically but can be seen in this condition. 00:36 So let's first start with vestibular schwannomas. 00:38 How do they present? Well, there are tumors on the hearing nerve. 00:42 So patients present with hearing loss. 00:44 And this is sensory neural hearing loss. 00:46 We also see tinnitus, we can see imbalance. 00:49 Vertigo is actually very rare, though that vestibular cochlear nerve does carry information about balance. 00:57 Bilateral vestibular schwannomas are pathognomonic for this condition, and that's present in about 90% of patients, of NF2 patients at the time of diagnosis and should be present by age 30. 01:10 If a patient, an MRI, or a clinical vignette shows bilateral vestibular schwannomas that patient has NF2. 01:19 What do they look like? Well, here we see some of the brain findings on this coronal postcontrast imaging of the brain as well as the axial images on the top. 01:28 We also evaluate these patients and evaluate these vestibular schwannomas with audiometry. 01:33 Audiometry is a type of hearing test. 01:36 We look at how loud a tone has to be to hear it, and how many words you can hear out of 100. 01:42 Normal is 100%. 01:43 When patients get to hearing less than 70% that causes a problem with conversational speech. 01:49 It is an important indicator of symptomatic dysfunction from these tumors. 01:54 Here we see some of the tumors on imaging. 01:57 We see a right vestibular schwannoma and a left vestibular schwannoma. 02:01 Again, a right-sided vestibular schwannoma and a left-sided vestibular schwannoma. 02:05 And actually that tumor is closely approximated to a meningioma that may result in a collision tumor, two tumors colliding together, which can be particularly symptomatic. 02:15 Here we see an intracranial or cranial vault meningioma in this patient, and two bilateral vestibular schwannomas. 02:22 We see a lot of tumors in these patients. 02:24 And so all patients must get neuroimaging and audiometry at the time of diagnosis, and serially over time. 02:33 What about the intracranial meningiomas? What are those look like? And how are they different from sporadic meningiomas? Well here we see a couple of images, and a very important point. 02:43 Unlike classic sporadic meningiomas, which are the most common primary brain tumor. 02:49 Meningiomas in NF2 are often not discrete, single nodular lesions, but often diffusely involved the entire dura. 02:57 On the left with the red arrow we see a very small nodular meningioma, which is common to see sporadically. 03:03 And on the right we see Diffuse dural thickening. 03:07 Nodular lesions spread throughout the entirety of the dura, both in the frontal and occipital sides of the brain. 03:13 And this raises suspicion for a genetic and inherited syndrome like NF2. 03:18 NF2 meningiomas are often present with diffuse dural involvement. 03:22 And you can see that here on this imaging video. 03:25 We see that the entire dura is thickened and inflamed. 03:29 The white part of the brain that is enhancing with contrast, lighting up with gadolinium dye is diffusely thickened and enlarged. 03:37 And you can see that here, there's not just one meningioma or one nodule, the entire dura is involved in this tumor. 03:43 This makes these tumors very difficult to surgically remove and requires both a neurologist to evaluate which tumor is the problem, and which tumor should go after or a medical intervention to shrink them? What about the spinal cord lesions? In these patients we don't just focus on the brain, we have to look at the whole spine with spinal imaging. 04:04 Here we're looking at sagittal T2 or a stir image as well as a T2 weighted image to look at lesions that could be present in the spine. 04:12 And we see a T2 bright to hyperintense lesion behind the posterior aspect of the second cervical vertebrae or the C2 vertebrae. 04:21 This is a C2 lesion in the spinal cord. 04:24 Intermedullary enhancing tumors are common in patients with NF2. 04:29 And these are ependymomas, tumors that arise from those ependymal cells that line the junction between the brain and the ventricle. 04:36 When present, they're often multiple in about 58% of patients. 04:40 And they're common in this region. 04:42 the cervicomedullary junction or in the thoracic spinal cord. 04:47 They enhanced with contrast and so here you can see in this gadolinium enhanced MRI, very subtle enhancement or lighting up with the gadolinium contrast that's indicative of an active tumor process. 04:58 But the natural history is different from sporadic ependymomas, which are often quite severe, and it can be very aggressive. 05:05 In contrast, patients with NF2 often have a very benign natural history or clinical course, the majority of patients are asymptomatic up to 76%. 05:13 And symptomatic progression is very rare. 05:16 These are tumors that are monitored serially over time and often do not require intervention. 05:23 There are other manifestations that we need to think about in these patients beside tumors in the brain, and spinal cord that should be in the back of our mind to evaluate in these patients, and to consider in a clinical vignette. 05:33 In the eyes we see posterior subcapsular cataracts, often early in age. 05:39 Typical age onset or adult onset cataracts are in the anterior part of the lens. 05:45 Whereas, these juvenile posterior subcapsular cataracts are in the posterior aspect of the lens, which is uncommon sporadically, and suggests an inherited condition like NF2. 05:58 Cranial neuropathy can be seen and should be evaluated in patients with NF2 and generalized neuropathy, either a polyneuropathy or other type of mononeuropathy can be seen in these patients as well.
About the Lecture
The lecture Neurofibromatosis Type 2: Clinical Presentation by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Other than MRI, which of the following tests is used to evaluate patients with neurofibromatosis type 2?
- Audiometry
- Nerve conduction studies
- Lumbar puncture
- Electromyography
- Ophthalmoscopy
Which of the following is commonly seen on imaging of the type of meningiomas associated with neurofibromatosis type 2?
- Diffuse dural involvement
- Discrete nodular dural involvement
- Cerebellar vermis involvement
- Cerebellar hemisphere involvement
- Cerebellopontine angle involvement
Which of the following eye findings might be seen in a patient with neurofibromatosis type 2?
- Cataracts
- Amblyopia
- Optic neuritis
- Glaucoma
- Uveitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |